1. Background
The ultimate goal of policymakers in any health system is to provide and improve the health of all people in order for them to be able to participate in social and economic activities (1). The Alma-Ata Conference in 1978 emphasized on taking preventive measures rather than treatment as one of the most important ways of providing and promoting health (2).
The outcome of the Alma-Ata Conference in 1978 was a 10-item declaration. The universal declaration defined the overall health objective for the world's population as achieving a level of health (i.e., physical, mental and social) by the year 2000 through which individuals can have a constructive socio-economic life, and the key to attaining this goal is primary health care (3, 4).
As defined by the World Health Organization, primary health care refers to the essential health care provided through scientific and practical means and technologies that are acceptable, accessible and cost-effective for the community and country at each stage of development. It should also be at the first level of contact of the society with the health system (5). Studies have shown that 75% - 85% of patients need primary care within a year; consultation with specialist doctors is necessary in only 10% - 12% of cases, and referral to higher levels of care is solely necessary for 5% of cases. Thus, the key to comprehensive health care is at the first level of contact and primary health care (6). It is worth mentioning that direct referral of patients to higher levels of service delivery would increase treatment costs (7).
However, most studies conducted on the Iranian primary health care system showed that, despite having numerous achievements, it had notable weaknesses. Nekoei Moghadam et al. referred to the weakness of the system in urban areas and the existence of several centers with different providers (8). In its report on the Iranian health system in 2007, the World Bank highlighted many of the Iranian health system achievements after the expansion of health networks, and then mentioned some of the existing problems, including the multiplicity of service delivery systems and fragmentation of the health system, especially in cities (9). The results of these health system failures are increased costs of treatment and a large number of preventable deaths and disabilities in the country (7, 10). One of the important areas for improving the existing deficiencies is to review consumer decisions about the time, place and ways of seeking health services (11). Undoubtedly, various groups have different patterns of health care demand (12) because the factors affecting the need and demand for health services vary in different groups. These factors consist of demographic characteristics, gender distribution, age pyramid, the prevalence of diseases, health policies, gross national product and per capita income, the process of medical knowledge and technology development and cultural characteristics of the society (11).
Given the important role of timely use of primary health care by individuals for opportune diagnosis and control of disease costs and, eventually, the progression of recovery, knowing about individuals’ behaviors at the first step of health-seeking behavior can be of great help to managers and health care providers for making decisions. Therefore, we examined the utilization pattern of primary health care services in the households living in Shiraz, Iran, during 2016 - 2017.
2. Methods
This cross-sectional study was carried out during 2016 - 2017. The study population consisted of the households living in the 10 municipal districts and rural district of Shiraz. The sample size was calculated according to the results of a pilot study. In the pilot study, the mean scores of adherence to the referral system in men and women were respectively 2.63 ± 0.78 and 2.41 ± 0.87. According to the sample size formula in the two independent societies:
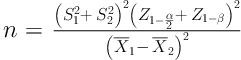
and 0.05 error, test power of 80% and potential attrition of 10%, the final sample size was calculated at 500 households.
In this study, a multi-stage sampling method was used for data collection, that is, using the stratified sampling method with proportional allocation, we determined the size of each class (10 municipal districts as well as the rural one). In the second stage, the cluster sampling method was used. Through this sampling method, each municipal district was classified into smaller areas based on the boulevards or streets of that district. The researcher selected 20% of the total number of boulevards or streets of each district through lottery, and then the households to be studied were equally selected from each selected street using random sampling. In so doing, after going to any street, we started from a residential building, and regarding the number of the houses, one out of 10 houses was selected through lottery, and a family member who was over 18 years of age and well-informed was interviewed. If a selected household was not inclined to respond or the informed family member was not present, the next-door house on the right was selected for the interview.
The data collection tool was a researcher-made questionnaire. To design the questionnaire, a combination of the tools used in the studies by Shabila et al. (13), El Kahi et al. (14) and Rasoulynezhad et al. (6) was used. To assess the content validity of the questionnaire, the expert panel method was applied. To examine the structural validity and reliability of the questionnaire, a pilot study with a sample size of 200 households was performed. The results of exploratory factor analysis to determine the structural validity of the third part of the questionnaire revealed two factors that, due to factor loading and design logic, were named adherence to reference system and perception of service quality. These two factors account for 62.8% of the variance. Also, the Kaiser-Meyer-Olkin measure of sampling adequacy was 0.74. This indicates that the correlation between the data for the analysis of the factor is appropriate and the Bartlett’s test of sphericity was 0.00, which indicates that the data analysis factor is significant. The Cronbach’s alpha coefficient of the questionnaire was obtained to be 0.747 using SPSS, version 22.
The questionnaire used in this study comprised three sections; the first section was about the individual and the second one was on household information. These sections include demographic and socio-economic variables, the first decision made by the individual and household for primary health care and barriers to accessing the services of the formal service provider. Most of the questions in these sections were in the form of checklists. The third section of the questionnaire, which was taken directly from the study of Shabila et al. (13). Due to the fact that the minimum factor loading accepted for each variable was 0.3, 7 out of the 10 questions of the third part of the questionnaire remained in two main dimensions, namely adherence to the referral system and the perception of the quality of primary health care services. Three questions were also deleted due to factor loading of less than 0.3. As in the case of the tool used by Shabila et al. (13), the Likert scale was used for answering the questions of this section and the options were: always (5 scores), most often (4 scores), sometimes (3 scores), rarely (2 scores) and never (1 score). The collected data were entered into SPSS version 22 and analyzed using descriptive and inferential statistics. Some tables were used to describe the data. Chi-square, Fisher’s exact test, independent samples t-test, one-way analysis of variance (ANOVA) and Pearson correlation coefficient were used for data analysis.
This study was approved by the ethics committee of Shiraz University of Medical Sciences. All the participants signed an informed consent form and the questionnaires were anonymous.
3. Results
Our results showed that 52.4% of the subjects were female, 65.6% were married and 34.4% had academic education. Furthermore, 95% were under the coverage of a health insurance, of which 64.4% had social security insurance. The mean age of the participants was 39.08 years. In terms of socio-economic characteristics, 52.4% owned a house and 56.6% were in the income group of 10 - 20 million Rials. The average household size was 3.86, and 41.8%, 49.6% and 32.8% of the households had elderly member(s), hypertensive patient(s) and diabetic member(s), respectively. Only 31.2% of the participants said they had required consultation on high-risk behaviors. Table 1 presents the frequency of people according to the first decision made when they needed first-level health services.
| First-Level Services | Refer to Family Physicians | Refer to a Specialist Physician | Refer to Health Houses/Health Posts/Health Centers | Self-Treatment | Refer to Traditional Therapists | Not Seeking any Special Treatment/Advice | Other Decisions |
|---|---|---|---|---|---|---|---|
| During simple illnesses | 44.6 | 0.8 | 0.8 | 26.8 | 8.6 | 6.6 | 11.8 |
| Nutritional counseling, weight control and pharmaceutical supplements | 18.6 | 21.4 | 4.8 | 16.2 | 2.6 | 27.8 | 8.6 |
| Psychological services | 6.4 | 42.4 | 3.4 | 4.8 | 0.6 | 38 | 4.4 |
| Consultations on high-risk behaviors | 23.7 | 30.8 | 12.2 | 2.6 | 0 | 9 | 21.7 |
| Care for diabetic patients | 32.9 | 37.8 | 2.4 | 4.3 | 0 | 1.8 | 20.8 |
| Care of the elderly | 45 | 23.4 | 3.8 | 0.5 | 0 | 6.2 | 21.1 |
| Care of hypertensive patients | 40.7 | 21.4 | 5.2 | 12.9 | 0 | 0 | 19.8 |
aValues are presented as percentage.
The majority of the participants stated that not taking the problem seriously was the most important reason for not seeking formal health services in case of simple illnesses (40.7%), counseling for high-risk behaviors (50%), elderly care (28.6%), hypertensive care (57.1%) and diabetes care (70%). Most of the subjects in terms of nutritional counseling (37.1%) and psychological services (35.5%) stated that the most important reason for not using formal care services was economic problems.
The results showed that age (P = 0.001), educational level (P = 0.003), residence (P = 0.001), household income (P = 0.001), health insurance (P = 0.000), type of insurance (P = 0.000) and type of referral system (P = 0.004) had a significant relationship with the first decision made when facing simple illnesses. People with a lower mean age had more referrals to a specialist physician. Non-use of the services provided by the formal sector was higher among under-diplomas, people with lower incomes and residents of villages. Referral to non-family general physicians was higher among the households with higher incomes. Not using the services provided by the formal sector was more common among uninsured people than insured ones, and among rural insurants than others. It was also higher when the referral system was mandatory compared to when it was optional.
The factors such as educational level (P = 0.000), marital status (P = 0.003), place of residence (P = 0.001), household income (P = 0.001), health insurance (P = 0.001), type of insurance (P = 0.001), referral system (P = 0.004) and health status (P = 0.028) had a significant relationship with the first decision made on nutritional counseling, weight control and the need for pharmaceutical supplements. Referral to a specialist was more common among the people with academic education. Not seeking any treatment or advice was higher among under-diplomas. Married people referred to health houses/centers and family doctors more than single individuals and those without spouses. Referrals to specialists were more common among higher-income participants. Non-use of formal sector services was higher among the uninsured subjects, while referring to a specialist was more common among those insured by the armed forces. As the referral system got optional, referrals to specialists increased. Those who had a poorer health status sought less treatment or physician advice.
The factors such as gender (P = 0.035), educational level (P = 0.000), residence (P = 0.000), household income (P = 0.000), health insurance (P = 0.001), type of insurance (P = 0.000), referral system (P = 0.048) and health status (P = 0.000) had a significant association with the first decision made in terms of psychological services. Non-use of the services was higher among men than women and in rural areas than in urban ones. The subjects with academic education used expert services more than others. The lack of specific action was higher among lower-income groups and referral to a specialist was higher among higher-income subjects. The lack of action was higher among non-insured people and those with a rural insurance and when the referral system was optional. Not using health services was observed more frequently among the people with poor health status.
The factors such as residence (P = 0.000), family income (P = 0.000), health insurance (P = 0.002), type of insurance (P = 0.000), referral system (P = 0.013) and health status (P = 0.028) were significantly related to the first decision made about counseling for high-risk behaviors. Residents of villages often went to health houses, but urban residents usually referred to specialists. As the income increased, referral to specialist doctors increased as well. Not seeking advice was more common among uninsured people. Referral to specialist doctors was higher among those insured by the armed forces. Not seeking any advice and self-treatment were more common when the referral system was optional. Non-use of the services provided by the formal sector was greater among those who had a poorer health status.
The factors including income (P = 0.028), the closest center to the place of residence (P = 0.000) and place of residence (P = 0.001) had a significant relationship with the first decision made for the elderly care. Those with higher incomes had more referrals to specialist physicians. Residents of cities initially preferred family doctors and then specialists. Rural residents initially preferred rural health houses and then family physicians.
Income (P = 0.000), the closest center to the place of residence (P = 0.000) and place of residence (P = 0.001) had an impact on the first decision made about care for patients with hypertension. Self-treatment was more frequently noted among those with lower incomes, and referring to specialists was more common among higher-income groups. Residents of cities had often selected family physicians first, and then visited specialist doctors. Residents of villages, on the other hand, had often chosen health houses and then family physicians.
The factors such as the closest center to the household residence (P = 0.001) and place of residence (P = 0.000) had a significant relationship with the first decision made about taking care of diabetic patients. Residents of cities had the most frequent referrals to specialist physicians and then to family physician, while residents of villages mostly referred to health houses and specialists.
Regarding care for the elderly, as well as patients with hypertension and diabetes, most people preferred the closest center to the place of residence for receiving health services.
The factors of age (P = 0.04), gender (P = 0.013), place of residence (P = 0.008) and marital status (P = 0.011) had a significant impact on the perception of the quality of first-level services. There was a significant positive relationship between age and perception of the quality of first-level services. Women estimated the quality of services higher than what men did, and single participants estimated the quality of services lower compared to married ones and those without a spouse. Further, rural residents appraised the quality of services higher than the residents of cities.
The factors of place of residence (P = 0.000), marital status (P = 0.008), educational level (P = 0.000), income (P = 0.000), type of referral system (P = 0.000), type of insurance (P = 0.001) and health status (P = 0.000) had a significant relationship with adherence to the referral system.
Those with under diploma education adhered more to the referral system than the subjects who had a diploma, and those with a diploma adhered to it more than those with academic education. Moreover, married people adhered to the referral system more than those without a spouse, and those without a spouse adhered to the referral system more than single ones. Villagers adhered to the referral system more than urban residents. Income had a converse relationship with adherence to the referral system. The highest adherence to the referral system was observed among insured rural residents. Those with a poorer health status were more likely to adhere to the referral system. Adherence to the referral system was more frequent when the system was mandatory.
Table 2 exhibits the significant relationship of gender and residence with the perception of the quality of first-level health services. It also shows that according to the one-way ANOVA, there was a significant link between marital status and the perception of service quality. However, it does not indicate a significant relationship between having health insurance and the type of referral system with the perception of the quality of first-level services according to the independent samples t-test. Moreover, the type of insurance, health status, educational level and income were not significantly associated with the perception of the quality of first-level services according to one-way ANOVA.
| Variable | Mean | Standard Deviation | Test Satistic | Significance |
|---|---|---|---|---|
| Gender | -2.501 | 0.013 | ||
| Male | 3.41 | 0.88 | ||
| Female | 3.65 | 0.86 | ||
| Educational level | 2.84 | 0.06 | ||
| Under-diploma | 3.69 | 0.808 | ||
| Diploma | 3.42 | 0.99 | ||
| Academic | 3.48 | 0.827 | ||
| Marital status | 4.601 | 0.011 | ||
| Single | 3.27 | 0.919 | ||
| Married | 3.6 | 0.84 | ||
| Without spouse | 3.68 | 0.9 | ||
| Income | 1.433 | 0.233 | ||
| Lower than 1 million Tomans | 3.45 | 0.87 | ||
| 1 to 2 million Tomans | 3.5 | 0.86 | ||
| 2 to 4 million Tomans | 3.71 | 0.91 | ||
| Higher than 4 million Tomans | 3.2 | 0.55 | ||
| Residence | -2.66 | 0.008 | ||
| City | 3.49 | 0.87 | ||
| Village | 3.92 | 0.85 | ||
| Health insurance | -0.502 | 0.616 | ||
| Yes | 3.53 | 0.87 | ||
| No | 3.73 | 1.29 | ||
| Type of insurance | 1.77 | 0.151 | ||
| Social security | 3.48 | 0.84 | ||
| Health insurance | 3.69 | 0.95 | ||
| Armed forces | 2.66 | 0 | ||
| Rural | 3.58 | 0.9 | ||
| Referral system | -0.325 | 0.746 | ||
| Mandatory | 3.52 | 0.89 | ||
| Optional | 3.56 | 0.83 | ||
| Health status | 0.906 | 0.461 | ||
| Very poor | 3.21 | 1.11 | ||
| Poor | 3.59 | 0.88 | ||
| Average | 3.63 | 0.87 | ||
| Good | 3.53 | 0.82 | ||
| Excellent | 3.45 | 0.98 |
Table 3 demonstrates the significant relationship of place of residence and the type of referral system with adherence to the referral system according to the independent samples t-test. Furthermore, one-way ANOVA reflected a significant relationship between adherence to the referral system and marital status, educational level, income, type of insurance and health status. Nonetheless, according to the independent samples t-test, the relationship of gender and having health insurance with adherence to the referral system was not significant.
| Variable | Mean | Standard Deviation | Test Statistic | Significance |
|---|---|---|---|---|
| Gender | 0.832 | 0.406 | ||
| Male | 2.84 | 1.04 | ||
| Female | 2.75 | 1.19 | ||
| Educational level | 10.86 | < 0.001 | ||
| Under-diploma | 3.15 | 0.95 | ||
| Diploma | 2.64 | 1.18 | ||
| Academic | 2.59 | 1.13 | ||
| Marital status | 4.878 | 0.008 | ||
| Single | 2.51 | 1 | ||
| Married | 2.91 | 1.15 | ||
| Without spouse | 2.66 | 1.05 | ||
| Income | 12.307 | < 0.001 | ||
| Lower than 1 million Tomans | 3.29 | 0.93 | ||
| 1 to 2 million Tomans | 2.87 | 1.12 | ||
| 2 to 4 million Tomans | 2.35 | 1.05 | ||
| Higher than 4 million Tomans | 2 | 0.9 | ||
| Residence | -7.45 | < 0.001 | ||
| City | 2.69 | 1.09 | ||
| Village | 3.8 | 0.85 | ||
| Health insurance | -1.056 | 0.291 | ||
| Yes | 2.79 | 1.12 | ||
| No | 3.27 | 1.02 | ||
| Type of insurance | 5.72 | 0.001 | ||
| Social security | 2.76 | 1.11 | ||
| Health insurance | 2.84 | 1.13 | ||
| Armed forces | 1.54 | 0.58 | ||
| Rural | 3.54 | 0.87 | ||
| Referral system | 16.31 | < 0.001 | ||
| Mandatory | 3.26 | 0.99 | ||
| Optional | 1.87 | 0.71 | ||
| Health status | 6.645 | < 0.001 | ||
| Very poor | 2.98 | 0.62 | ||
| Poor | 3.33 | 1.11 | ||
| Average | 3.1 | 1.07 | ||
| Good | 2.61 | 1.12 | ||
| Excellent | 2.51 | 1.1 |
4. Discussion
The results of this study showed that in half of the first-level health services, including psychology, counseling for high-risk behaviors and diabetes care, the first decision made by most of the individuals was to refer to specialist physicians, which indicated an inappropriate health-seeking behavior. The results of the studies by Musah and Toyin Kayode in Nigeria (15), Van der Hoeven et al. in Africa (16), Pourreza et al. in Tehran, Iran (17), Borhaninejad et al. in Kerman, Iran (18), Ebadi Fard Azar et al. in Isfahan, Iran (11) and Rasoulynezhad et al. in Kashan, Iran (6), which showed that the most frequent referrals were to specialist physicians, confirm the findings of our study.
But what is the reason for the preference for referring to specialist doctors? Borhaninejad et al. found that higher quality of services and greater trust were the reasons for more referrals to specialist doctors (18). Some individuals studied by Van der Hoeven et al. described the reasons for referring to more specialist levels as follows: “because I was not good at all,” and some others said: “Health clinic services are convenient for monthly care of non-communicable diseases such as hypertension” (16).
In the present study, the mean score of perceived quality of first-level services given to health houses/health posts/family physician posts was 3.45 out of 5, which was relatively good, but the lowest quality score was related to the staff manner dimension. Another reason for unnecessary referrals to specialists was the public view; that is to say, health houses/health posts were only suitable for vaccination, and family physicians were only suitable for simple illnesses such as a cold. Indeed, this view is affected by the structure of the health service supply system because health centers and health posts in urban areas are currently abandoned in the network system. The lack of attention of authorities reduces the credit of these centers (19). In villages, local educated forces (Behvarz) have been trained for health houses, but there are no similar forces in cities (9).
On the other hand, the family physician program being executed cannot be called a real family doctor program since one of the most important duties of family physicians is to provide basic health care services, but in this program, no separate and explicit definition has been provided for the health care of target groups, and referrals to family doctors are so numerous that they fail to accomplish their main duties, that is, monitoring and promoting health (20). Meanwhile, confused people are looking for a quality service center for their health needs, and they will ultimately refer to specialists or subspecialists on the basis of their own discretion. To address this, the opinions of the service recipients should be taken into account during the delivery of the first-level services, and even better evaluation of services by the public should be made. Damari et al. believe that patients who are satisfied with the services will not tend to circumvent the referral system. Thus, health centers should be rich in personnel, well-equipped and sufficiently accessible to people at appropriate times throughout the day (20).
In our study, the first decision made by most people was to not seek specific health services in terms of nutritional counseling. The results of the study by Olasunbor et al. on nutritional health-seeking behavior in Nigeria showed that 85.2% of the subjects had visited a health care center at least once within the previous month (21). This was not consistent with the results of the present study. The results of our study in terms of receiving services in case of simple illnesses, as well as care for the elderly and patients with hypertension, showed that the first decision of most people was to refer to the family physician’s office, which is indicative of an appropriate health-seeking behavior.
However, regarding these services, the respondents stated that they had not received the services in the form of continuous and comprehensive health care, and only in the event of a disease their first decision was to refer to the family physician's post. The study by Borhaninejad et al. on utilizing health care services by the elderly in Kerman, Iran, showed that specialist doctors had the highest number of visits (18), which was not consistent with our study results in terms of the first decision about elderly care. It seems that the family physician plan in Shiraz, Iran, has been able to provide an appropriate coverage for the elderly to receive care services.
A survey by Bovet et al. on health care utilization for hypertensive patients in Tanzania showed that 63% of the people used public health centers (22). These results were consistent with those of our study in terms of the fact that the participants had referred to the same first-level services.
As far as counseling for high-risk behaviors is concerned, the important point was that nearly 70% of the individuals said they never needed to receive such services. Perhaps, people’s lack of awareness about diseases like AIDS and hepatitis, as well as their feeling about incurability of these diseases may cause social stigma to those in need of such services, and this leads to lack of referral to the service centers, or even if they refer, they will hide their referrals. In terms of counseling for nutrition and psychology, the majority of people who had not used the services provided by the formal sector said the reason for their non-referral was economic problems.
Economic resources are among the empowering factors of the Andersen model and the factors needed for enabling people to access health care services. One way to receive these services is to subsidize low-income people by the government. However, community health centers offer services such as nutritional and psychology counseling free of charge to those referred by family physicians, but the information about the delivery services was so poor that almost nobody knew about such health care services.
Findings showed that in more of the first-level services, including simple illnesses, counseling for high-risk behaviors, elderly care and hypertension and diabetes patients, the major reason for not using formal services was that these problems were not taken seriously. Regarding preventive and screening services, unlike health care or rehabilitation services, since the illness or disability has not appeared yet, people do not consider receiving care seriously, and this is the time when educating and directing the attention of the individuals toward health issues seems necessary (23).
In many studies such as those by Borhaninejad et al. in Kerman, Iran (18), Pourreza et al. in Tehran, Iran (17), Danso-Appiah et al. in Ghana (24) and Kolola et al. in Ethiopia (25), people stated that their lack of referral to receive health care services despite having illnesses was due to the unimportance of their illnesses and economic problems. However, Kavosi et al. did not show any inequality in the actual amount of outpatient service utilization in Shiraz, Iran (26).
The family physician program in Fars province was implemented in July 2012. Prior to March 2017, referrals to specialists had to be made only through a family physician referral form, but since then, due to pressures on policy makers, referrals to specialists became possible outside of the referral system and without referring to the family physician, but with a little higher charge. Since the referral system became non-mandatory during conducting this study, a comparison was also made with regard to the impact of mandatory referrals on households’ decisions. Findings showed that the mean score of adherence to the referral system by the subjects under study at time of mandatory referral system was higher than their score at the time of optional referral system. The mandatory referral system was one of the control mechanisms that prevented the direct referral of patients to specialists in order to strengthen the first level of contact, and when the referral system became optional the mean score of adherence to it declined.
The results of this study revealed that in case of simple illnesses, the factors such as age, educational level, place of residence, household income, having health insurance, type of health insurance and mandatory or optional referral system influenced the use of services, but the factors such as gender, marital status, and health status did not play any roles in the use of services. The study by Kuuire et al. on health-seeking behaviors during illnesses showed that age, health status and educational were effective on individuals’ behaviors (27). The results of their study were not consistent with those of our study in terms of the impact of health status.
In our study, nutritional counseling was influenced by educational level, marital status, household income, household residence, health insurance, type of insurance, health status and referral system. However, receiving these services had no significant relationship with gender and age. The results of the study by Olasunbor et al. in Nigeria, which was conducted on nutritional health-seeking behavior in Nigerian, indicated that gender, age, educational level and income had an impact on the health-seeking behavior in terms of nutrition (21). Quinn et al. in Georgia, US, showed that age, income and gender affected the nutritional health-seeking behavior (28). The results of their study were not consistent with those of our study in terms of the impact of age and gender.
The results of the present study presented that using psychological services had a significant relationship with gender, educational level, income, residence, having health insurance, type of health insurance, health status and referral system. However, psychological services had no significant relationship with marital status and age. In a study on the factors affecting the use of Canadian mental health services, Fleury et al. found that gender and income had an impact on the use of psychological services (29). The results of their study were consistent with those of our study.
The results of our study showed a significant relationship between counseling about high-risk behaviors and income, residence, having health insurance, type of health insurance, health status and referral system, but no significant link was noted between counseling about high-risk behaviors with gender, educational level, marital status and age.
The results of this study showed that educational level, marital status, income, residence, type of insurance, health status and type of referral system played a determining role in adherence to the referral system, but factors such as gender, age and having health insurance did not affect the referral system.
According to the results of this study, the factors including gender, marital status, age and residence played a determining role in the perceived quality of primary health services, but educational level, income, having health insurance, type of health insurance, health status and type of referral system did not have any effects on the estimated quality of primary health care services. A study by Alibabaei et al. was conducted to determine the quality of family doctor team’s services from the viewpoint of the clients in Ajabshir showed that women had higher satisfaction with most items than men. The highest satisfaction was found among the 40 - 49 age group and the single people. There was no significant relationship between satisfaction and educational level (30). This finding was consistent with our results in terms of all items, except for the effect of marital status. The study by Fallahi et al. on the satisfaction of clients with family physicians in Jiroft, Iran, showed that gender and insurance did not affect the individuals’ satisfaction, but the people aged 45 - 60 years, married ones and those with low educational level had estimated the quality of the services higher (31). The results of that study, except for the two factors of gender and educational level, were consistent with those of the present study.
The results of our study showed a significant relationship between the use of elderly care and household income, the closest center to the household residence and residence, but there was no relationship with the current residential status and type of referral system. In the study by Park in Korea, income also influenced the use of elderly care services (32).
In the present study, receiving hypertension care had a relationship with income, the closest center to the household residence and the house location. However, hypertension care had no relationship with the current residential status and type of referral system. The results of the study by Bovet et al. showed that income did not affect the use of services by Tanzanian hypertensive patients (22), and it was not consistent with the results of our study. This inconsistency can be attributed to the time of study, study location, socio-cultural factors, demographic characteristics of the population studied, access of different communities to various locations and the quality of service provision. The results of the study by Ham and Lee on the use of health services by South Korean hypertensive patients also showed that the place of residence had an impact on the use of health services (33).
According to the findings of this study, regarding diabetes care, the closest center to the household’s residence and the place of residence had a relationship with using these services. Nonetheless, housing status, household income and type of referral system did not affect the first decision made for this kind of care. The study carried out by Inche Zainal Abidin et al. in Malaysia also indicated that the closest center to the place of residence had an impact on the treatment-seeking behavior of diabetes patients (34).
4.1. Conclusions
The demographic characteristics and attitudes of individuals towards the existing services have a significant effect on their willingness to reuse those services at the health care centers. Therefore, managers and policy-makers of the system should focus their efforts on providing desirable services and, consequently, changing the way households view the services and increasing their satisfaction with the existing services.