1. Background
A considerable controversy exists about the long head of the biceps (LHB) tendon roles and functions, but the majority of scientists agree that the function of LHB is in humeral head depression and its anterior stability (1, 2). Inflammatory tendinopathy in LHB tendon is one of the most common causes of shoulder pain that mainly induces weakness in forward flexion of the shoulder (2). Damage to this tendon can be categorized as tenosynovitis, tendinosis, or tendonitis and can be accurately diagnosed by biopsy (3). Similar to other inflammatory tendinopathies, the treatment of LHB tendinopathy includes conservation and surgical approaches. However, none of the methods are known to be the best, neither in non-surgical nor in surgical approaches (4-6).
The most widely used physiotherapeutic methods for the treatment of tendinopathies are low-level laser treatment (LLLT) and ultrasound (US) (2, 5, 7). The effectiveness of these two methods has been investigated in many studies. In recent years, the methods either in combination with exercise (8) or in combination with each other (9) as L/US have been used to reduce pain related to shoulder tendonitis. However, confirmed evidence on the effectiveness of these methods is not yet available (2, 3, 6). Peri-tendon corticosteroid injections are used in many tendinopathies such as De Quervain’s disease, tennis elbow, trigger finger, and plantar fasciitis. Contrary to the wide use of local injection of corticosteroids, a disagreement exists about their effectiveness in the treatment of LHB tendonitis (7, 10, 11). In addition, short-term and long-term effects in addition to the side effects of peri-tendon injections are controversial (7, 11).
In recent years, some studies have evaluated the accuracy of injection under the guidance of US in the treatment of LHB tendonitis (1, 12). Although the higher accuracy of injection under the guidance of US has been reported (13, 14), a few studies have compared the results of US-guided injection in the treatment of LHB tendonitis (15). Therefore, the aim of the present study was to compare the therapeutic effects of the four methods of US alone or in combination with LLLT (L/US), intra and extra sheath US-guided injection in the treatment of LHB tendonitis.
2. Methods
2.1. Ethical Statement
The protocol of the present study was registered after an approval was obtained from the institutional review board (IRB) of Guilan University of Medical Sciences with No. 7723. The present study was designed under the principles of the declaration of Helsinki and the findings were reported based on the CONSORT guidelines. Advantages and disadvantages of each therapeutic method were discussed with patients and written consent was obtained from all patients. The patients were informed that they could withdraw from the study at any time. The required sample size for the evaluation of the Constant-Murley score (CMS) index in four studied groups was determined based on Otadi et al. (9) report. The used values were 95% confidence and 80% power in the two-way analysis of variance (ANOVA), and the lowest number of persons in each group was set at 32. The sampling was done in all groups to reach an appropriate sample size. Eligible patients were randomly divided into one of the four treatment groups by using a random block method of 8 patients in each block. Patient randomization was performed based on the ethical standards of Helsinki and the consolidated standards of reporting trials (CONSORT) statement.
2.2. Patients and Settings
From January 2014 to January 2015, patients with confirmed LHB tendonitis who referred to the orthopedic clinic of an academic tertiary referral hospital were enrolled in a four-group parallel-randomized clinical trial (RCT) to evaluate the therapeutic results of four methods of treatment. These methods included US alone (US), combined LLT and US (L/US), intra sheath corticosteroid injection (InCI), and extra sheath corticosteroid injection (ExCI). Our inclusion criteria were an age between 22 and 60 years, the pain history of shoulder or forelimb that continued for more than 3 months, local tenderness in bicipital groove, at least one biceps positive test (Yergason’s test or speed test), positive LHB tendonitis signs in IMRA (indirect magnetic resonance arthrography), and lack of any evidence about complete or incomplete rapture of rotator cuff. Patients with a history of trauma, injection or surgery in the affected shoulder, any calcification (or calcareous deposit) in the rotator cuff, any sign of concomitant shoulder pathology in IMRA, and any signs of partial or complete dislocations or raptures of LHB tendon were excluded from the study. Patient’s eligibility assessment was performed by the senior author and all patients were treated at the same center.
2.3. Interventions
The following interventions were applied to the groups:
- US group: 10 sessions of US (three per week, Sonopuls 492, Enraf-Nonius, The Netherlands) with a frequency of 1 MHz and intensity of 1 W/cm2 by the pulse mode duty cycle of 2:8 and the probe surface of 5 cm2 were applied for 5 minutes in each section (9).
- L/US: In this program, the type and frequency of US were similar to those of the previous group. In addition, LLLT was performed using a gallium-arsenide-aluminum infrared laser (830 nm wavelength, 30 mW power, 1 J/cm2 intensity, 4 mm ray diameter, and 2.5° angle of divergence) 9 with a pencil probe (EndoLaser 422, Enraf-Nonius, The Netherlands).
- InCI: In the supine position, forelimb of the injection site was bent as 90° from the elbow and it was put on the body. The injection site was disinfected by povidone-iodine solution and covered by a sterile drape. The US probe (Ultrasonix Touch ver.5.5.4 model) was covered by the sterile cover and the sterile gel was also used. With the help of the linear probe at a range of 2 - 20 MHz and based on the depth of anatomical structure, LHB tendon was found in bicipital groove. 1 mL of 40 mg/mL methylprednisolone acetate solution and 1 mL of 2% lidocaine solution were mixed together and intra tendon sheath injection under US guidance by 1.5-inch length gauge 25-needle was applied (15).
- ExCI: All steps and equipment were similar to those for InCI with a difference being that extra tendon sheath injection of the solution was applied.
All injections were performed by an expert radiologist in musculoskeletal interventions and all physiotherapy sessions were performed by one physiotherapist with 11 years’ experience.
2.4. Outcome Measurements and Follow Up
Demographic characteristics such as age, gender, history of diabetes mellitus (DM), the affected side, and level of hand and shoulder use in job or exercise were obtained. Patient’s evaluations were performed by an orthopedist who was blinded to the treatment methods at five times of before intervention, one week, one month, three months, and one year after the treatment. As the primary outcome, pain intensity was evaluated at all five visits using visual analogue scale (VAS) from 0 (no pain) to 10 (intolerable pain). The secondary outcome was CMS. Similar recommendations for exercise and after treatment were presented to all patients. If the patients’ symptoms were not recovered in one month or the symptoms recurred, similar treatment approaches were applied for a maximum of three times.
2.5. Statistical Analysis
Data are presented as mean ± standard deviation (SD) for quantitative variables and frequency and percentage for qualitative variables. One-way analysis of variance (ANOVA) with Tukey as Post hoc test and Chi-square test were used for finding statistically significant differences when P < 0.05.
3. Results
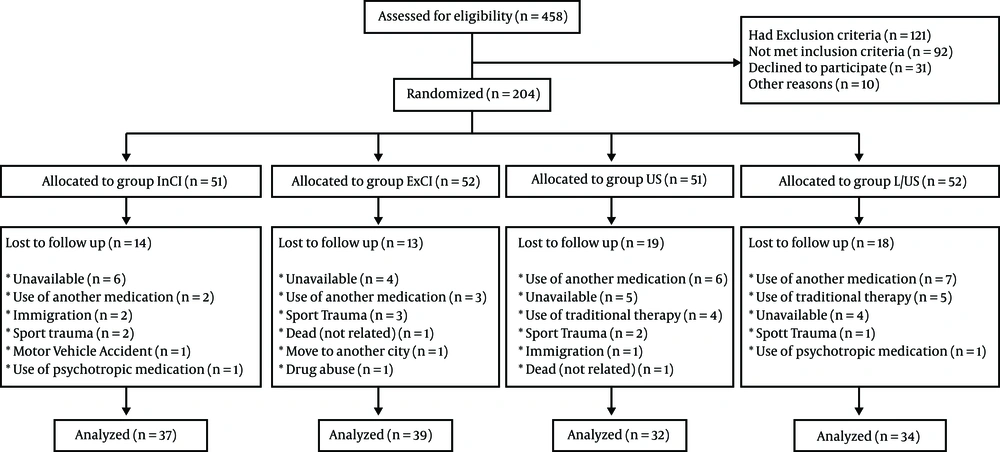
Totally, 204 patients were included and at the end of one year, the follow-up of 142 cases was done (Figure 1).
No significant differences existed in demographic information between the four groups (Table 1).
| Variables | Evaluated Groups | ||||
|---|---|---|---|---|---|
| InCI | ExCI | L/US | US | P Value | |
| Age, y | 40.1 ± 8.9 | 40.9 ± 6.9 | 38.4 ± 8.3 | 38.1 ± 7 | 0.355b |
| Female | 22 (59.5) | 22 (56.4) | 23 (67.6) | 16 (50) | 0.530 |
| Right side | 27 (73) | 32 (82.1) | 26 (76.5) | 22 (68.8) | 0.609 |
| Dominant hand | 24 (64.9) | 25 (64.1) | 23 (67.6) | 21 (65.6) | 0.991 |
| Diabetes mellitus | 7 (18.9) | 8 (20.5) | 9 (26.5) | 7 (21.9) | 0.887 |
| Intensity of activity | 0.762 | ||||
| Low | 4 (10.8) | 3 (7.7) | 2 (5.9) | 5 (15.6) | |
| Moderate | 26 (70.3) | 27 (69.2) | 25 (73.5) | 18 (56.3) | |
| High | 7 (18.9) | 9 (23.1) | 7 (20.6) | 9 (28.1) | |
aValues are expressed as mean ± SD or No. (%).
bBetween-groups analysis was performed using one-way ANOVA for age and chi-square test for other variables.
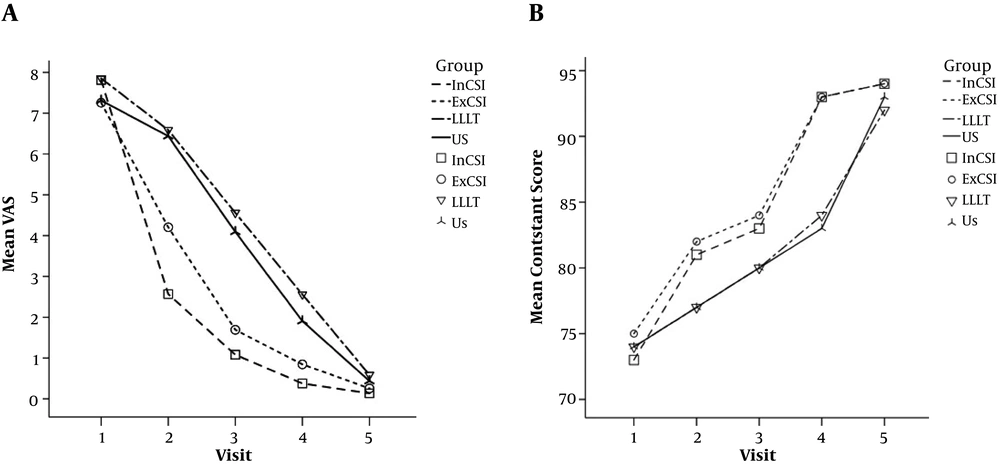
No statistically significant differences were detected in pain intensity based on the VAS score (P = 0.076) and shoulder function based on CMS score (P = 0.076) before treatment between the four groups. However, significant differences in all visits in VAS and CMS scores existed between the four groups after the treatment (Figure 2).
VAS and CMS scores were improved after treatment in all four groups and at all visits in comparison with before treatment (P < 0.001). The greatest decline in the VAS score and the highest increase in the CMS score were seen in the InCI group. The VAS score at the second visit was lower in the InCI group than in all other groups (P < 0.001). This difference was not significant at the third and fourth visits between the InCI and ExCI groups (P > 0.05) while the InCI group had a significant difference with the US and L/US groups in the VAS score (P < 0.001). At the fifth visit, the VAS score in the InCI group was not significantly different from those of the ExCI and L/US groups (P = 0.759 and P = 0.096, respectively) while it was only significantly different from the score of the US group (P = 0.003). Shoulder function based on CMS was similar at all visits between both injection groups. Nevertheless, at the second and fourth visits, significant differences were seen between the injection groups and the two other non-injection groups. At the fourth visit, CMS difference between the InCI and US groups remained significant (P = 0.012) but this difference was not observed between the InCI and L/US groups (P = 0.43). At the fifth visit, CMS differences between the InCI group and ExCI and L/US groups were not significant (P = 0.056 and P = 0.101, respectively) but significant in comparison with the US group (P < 0.001). The mean VAS decrease before treatment compared to one year after treatment in the InCI and ExCI groups was 7.7 ± 1.1 and 7 ± 1.3, respectively. Moreover, the mean CMS improvement within 1 year after treatment in the InCI group was 21.4 ± 5.5 and in the ExCI group was 18.6 ± 4.7.
Overall, the slope showing the improvement of VAS and CMS scores was steeper in both InCI and ExCI groups than in the other two groups (P < 0.001) but this difference was not significant. The differences in VAS and CMS scores between the US and L/US groups were not significant at any of the visits (P > 0.05). Regardless of the treatment method, the level and trend of VAS reduction and CMS increase in all patients had no significant relationships with DM and intensity of activity (P = 0.635 and P = 0.716 for VAS score and P = 0.111 and P = 0.762 for CMS score, respectively). Re-treatment need in the treatment groups was different (P < 0.001) and the InCI and ExCI groups with a mean of 1.03 ± 0.16 and 1.08 ± 0.27, respectively, had less need for re-treatment compared to the two groups of L/US and US with the mean of 1.41 ± 0.5 and 1.49 ± 0.6, respectively. The frequency of treatment also had no significant relationship with DM and intensity of activity (P = 0.091 and P = 0.953, respectively).
Two patients in the US group and one patient in the L/US group had symptoms after three treatment periods. Other therapeutic approaches were used for them and they were excluded from the study. None of the patients in both injection groups needed other treatment methods.
4. Discussion
In the present study, the pain relief and improvement of function based on VAS and CMS scores were compared between four therapeutic approaches of US, L/US, InCI, and ExCI in patients who suffered from LHB tendonitis. Our findings demonstrated that all four methods could decrease pain and increase shoulder function in patients with LHB tendonitis. Although the improvement trend was faster in the injection groups, after 1 year, the results of the injection methods and L/US were similar and the results of these three methods were better than the results of US alone. US guidance to some extent increases the accuracy of injection in LHB tendon and by reducing the possibility of injection into the tendon, vessels, and surrounding nerves, the adverse effects can be lessened (16). Our main aim in this study was to determine whether intra or extra tendon sheath injections affect the results or not. One week after treatment, pain intensity was significantly lower in the InCI group than in the other three groups. However, after 3 weeks, the difference between this group and the ExCI group disappeared. The range of changes was comparable with InCI in the study of Zhang and colleagues. They concluded that a higher accuracy of injection under US guidance could be the reason for better results in the guided group in comparison with the blinded group (15). Corticosteroid injection is one of the most effective and common applicable methods in the treatment of tendinopathies10 being used in many types of tendon inflammations and pathological conditions (17-20). On the other hand, the use of US technology in musculoskeletal interventions has gained more interest in recent years (1, 11, 12). Hashiuchi et al. (13) showed that injection under US guidance had higher accuracy against blinded injection. The lack of accuracy in blinded injection causes extra- or a combination of extra and intra tendon sheath injections. The most important reason for the use of US guidance in the treatment of LHB tendonitis is to confirm intra-sheath delivery. Nevertheless, based on the findings of this study, it seems that intra tendon sheath corticosteroid injection has no advantages over extra tendon sheath injection with regard to shoulder function. Although a more dramatic pain reduction was seen in a short time, the results quickly become similar to the results of extra sheath injection. It can be concluded that due to more-technical demand and the more expenses of intra tendon sheath injection, the freehand injection can be used in the treatment of LHB tendonitis except when a rapid pain decline is needed.
The use of any modalities in the treatment of shoulder pain is very applicable (8, 9, 21). In our study, the number of treatments was lower in the injection groups than in the physiotherapeutic groups. Although a significant difference existed between the injection methods with US and L/US at the second, third, and fourth visits, this difference between L/US and injection groups disappeared at the 1-year visit. However, this difference remained for the US group. In Otadi et al. study (9), the addition of LLLT to US could enhance the effects of US alone. Otadi et al. (9) study, similar to our study, confirmed the better effectiveness of L/US as compared to US. In addition, other studies reported that the use of US alone was not effective (22). Debates about the effectiveness of these methods are still ongoing but the result of our study showed that the concurrent use of LLLT and US produced better and more rapid results than the use of US alone. When the therapist does not have enough expertise in local injection, it is better to use L/US and not to use US alone in the treatment of LHB tendonitis.
Although the prevalence of tendonitis and tenosynovitis is higher in DM patients than in the normal population (23), the result of the present study showed that suffering from DM has no effects on the treatment trend of LHB tendonitis. Doctors always have concerns about complications such as infection and increasing blood sugar levels in DM patients after corticosteroid injection. As Stepan et al. (24) reported, the increase of FBS in the local injection is transient and has no effects on glycosylated hemoglobin. In addition, in Cervini et al. (16) study, the prevalence of infection in procedures under the guidance of US was very low (0.1%). In our study, not only were the signs of infection not seen, but also the results of diabetic and non-diabetic patients were similar. Due to the fact that the overuse of hand and repetitiveness in manual work and projectile sports are some of the main causes of LHB tendonitis (25), we aimed to evaluate the effects of intensity of activity on pain reliving trend and improved function in these patients. Although, due to the low power of the study, the effect of this factor in each group could not be evaluated separately, our results demonstrated that the intensity of activity has no effect on the trend of improvement.
This study suffers from some limitations. One of the limitations of this study is that due to the low number of DM and non-DM patients in each group, we evaluated all DM and none-DM patients together. Future studies must evaluate and compare the results of these methods only in DM patients. Another limitation was the lack of complete blindness of patients. To lessen this effect, the evaluating doctor was blinded to the therapeutic method. Finally, the concurrent existence of inflammatory diseases of the shoulder joint (arthritis or capsulitis) may be another limitation. Any of the therapeutic methods may be used to treat such diseases and this can interfere with results’ specificity. In addition, it is possible that patients used other drugs or traditional medicinal agents as arbitrary and secret.
4.1. Conclusions
Although intra sheath corticosteroid injection under US guidance is an effective method for the treatment of LHB tendonitis, especially in the 1st week after treatment, extra sheath injection also has acceptable results. L/US as a less invasive treatment could be as effective as corticosteroid injection in the long term.