1. Background
Overweight and obesity are major health problems worldwide. Obesity may lead to serious disorders such as musculoskeletal disabilities resulting in impaired quality of life (1-3). It has been also shown in some studies that weight gain and obesity are along with some postural disorders such as higher prevalence of knee valgus angle, thoracic kyphosis, and lumbar hyperlordosis compared to eutrophic ones (3-7). For this reason, lowering postural faults is expectable by lowering body weight via various supportive, medical or even invasive plans. In recent years, Bariatric surgery has been known as a popular method superior to conventional treatments among severely obese patients. The earliest reports on the effectiveness of surgery in the treatment of obesity refer to the fifth decade when the amelioration of obesity and its common related disorders such as diabetes mellitus were reported following subtotal gastrectomy (8). Later, the effectiveness of gastric bypass surgery on weight loss was indicated in combination with other treatment methods (9, 10). Further evidence for the long-term effectiveness and safety of bariatric surgery has continued to grow in the literature (11-14). Although the positive effect of weight loss by using ordinary methods such as diet and exercise on musculoskeletal pain has been shown (15, 16), the evidence approving the role of bariatric surgery on these disorders are limited. Longitudinal follow-up is advocated to reveal whether weight loss surgery reverses pain and physical functional limitations and improves the quality of life (17). Therefore, this study aimed to investigate the long-term effect of weight loss mediated by bariatric surgery on the disability from spinal pain and body postural disorders.
2. Methods
This survey was a present prospective interventional case series study approved by the Ethics Committee of Iran University of Medical Sciences (92-02-140-23111). Prior to the study, all subjects were asked to sign an informed consent form, which was approved by the Ethics Committee of Iran University of Medical Sciences.
The inclusion criteria included obese patients who were candidates for laparoscopic Roux-en-Y gastric bypass surgery, aged more than 30 years and body mass index (BMI) of at least 40 kg/m2. Those patients who were unwilling to perform the postural evaluation were excluded from the study. All eligible participants were planned to undergo Roux-en-Y gastric bypass surgery. The baseline information for the patients such as demographic data and medical history were collected by interview.
The body postural status was assessed using a plumb line in the anterior, posterior, and lateral views by a sports medicine specialist. The plumb line was a simple equipment at minimal cost (18). In a standing posture, a plumb line was used as the line of reference to represent a standard. Based on nature's law of gravity, it is a tool in the science of mechanics. The simple device of a plumb line enabled us to see the effects of the force of gravity. The plumb line test was used to determine whether the points of reference of the individual being tested were in the same alignment as the corresponding points in the standard posture. The deviations of the various points of reference from the plumb line revealed the extent to which the subject's alignment was faulty. The patients were asked to take off clothes (except underwear) and stand in the habitual posture they stand usually while looking at a point on the wall at the same level of their eyes. The plumb line was hung up from the roof in a small room with plaid walls. The patients stood in three positions; back to the plumb line, face to the line, and side to the line. In the side view, the plumb line represented a projection of the gravity line in the coronal plane that hypothetically divided the body into front and back sections of equal weight and the researcher observed deviations from the plumb line. In the back view, the plumb line represented a projection of the gravity line in the midsagittal plane. It was beginning midway between the heels; it extended upward midway between the lower extremities, through the midline of the pelvis, spine, sternum, and skull. The right and left halves of the skeletal structures were assessed symmetrically, and the counterbalance of the two halves of the body was observed. Evaluation in the anterior view was also similar to the back view. The posture of the head, neck, shoulders, thoracic and lumbar spine, pelvic and lower extremities were observed by the researcher in the three views. The plaid wall helped to evaluate the symmetry of the different parts of the body.
The data related to spinal pain were collected using the standardized neck disability index (NDI) and Roland-Morris questionnaires that are valid and reliable in Iran (19, 20).
The NDI is a patient-completed questionnaire with 10 items (the score of every question up to 5, for a total score of 50). The questions are about cervical pain during daily activities such as lifting, reading, headache, driving, sleeping, and recreation. The Roland-Morris is a 24-item self-report questionnaire assessing the functional abilities related to back and lumbar pain. The score of each question ranges from 0 (no disability) to 24 (the greatest disability).
All the parameters were assessed immediately before and 3, 6, and 12 months after the surgery. The patients went under the Roux-en-Y gastric bypass surgery at the same clinic by an expert surgeon with more than 10 years of experience in the bypass surgery. Two weeks after the surgery, they came to the clinic for visit. They were advocated to do the usual daily activities as similar as they do before the intervention. All patients underwent a diet of 300 kcal added to resting metabolic rate (RMR). All the patients were recommended to do aerobic and strengthening exercises regularly. Walking or running in a moderate intensity (50% - 70% of heart rate reserve) for 30 minutes on most days of a week was prescribed. Three sets of 15 repetitions of strength exercises in the upper and lower extremity muscles were prescribed twice a week. The upper extremity exercises included shrug, strengthening exercises of the deltoid, rotator cuff, biceps, and triceps muscles. In the lower extremity strengthening exercises of hip adductor and abductor, quadriceps and hamstring muscles were recommended. The patients were not being observed between the follow-ups.
The study endpoints included: 1) The amount of weight loss, 2) the difference in body posture status and 3) the amount of pain reduction.
For the statistical analysis, the statistical software SPSS version 16.0 (SPSS Inc., Chicago, IL) was used. The results were presented as the mean ± standard deviation (SD) for quantitative variables and were summarized by absolute frequencies and percentages for categorical variables. The trend of the changes in the parameters of weight and BMI was assessed using the repeated measure ANOVA test after being adjusted for baseline confounding factors. The difference between the different times of follow-ups compared to before intervention was analyzed by post hoc test (Turkey test). The non-parametric analysis (Friedman) was used for the NDI and Roland Morris comparing the changes during 1 year. Wilcoxon Signed Rank Test also was used for the pairwise comparing of the data. The P values of 0.05 or less were considered statistically significant.
3. Results
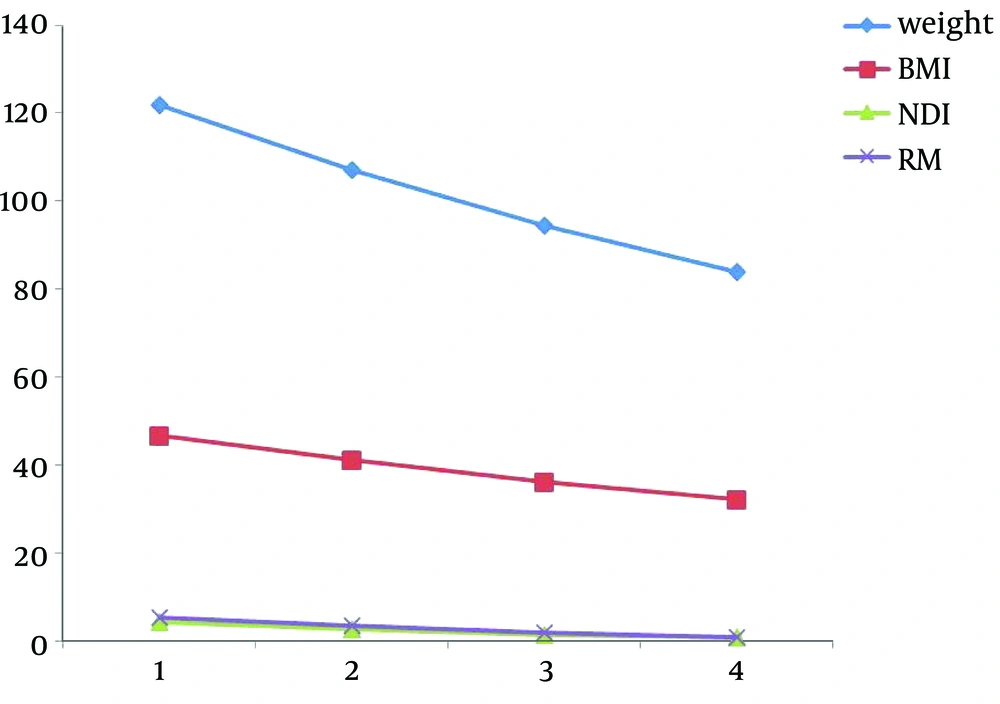
In total, 60 obese patients (58 women and 2 men) with the average age of 39.8 ± 8.5 years (ranged from 30 to 60 years) were assessed. The mean study parameters relating to spinal pain and disability before and after the intervention are summarized in Table 1. The mean and standard deviation (SD) of NDI score before surgery (4.28, 5.82) significantly reduced within 12 months of follow-up (0.75, 1.97) (P < 0.001). The Roland Morris mean score and SD considerably reduced during the 12 months after the intervention (0.90, 1.46) as compared to before (5.42, 5.55) (P < 0.001). Similarly, the mean weight and body mass index before surgery were 121.7 and 46.76, respectively, that decreased to 83.99 and 32.25 one year after the surgery (P < 0.001).
| Before Intervention | 3 Months Later | 6 Months Later | 12 Months Later | P Value | |
|---|---|---|---|---|---|
| Mean weight, kg | 121.73 ± 19.38 | 106.98 ± 18.40 | 94.47 ± 17.04 | 83.99 ± 15.51 | < 0.001 |
| Mean BMI, kg/m2 | 46.76 ± 6.19 | 41.08 ± 5.94 | 36.27 ± 5.51 | 32.25 ± 5.14 | < 0.001 |
| Mean NDI score | 4.28 ± 5.82 | 2.68 ± 3.89 | 1.38 ± 2.58 | 0.75 ± 1.97 | < 0.001 |
| Mean Roland-Morris score | 5.42 ± 5.55 | 3.33 ± 3.74 | 1.80 ± 2.35 | 0.90 ± 1.46 | < 0.001 |
The Change in Weight, Body Mass Index, and Musculoskeletal Pain and Disability Following Surgery for Obesity Treatment
The body posture deviations at different points before and after the surgery are also presented in Table 2. Of all the measured postural parameters, foot pronation significantly improved. For example, before the surgery, 78.3% of the obese people had foot hyperpronation while the rate decreased gradually after the surgery. As shown in Table 2, 48.3% of the patients had foot hyperpronation after one year. Anteroposterior pelvic tilt was also one of the postural faults that improved after the intervention as 21.7% of the patients had anteroposterior pelvic tilt before the surgery but 12 months after the intervention, only 3.3% had pelvic tilt. The rate of the subjects who had lumbar hyperlordosis decreased to 36.7% compared to before the intervention (61.7%). 41.7% of the patients had dropped shoulder in one side that decreased to 30% after the intervention. The rounded shoulder was 26.7% before the surgery that declined to 5% one year after the intervention. 33.7% of the patients had head lateral tilt that also significantly reduced within 12 months after the intervention to 15%.
| Before | 3 Months Later | 6 Months Later | 12 Months Later | |
|---|---|---|---|---|
| Foot pronation | 78.3 | 75.0 | 61.7 | 48.3 |
| Flat foot | 18.3 | 18.3 | 18.3 | 18.3 |
| Hyperextension of knee | 10.0 | 10.0 | 10.0 | 8.3 |
| Flexed knee | 11.7 | 10.0 | 10.0 | 10.0 |
| Bow legs | 5.0 | 5.0 | 5.0 | 5.0 |
| Knock knees | 8.3 | 8.3 | 8.3 | 8.3 |
| Anteroposterior pelvic tilt | 21.7 | 16.7 | 11.7 | 3.3 |
| Lumbar hyperlordosis | 61.7 | 61.7 | 48.3 | 36.7 |
| Flat low back | 8.3 | 8.3 | 8.3 | 8.3 |
| Thoracic kyphosis | 1.7 | 1.7 | 1.7 | 1.7 |
| Upper back flat | 1.7 | 3.3 | 0.0 | 0.0 |
| Dropped shoulder | 41.7 | 41.7 | 38.3 | 30.0 |
| Elevated shoulder | 3.3 | 5.0 | 5.0 | 1.7 |
| Rounded shoulder | 26.7 | 26.7 | 20.0 | 5.0 |
| Head lateral tilt | 33.3 | 33.3 | 18.3 | 15.0 |
Improvement of Postural Deviations Following Laparoscopic Surgery for Obesitya
Using the repeated measure ANOVA, the downward trends of the changes in weight and body mass index were all significant after the surgery (Figure 1). The Friedman test also showed a significant difference after the surgery compared to before surgery in NDI and Roland Morris (Figure 1).
4. Discussion
The beneficial effects of bariatric surgery-induced weight loss on obesity-related morbidity have been clearly demonstrated although its effects on improper posture and spinal pain were uncertain. As shown in our survey, Roux-en-Y gastric bypass surgery not only significantly reduced disability resulting from spinal pain, but also improved some postural faults in severely obese patients.
The effect of obesity surgical approaches on the pain in the upper and lower extremity joints and the spinal area has been evaluated. Some studies (21-29) showed that musculoskeletal pain attenuated or abolished in morbidly obese persons after weight loss. According to Hacken et al. (29) and Vincent et al. (30) studies, the range of BMI reduction by bariatric surgery was 6.2 - 14.7 kg/m2 accompanied by a reduction in knee and back pain in 5% - 100% of the patients, while the pain reduction in 31% - 94% of the patients lasted up to 2 years. In total, the long-term improvement of musculoskeletal functionality following surgery has been also revealed in obese ones that are compatible with our findings. As shown by Iossi et al. (31) the quality of life and functionality improved 6 months and 1 year after surgery-induced weight loss. In addition, the acquired weight 12 months after surgery was also significantly correlated with most functional outcomes. In our study, weight loss maintained for 12 months. Hooper et al. (24) demonstrated that 100% and 23% of the obese people complained of musculoskeletal disturbances before and after weight loss, respectively. The most improvements were related to the cervical spine (90%), lumbar spine (83%), foot (83%), and myofascial syndrome (92%). 79 percent of the patients suffered from upper extremity pain before reducing weight while the rate after weight loss was 40%. Finally, in terms of lower extremity pain, the rates of people who had pain before and after surgery were 100% and 37%, respectively. The authors believe that the reduction in musculoskeletal pain is directly associated with significantly modified body posture state.
Our findings showed that although disability and pain in the cervical, upper, and lower back were not high before the surgery, their mean scores improved after the intervention.
As indicated in our study, several postural dysfunctions such as anterior pelvic tilt and lumbar hyperlordosis were modified after the surgery. Exaggerated anterior pelvic tilt and lumbar hyperlordosis are usually accompanied with each other. The correction of one of them is expected to be associated with the correction of another one. The increased sagittal moment in prominent abdomen leads to lumbar hyperlordosis. Thus, after fat reduction in the abdomen, hyperlordosis is expected to be diminished. However, all patients in our study performed abdominal resistance exercise 8 weeks after the surgery. The corrected lumbar hyperlordosis and anterior pelvic tilt can be due to the increased abdominal muscle resistance.
In severe obesity, diagnosing the anterior pelvic tilt based on the ASIS (anterior superior iliac spine) and PSIS (posterior superior iliac spine) positions in the side view is so difficult because of the large volume of subcutaneous fat. Therefore, there is a probability of misdiagnosis of pelvic tilt and hyperlordosis by the plumb line in the obese people. After surgery, due to a great abdominal fat reduction, the ASIS and PSIS markers are more prominent and diagnosing postural faults would be easier and more accurate than before the surgery. Therefore, using the plumb line for these postural states in obesity is another limitation of our study.
Maintaining a faulty posture in the vertebral bodies leads to strains on the supporting dynamic systems such as ligaments and muscles and irritates the end of the nerves, resulting in a pain. Therefore, correcting a bad posture could improve the pain. Therefore, diminished back and lower back pain in our findings can be due to modified postural faults in the lower back and pelvic.
We found that foot hyperpronation abolished after the surgery. As similarly shown by Song et al. (32) weight reduction via different protocols leads to improved dynamic plantar loading and even some indices of foot structural condition. They found that plantar peak pressure decreased after weight loss and reduced pressure on some foot structural components such as the metatarsal bones and the medial arch leading to foot posture improvement. Our hypothesis for improving foot hyperpronation is that hyperpronation might be misdiagnosed due to the fat collection around the ankle, especially in the medial part, irritating talonavicular prominence. Therefore, the improvement of hyperpronation could be due to the fat reduction in the ankle. One of the limitations of our study was the non-accurate method for evaluation of hyperpronation. Then, it is advocated using more accurate methods of posture evaluation for diagnosing hyperpronation such as FPI (foot posture index) among obese people in the future.
Dropped and rounded shoulders also improved after the surgery. This finding can be related to some resistance exercises that all the patients took after the surgery. Resistant trapezius muscle elevates the shoulders and resistance training for external rotators leads to modifying rounded shoulders. However, overlay modified posture and weight loss after the surgery could influence the standing posture during an evaluation at the moment.
Other studies (3-7) showed a reverse relationship between weight loss and thoracic kyphosis or knee valgus. Nevertheless, in our study, the pointed postural faults did not change after the surgery. It may be due to the difference in the measurement methods. They had a more reliable method for detecting the changes such as radiography but the method of postural evaluation in our study was the plumb line.
The mean amount of weight loss in our study was almost 40 kg and the maximum amount of BMI reduction was 14. In other studies (29, 30), the beneficial effects of bariatric surgery on pain and functionality were confirmed and the amount of weight loss was as the same as that in our study. It seems that these two beneficial changes are the advantages of surgical weight loss because the amount of weight loss by surgery is higher than that in other methods.
In total, it can be concluded that weight loss can effectively improve functionality and spinal pain and when combined with exercise, it can correct some postural impairments.