1. Background
Demographic transition and population aging are the important challenges facing countries in the 21st century. Due to the demographic, social, economic, and cultural changes, the aging phenomenon is increasingly emerging as a social issue (1). The global growth rate of the elderly (1.9%) is higher than the general population (1.2%) (2). The United Nations estimates that the elderly will account for 11% of the world's total population (about 800 million), rising to about 2 billion in 2050 (3). The population of the age group of 65 years old and older, constitutes 6% of the total population in Iran (4). An elderly community poses challenges to the health system and the provision of health services. One of these challenges is drug use, its pattern, and prescription among the elderly (5). The drug use among the elderly has attracted a lot of attention in recent years, and various studies indicate an increase in the prevalence of polypharmacy in the elderly population (6, 7). Over the past few years, previous studies on the healthy and effective use of drugs in developing as well as developed countries showed that irrational drug use is a global phenomenon (8).
The elderly, due to age-related physiological changes, are susceptible to multiple common chronic diseases, which lead them to use more drugs than other life periods (9, 10). This situation result increase in irrational drug use, use of inappropriate treatments, economic burden, drug complications, and interactions (11, 12). Age increasing can cause inevitable physiological, pharmacokinetic, and pharmacodynamics changes (13, 14). These changes may lead to accumulation of drugs in the body to the toxic level and cause severe complications (15-17). In addition to the changes mentioned above, some drug use and prescription behaviors, such as the use of prescription and non-prescription drugs, self-medication, use of medicinal plants, regardless of the possible drug interaction with chemical drugs, and failure to follow medication adherence or inadequate drug prescription have highlighted the importance of the pattern of drug use in the elderly (18).
Self-medication can be defined as obtaining and consuming drugs without the advice of a physician either for diagnosis, prescription or surveillance of treatment (19, 20). Self-medication is currently one of the major problems in the treatment cycle of Iran and many other countries. This leads to bacterial resistance, lack of optimal treatment, unwanted poisonings, adverse effects and unwanted complications, drug market disruption, waste of costs, and increasing drug per capita in the society (21). According to the research, it is estimated that 83.3% of Iranians self-medicate (22). Elderly health care is one of the priorities of the Ministry of Health; the integration into primary health care (PHC) services and the elderly will form the largest number of a community’s health (care) nurse clients in the near future.
2. Objectives
The aim of the present research was to determine the pattern of drug use in the elderly population of Rasht, the capital of Gilan as the one of three Northern Province of Iran.
3. Methods
3.1. Study Design
The present study is a descriptive-analytic cross-sectional study.
The study population included all individuals who aged 60 years or older and members of the retirement centers and House of Hope of retirees of Rasht city. The sample size of this study is 381 people. The sampling method used in this study is a consecutive random sampling. Our inclusion criteria were age equal or more than 60 years, membership in these centers, the ability to communicate verbally in terms of answering questions and the willingness to participate in the study. After confirming the eligibility of the patients to participate in the research, the questionnaire was completed through interviewing the participants and observation of the medicine bags after providing the necessary explanations and obtaining their informed consent from. Also, individuals who did bring their medicine bags were asked to refer at another time with their medicine bag. A four-part questionnaire was used in this study to collect data.
3.2. Study Tools
A four-part questionnaire was used in this study to collect data about; (A) sociodemographic features (age, sex, area of residence, level of education, marital status, level of income, living arrangement, smoking and abuse of drug); (B) chronic disorders and diseases (this part of the questionnaire contains a list of disorders and common diseases of the elderly, which was completed through self-reporting); (C) pattern of drug use (consists of nine questions regarding use or disuse of drugs, polypharmacy, forms of drugs taken, use of herbal medicines, self-medication, and its reasons and types, which were determined and coded based on the anatomical therapeutic chemical (ATC). Its information was completed by the researcher through interviewing the participants and observing their medicine bag, the number of drugs used included prescribed and non-prescribed drugs, vitamins and food supplements consumed within 24 hours (PRN), topical forms of drugs, herbal medicines, and medication doses were not considered, and (D) medication adherence based on the Morrisky medication adherence scale (includes four questions: Failure to follow the medication adherence due to forgetfulness, carelessness in observing the exact time of taking medications, medication discontinuation after feeling worse, and after feeling better). These questions were answered using a yes-no rating scale. The No and Yes options were given scores 0 and 1, respectively. Finally, the score 0, 1 - 2, and 3 - 4 are considered high, medium, and low adherence levels, respectively (23).
3.3. Validity and Reliability
The researcher-made questionnaire, on patterns of drug use was validated through content validation and surveying 10 faculty members of the Faculty of Nursing and Midwifery of Shahid Beheshti University of Rasht (CVI and CVR) (with score ranges of 0.9 - 1 and 0.62 - 0.8 in CVI and CVR, respectively). While investigating the internal consistency of questions, the Richardson coefficient of 20 was used on 17 subjects as a pilot study in order to measure the level of medication adherence. The obtained Richardson coefficient (α = 0.7) indicated the convergence of questions in order to determine the medication adherence. For the test-retest procedure, the medication adherence scale was completed by 17 eligible elderly people in an interval of two weeks. The correlation coefficient (r = 0.893, P < 0.001) and test-retest reliability coefficient (Re = 0.78) showed that the repeatability of this questionnaire is highly reliable.
3.4. Statistical Analysis
SPSS version 20 was used and the data analysis was performed using descriptive statistics (frequency, percentage and confidence interval of 95%, mean, and standard deviation). Chi-square tests were used to compare qualitative variables and P < 0.05 was considered as the significant level.
4. Results
A total of 381 individuals aged over 60 years of age were studied. The mean age was 67.27 ± 6.14 years and 96.3% of them lived in the city. The socio-demographic characteristics of the participants are presented in Table 1.
| Variable | Values |
|---|---|
| Age, mean ± SD (Range) | 67.27 ± 6.14 (60 - 88) |
| Sex | |
| Male | 248 (65.1) |
| Female | 133 (34.9) |
| Area of residence | |
| City | 367 (96.3) |
| Village | 14 (3.7) |
| Level of education | |
| Illiterate | 9 (2.4) |
| Reading and writing | 13 (3.4) |
| Elementary | 33 (8.7) |
| Cycle | 27 (7.1) |
| Secondary school | 159 (41.7) |
| Academic | 140 (36.7) |
| Marital status | |
| Married | 337 (88.5) |
| Single | 3 (8.0) |
| Divorced | 3 (0.8) |
| Widow | 38 (10) |
| Level of income | |
| Less than family needs | 261 (68.5) |
| Meeting family requirements | 112 (29.4) |
| More than family needs | 8 (2.5) |
| Living arrangement | |
| Alone | 23 (6) |
| With spouse | 189 (49.6) |
| With children | 20 (5.2) |
| With spouse and children | 147 (38.6) |
| With relatives and acquaintances | 2 (0.5) |
| History of smoking | |
| Yes | 357 (93.7) |
| No | 24 (6.3) |
a Values are expressed as No. (%) unless otherwise indicated.
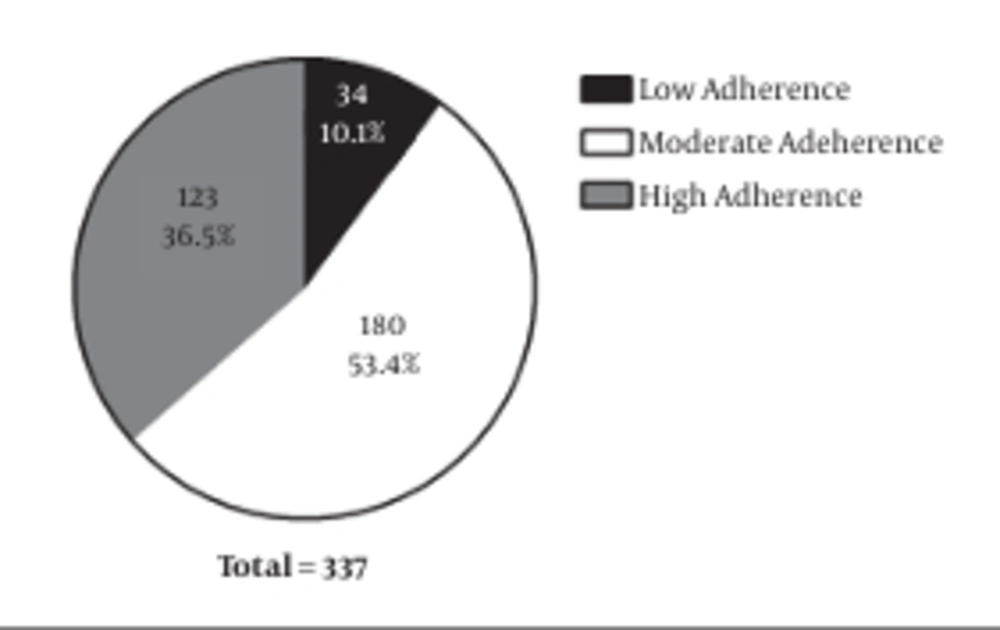
A total of 337 ones (88.5%) used drugs as mean as 3.95 ± 2.71 per person daily. Polypharmacy (taking 5 drugs a day) was observed in 38.1% of the subjects. The most commonly used drugs were Atorvastatin, Aspirin, Losartan, and Calcium, respectively. Regard drug forms, the majority of elderly people took pills and capsules (Table 2). The therapeutic classes of the elderly are used in Table 3. The most commonly used pharmaceutical groups included anti-hyperlipidemia (48.8%), non-steroidal anti-inflammatory (44.6%), cardiovascular (38.8%), supplements (38.6%), and anti-hypertensive drugs (34.1%). Also, the findings on self-medication showed that 35.7% of the individuals used self-medication and 17.6% of the subjects used herbal medicines. The most common causes of self-medication included previous use of the same drug, and symptom recovery (44.9%), minor symptoms and lack of any need for medical attention (31.6%) (Table 4). The most commonly self-medication used drugs included acetaminophen and cold tablets. Self-medication was seen more, but, insignificant in the 60 - 64 age group, male, urban, married, non-smoker groups, with a secondary level of education, and low level of income. Morrisky medication adherence criteria (Figure 1) showed that most of the subjects (53.4%) had medium medication adherence. The most common chronic diseases included hypertension (44.6%) and hyperlipidemia (35.2%) (Table 5).
| Drug Forms | No. (%) |
|---|---|
| Pill | 322 (84.5) |
| Capsule | 118 (31) |
| Ampoule | 14 (3.7) |
| Spray | 11 (2.9) |
| Drop | 11 (2.9) |
| Syrup | 3 (0.8) |
| Therapy Class | No. (%) |
|---|---|
| Anti-hyperlipidemia | 186 (48.8) |
| Non-steroidal anti-inflammatory | 170 (44.6) |
| Cardiovascular | 148 (38.8) |
| Supplements | 147 (38.6) |
| Anti-hypertensive | 130 (34.1) |
| Analgesics | 106 (27.8) |
| Anti-diabetes | 98 (25.7) |
| Reasons for Self-Medication | No. (%) |
|---|---|
| Previous use of the drug and symptom recovery | 61 (44.9) |
| The minor symptoms and lack of need to a doctor | 43 (31.6) |
| Recommendation of non-specialists to the benefits of drug therapy | 16 (11.8) |
| A similar prescription written by a doctor | 14 (10.3) |
| Pharmacy recommendation | 12 (8.8) |
| Ensuring the drug safety | 12 (8.8) |
| Having insufficient time to visit a doctor | 11 (8.1) |
| Lack of affording for visiting physicians | 8 (5.9) |
| Disbelief and trust in doctors and health centers | 8 (5.9) |
| Having belief in traditional medicine and herbal medicines | 6 (4.4) |
| Crowed physicians’ offices or treatment centers | 5 (3.7) |
| Fear and embarrassment of medical examinations | 0 (0) |
| Absence of treatment centers near the place of residence | 0 (0) |
| Chronic Disorders and Diseases | No. (%) |
|---|---|
| Hypertension | 170 (44.6) |
| Hyperlipidemia | 134 (35.2) |
| Bone and joint diseases | 115 (30.2) |
| Diabetes | 97 (25.5) |
| Heart disease | 74 (19.4) |
| Eye diseases | 77 (20.2) |
| Prostate enlargement | 64 (16.8) |
| Sleep disturbances | 59 (15.5) |
| Diseases and gastrointestinal ulcers | 37 (9.7) |
5. Discussion
In the present study, we aimed to investigate the pattern of drug use in the elderly population of Rasht. Our results revealed that 88.5% of the people used drugs. On the other hand, polypharmacy was observed in 38.1% of the cases, i.e. consumption of five drugs or more per day, which could indicate the presence of multiple and common chronic diseases in the elderly. The average number of drugs was 3.95 per day for every elderly, which is approximately in line with the findings of Delshad Noghabi et al. (1), They reported that the average drug numbers were 4.06 per person with 56.6% of persons simultaneously using four drugs per day (1). The results of the study by Haider et al. in Sweden, also showed that 88.5% of the elderly took drugs with the average number of 4.4 per day and the polypharmacy (taking 5 drugs or more) being seen in 42.2% of the elderly, which is almost similar to our findings (24). Walckiers et al. also conducted a study on the elderly residing in the Belgian care centers and community and the results showed that 81.9% of them took drugs with the average number of 3.5 per person and with a range of 0-19 and a polypharmacy rate 33% (5 drugs and more within 24 hours) (25). This difference in the findings may be due to differences in demographic characteristics, differences in regulations and supervision governing the drug use, and the prevalence of different diseases in the studied populations.
We found that the most commonly used pharmaceutical groups included anti-hyperlipidemia, non-steroidal anti-inflammatory, cardiovascular, supplements, and anti-hypertensive drugs. Jyrkka et al. also showed that the most commonly used drugs for the elderly included cardiovascular, analgesics, blood and blood forming organs, and gastrointestinal drugs (6). Moreover, Nomura referred in their study to the cardiovascular, digestive, and central nervous system drugs as the most commonly used drug group among the Japanese elderly (26). In addition, Nobili et al. indicated that antithrombotic, digestive, and diuretic drugs were the most commonly used drug groups in the Italian elderly, respectively (27). The results of the above mentioned studies that were performed in various communities show that cardiovascular drugs are among the most commonly used drugs in all studies. This similarity probably indicates the prevalence of cardiovascular diseases among the elderly in different communities.
Our results, using the Morrisky’s scale, showed that 36.5%, 53.4%, and 10.1% of the participants had high, moderate, and poor levels of medication adherence, respectively. Joshi and Shalini also demonstrated that 49.68% of persons observed the medication adherence (28). Moreover, Delshad Noghabi et al. showed that 71.5% of the subjects fully observed the medication adherence and only 2.8% of them failed to observe the medication adherence. Also, three of the main reasons justifying the lack of the medication adherence included forgetting the time of drug use, symptom recovery, and unfamiliarity with drug orders (1). This difference in results may be due to demographic differences and the type of instrument used. In the present study, 35.7% of the subjects practiced had self-medication. In some studies, the rate of self-medication was lower than the current study. For instance, the rate of self-medication was 31%, 23.9%, and 24%, respectively, in Karimy et al.’s study on the elderly patients covered by urban centers of Zarandieh (29), study of Shalini and Joshi in India (28), and Shadeh et al.’s study (30). Furthermore, several other studies, including Delshad Noghabi et al.’s study reported the self-medication of 53.3% (1). Moen et al., showed in his study, which was performed in Sweden that 38.4% of subjects used over-the-counter (OTC) drugs (31), which is more than the rate reported in the present study. This difference in results may be due to cultural and social differences, such as the level of literacy and the degree of urbanization of the subjects, the difference in the instruments used to check the self-medication, and the use of OTC drugs.
In the present study, there was no significant relationship between self-medication with any of the demographic characteristics. Similar to our findings, Davati et al., showed no significant relationship between the self-medication with age, sex, occupation, and level of income, which is consistent with the present study (5). The most important causes of self-medication included symptom recovery (44.9%), minor symptoms, and lack of need to visit physicians (31.6%), the recommendation of non-specialists to the benefits of drug therapy, prescription of similar drugs by the physician (10.3%), the drug safety and the pharmacies recommendation (8.8%). These findings were consistent with Davati et al.’s study, which attributed the most common reason for self-medication to prescribing the same drugs by the physician, prior use of the drug, and symptom recovery, minor symptoms, and lack of need to the medical attention as well as Karimy et al.’s study , which reported that the most frequent reasons for self-medication included the previous experience of the disease and its diagnosis, the availability of the required drugs, and a history of recovery resulted by self-medication (29). Considering that some of the reasons for the self-medication are frequently referred to in various studies, there is a need to consider the educational needs of the elderly in this regard. Hypertension (44.6%) is the most common disease, and other cases are as follows: Hyperlipidemia (35.2%), bone and joint diseases (30.2%), diabetes (25.5%), and cardiovascular diseases (19.4%). The results of Nobili et al. showed that the most common diseases included hypertension, diabetes, coronary heart disease, and atrial fibrillation (27). In a study in Turkey, Bahat et al. referred to hypertension, depression, dementia, and diabetes as the most common diseases (32). In a study on the elderly admitted to a hospital in Nepal, Besent et al. showed that hypertension, stroke, and cardiovascular diseases were more prevalent (33). The results of various studies indicate that hypertension was the most prevalent disease among elderly people in different societies, which can lead to other common diseases, such as cardiovascular and cerebrovascular diseases.
5.1. Conclusion
The geriatric population is on the rise worldwide. Older people are vulnerable to chronic diseases, which requires long-term medical treatment and leads to the use of several medications and drug-related problems. The pharmacokinetic and pharmacodynamic changes secondary to age or illnesses make them particularly sensitive to the adverse effects of many drugs. On the basis of the finding of this study, 88.5% of the subjects used drugs, the average number of drugs was 3.95 per day, and 35.7% of the participants had self-medication. This clearly shows that it is necessary and requires careful attention, to promote a rational use of drugs, and drug use patterns, in older people requires careful attention. Regular training programs for doctors, pharmacists, nurses, and the elderly, can not only prevent the adverse effects of irrational drug use, but also enhances the dynamics and vitality as well as the health status of the elderly.