1. Context
Diabetes mellitus (DM) is on the rise and its frequency and prevalence show an increasing trend, especially in low and middle-income countries (1). Globally, 422 million adults were estimated to live with DM in 2014 (1), compared to 108 million in 1980 (1) and 171 million in 2000 (2), and it is expected to reach 333 million in 2025 (2) and 366 million in 2030 (2). Moreover, DM as the 20th cause of disability-adjusted life years (DALYs) in 2002 will be the 11th cause of DALYs in 2030, showing nine increases in the rank order (2). Diabetes and impaired blood glucose caused 1.5 and 2.2 million deaths in 2012, respectively (1) while 43% of these 3.7 million deaths occurred before the age of 70 years (1). Furthermore, the World Health Organization (WHO) projects that diabetes will be the seventh leading cause and responsible for 3% of all deaths in 2030 (2). It is also estimated that up to 13 percent of the world’s health care budget will be spent on diabetes care in 2025, while high-prevalence countries will spend up to 40 percent of their budget (3). All these figures show that diabetes, as one of the four priority non-communicable diseases, is an important public health problem (1). On the other hand, mobile health (m-health) as a subgroup of electronic health (e-health), by the application of mobile technologies, including phones, tablets, telemonitoring, and tracking devices, can play an invaluable role in the better management of DM and its risk factors (4). The current data show that there are almost 7 billion mobile phone subscriptions worldwide with a mobile penetration of 96% at the global level and 90% in developing countries (4, 5). In 2015, 45000 m-health publishers had activities around the world and more than 3 billion (bn) downloads of m-health applications (apps) were reported. 48 percent of these downloaders are chronically ill patients and DM patients are at the top of the list of them (6).
In DM, as one of the commonest chronic diseases, e-health tools such as m health can potentially help patients and care providers through different ways including prevention (by educating and training for remote behavioral change), diagnosis (by detecting blood glucose level), treatment (by medication adherence tracking), care coordination (by providing patient-physician synchronous or asynchronous relationship and clinical appointment reminding), and checking the efficacy of diabetes treatment (by monitoring Hemoglobin A1c (HbA1c) level). To date, there has been much primary and secondary evidence on the role of e-health and m-health in the management of DM. However, the results of these studies are sparse (5, 7) and controversial. Therefore, in this study, we aimed to compare the results of systematic review and meta-analysis studies to present a more comprehensive and conclusive result about this issue.
2. Evidence Acquisition
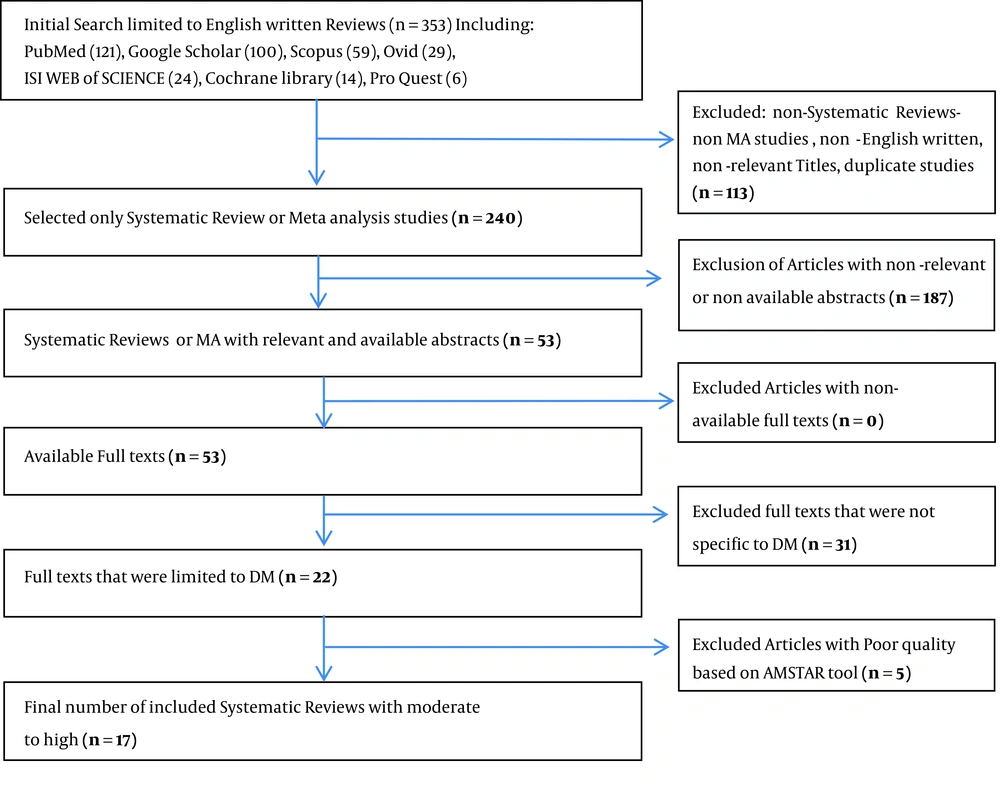
This review study was conducted in 2016. Our search had five stages: screening, eligibility assessment, the inclusion of data, extraction of data, and checking for overlaps among papers. In the screening stage, two reviewers independently searched the databases of ISI-Web of SCIENCE, PubMed, SCOPUS, Google Scholar, Pro Quest, Ovid, and Cochrane Library. A non-date limited search using Boolean operators (AND, OR) was used to combine the keywords in different combinations of “m health, M Health, m Health, M health, Mobile Health, mobile health, Mobile health, mobile Health, e health, E Health, e Health, E health, Cellular Phone, text message, SMS, MMS, and Internet” with the keywords “Diabetes Mellitus, Diabetic.” In this stage, only systematic review (SR) or meta-analysis (MA) studies were selected, while non-English papers, papers with non-relevant titles, duplicated papers, papers with non-available abstracts or full texts, and papers that were not specific to diabetes mellitus were excluded. We also had a look at the list of references of the selected papers to identify any additional reviews not captured by the primary search. In the second stage, to find eligible papers, the full texts of the screened papers were extracted and read by details and their qualities were measured using the checklist of Assessment of Multiple Systematic Reviews (AMSTAR). The AMSTAR is a valid and reliable measurement tool designed to assess the methodological quality of systematic reviews (8-10). In this tool, there are 11 items that should be regarded in checking the quality of each SR study, including the items: “Was an 'a priori' design provided?”, “Was there duplicate study selection and data extraction?”, “Was a comprehensive literature search performed?”, “Was the status of publication (i.e. grey literature) used as an inclusion criterion?”, “Was a list of studies (included and excluded) provided?”, ”Were the characteristics of the included studies provided?”, “Was the scientific quality of the included studies assessed and documented?”, “Was the scientific quality of the included studies used appropriately in formulating conclusions?”, “Were the methods used to combine the findings of studies appropriate?”, “Was the likelihood of publication bias assessed?” and “Was the conflict of interest stated?”. In the third stage, only papers with moderate (score 5 - 7) or high (score 8 - 11) quality remained in the study. In the fourth stage, the characteristics of each study including author(s), date of publication, type of study (SR or MA), study setting, number, extreme date of publishing and duration of included sub-articles, type of DM (type 1, type 2, Gestational DM), sample size, age of participants, countries in which sub-set studies were conducted, type of applied technologies, measured outcomes, and final conclusion were presented in the tables. In the fifth stage, the overlaps of the references among studies were checked by END NOTE software. In all the five stages, disagreements between the two reviewers were relieved by several meetings and revision of the searching protocol.
2.1. Ethics
Strict ethical standards were maintained in all the stages of this study. We cared to keep our neutrality in all steps to avoid the biased conclusion. All studies that supported the positive effect of e-health on the management of DM and those that reported non-conclusive and even opposite results were behaved in the same way by our team. Furthermore, the research protocol of this study was approved by the Ethics Committee of Shiraz University of Medical Sciences (Registration No. 95-10288).
3. Results
In the screening stage of this study, 353 papers were identified based on their titles. Among them, 240 SR or MA studies were selected. In the next step, 53 abstracts with available full texts remained and then 22, papers that were specific to DM were included. Finally, 17 studies with moderate to high quality were included in this study (Figure 1). Table 1 includes the characteristics of 17 finally included articles comprising 11 SA and 6 MA studies. These studies were published between 2005 and 2014. The total number of sub-articles was 533 and the date of publication of these articles was from 1990 to 2014. All articles included a kind of interventional study such as randomized clinical trial (RCT). Six articles studied DM type 2 (DM2), two assessed only DM type 1 (DM1), five investigated both types of DM, and four studies included DM1, DM2, and gestational DM. The total number of participants in these studies was 38641 (in the range of 2 - 958 in different studies) and all age groups were studied from pediatric age to the elderly groups. The duration of conducting sub-set studies ranged from time needed for two phone calls to 60 months. These subset studies were conducted in North America, Europe, Asia, and Oceania. The mean quality score of 17 selected papers was 7.1 (out of the total score of 11). Table 2 summarizes the type of interventions and their effects on the outcomes of DM. In the sub-set articles, the effects of different types of technologies such as short message service (SMS), multimedia messaging service (MMS), phone calls, voice calls, Tele-monitoring, Tele-consultation, Faxing, video conferencing, the use of glucometer apps, CD-ROMs, personal digital assistant (PDA) tools, and digital cameras were assessed and compared with the usual care. Nine out of 17 included studies (53%) showed a significant improvement in the glycemic control by reduction of HbA1c (11-19). Among these articles, two reported a small effect for the intervention on the glycemic index (11, 14) while the remained papers showed a greater effect on HbA1c (12, 13, 15-19). On the other hand, eight studies revealed unclear, inconclusive, or inconsistent effects on HbA1c (20-27). Three studies advocated mobile subgroup interventions and text messaging when compared to other interventions (12, 14, 19). However, the long-term effects of these tools in the management of behaviors and glycemic control were unclear as noted by two other papers (15, 21). One study showed that persistent use and greater uploads of website data caused a more improvement in the glycemic index in diabetic patients (22). The impact of e-health on the quality of life (QOL) and satisfaction of diabetic patients was determined in some research (17, 18, 26) but not proved by another report (14). The need for planning e-health programs based on behavioral change techniques (BCTs) was emphasized by one study (13). The cost-effectiveness of using Tele-consultation (25, 26) and home monitoring (19) in the management of DM was concluded by three studies against the majority of studies that remarked unclear, desperate, or inconsistent results or revealed the lack of the standard indices for measuring this index (11, 14, 15, 23, 25, 27). One study showed that age, sample size, diabetes duration, intervention period, HbA1c baseline level, and intervention type had associations with the clinical outcome of the intervention (12). The importance of participation of patients and their views in designing m-health programs was emphasized by another study (25). Among other research gaps in this field are the assessment of the effect of e-health tools on education (27), holistic assessment of outcomes, clinical, behavioral, and care coordination between patients and health providers (23, 25), adaptation of tools by users (15), and detecting the role of psychosocial factors in increasing the effect of these technologies (21). Moreover, the need for providing evidence on the long-term effect of e-health on increasing physical activity (16), identifying strategies to reduce tool users’ attrition rate (22), or enhance adherence and sustainability in order to increase the effectiveness of technology-based interventions in diabetes care (16, 22) and testing the applied software and its time, frequency, and format (21) were also announced by some research. The common points of most papers were the recommendations on conducting stronger interventional or other types of research (16, 17, 20-25, 27). A significant publication bias was reported in one study (11). The quantitative overlaps in the cited references among the subsets were not reported by the included papers in this study. The findings of this study also showed out of nine studies that remarked the positive effects of m-health on the outcome of DM, five included MA while out of eight studies that did not support such effect, one included MA. In the first group of studies, 271 sub-articles and in the second group, 278 sub-articles were studied. The maximum duration of follow-up in the sub-set studies in the first group was five years and in the other group, it was two years. Moreover, in the first group of studies, five papers studied DM2, three assessed both DM1 and DM2, and one focused on DM1, DM2, and gestational DM, while these figures for the other group were zero, three, and three, respectively. Two studies in the second group were limited to DM1 patients. The total population size studied in these groups was 28969 and 9975, respectively. The mean quality score of studies in the first group was 7.2 and in the second group, it was 7.0. It was also revealed that the overlap percentage of the sub-set articles among nine papers that were supportive of the effect of m-health and other technologies on the management of DM was 25.7% and among eight papers that did not conclude such an effect, it was 30.3%. The overlap between the first and second groups of papers was 19.1%.
| Author/ Year of Publication/ Reference | Type of Study | Number of Subset Articles (Date Range of Publication) | Designs of Subset Studies | Duration Range of Conducting Subset Studies | Type of Studied DM | Total Number of Studied People (Range of Sample Size in Subset Studies) | Quality Score (Out of 11) | Age (Years) or Age Group of Participants in Subset Studies | Countries or Continents That Subset Studies Were Conducted in |
|---|---|---|---|---|---|---|---|---|---|
| Zhai et al. 2014 (11) | SR, MA | 47 (2000 - 2014) | RCT | 3 - 60 m | DM2 | 8149 (13 - 844) | 8 | 42.3 - 70.9 | USA, South Korea, Italy, Iran, Jordan, Poland, Germany, Canada, UK, Spain |
| Saffari et al. 2014 (12) | SR, MA | 10 (2005 - 2013) | RCT | 3 m - 1 yr | DM2 | 960 (34 - 274) | 9 | 52.8 | Taiwan, Korea, USA, India, Bahrain, Iran |
| Peterson 2014 (20) | SR | 14 (2005 - 2013 ) | RCT, cohort, pilot study, case study | 1 - 9 m | DM1 | 266 (2 - 46) | 5 | Adult / Pediatric / Pregnant | USA, Jordan, Norway, Italy, Poland, UK, Spain |
| Van Vugt et al. 2013 (13) | SR | 13 (2002 - 2012) | RCT | 1 - 18 m | DM2 | 3813 (15 - 958) | 6 | 57.2 (40.1 - 67.2) | North America, Asia, Europe |
| Pal et al. 2014 (14) | SR,MA | 16 (1986 - 2011) | RCT | 2 phone calls - 18 m | DM2 | 3578 (30 - 886) | 10 | 20 - 67.2 | USA, South Korea, Australia, China |
| Herbert et al. 2013 (21) | SR | 7 (2006 - 2012 ) | RCT | 11 wks - 12 m | DM1 | 320 (11 - 92) | 7 | 8 - 25 | Austria, New Zealand, Norway, USA,UK |
| EI-Gayar et al. 2013 (15) | SR | 104 ( 1982 - 2012) | RCT, Cluster RCT | 12 hrs - 60 m | DM1 DM2, Gestational DM | 17040 (6 - 2924) | 5 | 12 - 70 | USA, Canada, UK, Korea, Israel, Spain, Italy, Bahrain, France, Norway, Germany |
| Connelly et al. 2013 (16) | SR | 15 (2001 - 2013) | RCT | 6 wks - 12 m | DM2 | 4567 (30 - 958) | 6 | 51 - 60.7 | USA, South Korea |
| Yu et al. 2012 (22) | SR | 3 (earliest to 2011) | RCT, controlled clinical trial, before-after, observational studies | 12 m | ND | 303 (16 - 183) | 8 | 18 - 63 | Australia, USA, UK, Switzerland, New Zealand, Canada |
| Holtz and Lauckner 2012 (23) | SR | 21 (2004 - 2010) | RCT, pilot, controlled clinical trial | 2 wks - 52 wks | DM1, DM2 | 1035 (6 - 100) | 6 | 13 | USA, UK, Italy, Ireland, Scotland, Finland, Norway, France |
| Baron et al. 2012 (24) | SR | 24 ( 2002 - 2011 ) | RCT | 3 - 12 m | DM1, DM2 | 1678 (10 - 297) | 6 | > 18 | China, Italy, USA, UK, Korea, Spain, Austria |
| Verhoeven et al. 2010 (25) | SR, MA | 90 (1994 - 2009) | RCT, before-after, quasi-experimental, cohort, expert opinion | 2 - 12 m | DM1, DM2, Gestational DM | 1423 (20 - > 100) | 7 | Younger than 30 and Adults | USA, Asia, Australia, Europe |
| Polisena et al. 2009 (17) | SR, MA | 26 (1998 - 2008) | RCT, observational studies | 3 m - 2 y | DM1, DM2 | 5069 (9 - 821) | 8 | 8 - >100 | USA, Germany Poland, Finland, Spain, Japan, South Korea, Italy, Canada, China |
| Krishna and Boren 2008 (18) | SR | 18 (2003 - 2007) | RCT, pre-post studies | 3 - 12 m | DM1, DM2 | 1176 (7 - 274) | 5 | Children-Adults | Austria, Japan, France, Korea, Norway, Spain, Taiwan, UK, USA |
| Verhoeven et al. 2007 (26) | SR | 39 (2005 - 2007) | RCT, observational studies with or without control, pre-post, quasi-experimental | 6 wks - 24 m | DM1, DM2, Gestational DM | 3141 (5 - 594) | 8 | Children, Teenagers, Adults | USA, Spain, Germany, Netherland, Denmark, UK, France, South Korea, Australia, China |
| Farmer et al. 2005 (27) | SR | 26 (1990 - 2004) | RCT, cohort, cross over Trial, non-parallel group trial | 3 m - 12 m | DM1, DM2, Gestational DM | 1809 (6 - 280) | 9 | All ages | Poland, Italy, Spain Saudi Arabia, Canada, Germany, France |
| Liang et al. 2011 (19) | MA | 22 (4 - 2010) | RCT, quasi-randomized trials, before-after trials, randomized crossover trials | 3 - 12 m | DM1,DM2 | 1657 (10 - 274) | 8 | 44 | Korea, UK, Austria, USA, Italy, France |
Abbreviations: e-health, electronic health; DM, diabetes mellitus; SR, systematic review; MA, meta-analysis; RCT, randomized control trial; m, months; DM2, diabetes type 2; USA, United States of America; UK, United Kingdom; yr, years; DM1, diabetes mellitus type 1; ND, not defined; wks, weeks.
| Author/Year of Publication/ Reference’ Number | Intervention | Outcome | Conclusion and Recommendations |
|---|---|---|---|
| Zhai et al. 2014 (11) | Phone-calling, SMS, video conferencing, telemedicine | Clinical effectiveness and cost effectiveness of changing HbA1c | A small, but statistically significant reduction in HbA1c (pooled difference in means s = 0.37, 95% CI = -0.49 to -0.25, Z = -6.08, P < 0.001) was found. Desperate results about cost-effectiveness were found. Telemedicine potentially allow for more effective self-management of DM2. Significant publication bias was detected, suggesting that the literature should be interpreted cautiously. |
| Saffari et al. 2014 (12) | Text-messaging, Internet | Changing HbA1c | HbA1c was reduced significantly after education. The effect size for glycemic control in studies that used text- messaging only was 44%; however, for studies that used both text messaging and Internet, the effect size was 86%. Age, sample size, diabetes duration, period of intervention, level of HbA1c and type of intervention may associated with effectiveness of such interventions. |
| Peterson 2014 (20) | Phone calling-SMS,Video conferencing Internet | Changing HbA1c | Initial results for glycemic control appear promising, though inconclusive. Studies with stronger methods are needed to improve the reliability of results and guide physicians or consumers on which tools are best. There is still a need for focused research exclusively on DM1 that assesses glycemic outcomes. |
| Van Vugt et al. 2013 (13) | Web based (online) | Health behavior change | 70% of studies reported statistically significant improvements in clinical outcomes measures, such as HbA1c, Fasting blood glucose, cholesterol, and triglycerides. A relatively small number of theory-based online self-management support programs for DM2 have been reported using only a select number of BCTs. The development of future online self-management interventions should be based on the use of theories and BCTs and should be reported accurately. |
| Pal et al. 2014 (14) | Mobile, Internet, clinic-based | HbA1c, biological markers, cognitive, behavioral and emotional outcomes, cost effectiveness, adverse event data. | Interventions appear to have small benefits on glycemic control in DM2: the pooled effect on HbA1c was 20.2% (22.3 mmol/mol [95% CI 20.4 to 20.1%]). This effect was larger in the mobile phone subgroup. However, There was no evidence of benefit for biological, cognitive, behavioral, or emotional outcomes in DM2. There was no evidence of improvement in depression, quality of life, blood pressure, serum lipids or weight. |
| Herbert et al. 2013 (21) | Text messaging by SMS, Internet, e mail, Pedometer | Changing HbA1c and behavioral change | Text messaging are feasible and enjoyable, but yet their clinical significance for long-term daily DM1 management behaviors and glycemic control is unclear. Researchers are recommended to carefully consider the format, frequency, and timing of Text messaging interventions and to fully test software before implementation. Future research needs include utilization of experimental designs such as randomized controlled trials, SMART design trials and stepped wedge design trials to clarify specific medical and psychosocial outcomes, the role of caregivers/peers and incentives, and utility in clinical settings. |
| EI-Gayar et al. 2013 (15) | Internet, cellular phones, telemedicine, and decision support techniques | Self-management for DM | Overall, 74% of studies showed some form of added benefit, 13% articles showed no-significant value provided by IT7 , and 13% of articles did not clearly define the added benefit due to IT. There is a distinct need for more comprehensive interventions, in which several technologies are integrated in order to be able to manage diabetes. IT interventions should be theoretically founded and should based on principles of user-centered and socio-technical factors in its planning, design and implementation. Moreover, the effectiveness of self-management systems should be assessed along multiple dimensions: Motivation for self-management, long-term adherence, cost, adoption, satisfaction and outcomes as a final result. |
| Connelly et al. 2013 (16) | Text messaging by mobile, websites, CD-ROMs computer-learning-based technology | Promotion of physical activity | Of eight studies that assessed changes in HbA1c, four found significant decreases: two mobile phone interventions and two web-based interventions. Average decreases in HbA1c were 22 mmol/mol (2.0%, P < 0.05) and 11 mmol/mol (1.1%, P < 0.001) in the mobile phone interventions and 1 mmol/mol (0.6%, P < 0.05) and 7 mmol/mol (0.6%, P < 0.05) for the web based interventions. One web-based intervention , a mobile phone intervention and a computer-learning-based intervention found non-significant reductions in HbA1c of 2 mmol/mol (0.2%), 1 mmol/mol (0.1%) and 16 mmol/mol (1.5%), respectively, with the latter also finding reductions of 9 mmol/mol (0.8%) in the control group. The last web-based intervention resulted in a 1-mmol/mol (0.1%) increase in HbA1c. All studies (especially web-based interventions and email and logbooks) found an increase in physical activity but 60% studies reported significant change. Overall, technology is effective in increasing physical activity; however, evidence of sustainability is needed. Future research should focus on which components effectively promote physical activity and enhance adherence to deliver sustainable outcomes. |
| Yu et al. 2012 (22) | Web based audiovisual tools | Glycemic control and cardiovascular risk Factor; hypertension, dyslipidaemia , smoking cessation; nutrition, physical activity and weight | Tools showed moderate but inconsistent effects on a variety of psychological and clinical outcomes including HbA1c and weight greater improvements in patient outcomes were seen with greater use of the tool. For example persistent website users had greater improvement in HA1c than intermittent users, and a larger number of website data uploads was associated with a larger decline in HbA1c Few tools were identified that met our criteria for effectiveness, usefulness, sustainability, and usability. Priority are as include identifying strategies to minimize website attrition and enabling patients and clinicians to make informed decisions about website choice by encouraging reporting of website quality indicators. |
| Holtz and Lauckner 2012 (23) | Mobile text messaging , DM related applications | Self-efficacy, HbA1c, self-management behaviors.95% of studies examined patient perspective and 19% examine healthcare providers | There is promise in that many of the outcomes had positive trends, such as for HbA1c levels, self-efficacy, and diabetes knowledge. However, many of studies lacked sufficient sample sizes or intervention lengths to determine whether the results might be clinically or statistically significant. Future research should examine other key issues, such as provider perceptions, integration into a healthcare practice, and cost. |
| Baron et al. 2012 (24) | Text feedback by mobile phone, PDA,Tele monitoring | Effect of education, CHO, protein, calories intake, HbA1c, blood glucose and Insulin dose monitoring, blood pressure, weight, exercise, medication, level of wellbeing | Most studies had important methodological weakness and resulted inconsistent and weak findings for both types of DM. Therefore, strong researches is needed. |
| Verhoeven et al. 2010 (25) | Cell phone, SMS, e mail, fax, digital camera, palmtop glucometers, PDA, videoconferencing, web based management systems | HbA1c, dietary values, blood pressure, quality of life, behavioral outcomes; patient-caregiver interaction, self-care and care coordination outcomes; usability of technology, cost-effectiveness, transparency of guidelines, equity of access to care | The included studies suggest that both synchronous and asynchronous tele-consultations for diabetes care are feasible, cost-effective, and reliable. However, it should be noted that many of the included studies showed no significant differences between control and intervention groups. This might be due to the diversity and lack of quality in study designs. Future research needs quasi-experimental study designs and a holistic approach that focuses on multilevel determinants (clinical, behavioral, and care coordination) to promote self-care and proactive collaborations between health care professionals and patients to manage diabetes care. A participatory design approach is needed in which target users are involved in the development of cost-effective and personalized interventions. Patients as part of the design team stimulates and enables designers to think differently, unconventionally or from a new perspective, leading to applications that are better tailored to patients’ needs. |
| Polisena et al. 2009 (17) | Cellular phone, telephone, videophone, tele monitoring, video conferencing, websites | HbA1c,hospitalization, quality-of-life, patient satisfaction, specialist visit | Tele monitoring had a positive effect on HbA1c but the results were mixed for telephone support. Study results indicated that home tele health helps to reduce the number of patients hospitalized, hospitalizations , bed days of care and enhances quality-of-life and patient satisfaction outcomes. More studies of higher methodological quality are required to give more precise insights into the potential clinical effectiveness of home telehealth interventions |
| Krishna and Boren 2008 (18) | Text messaging by cell phone and e mail, reminders | Behavior change by POEM,exercise, medication feedback, user satisfaction, reduction of HbA1c , Improved health status | HbA1c was improved among those receiving education and care support. Cell phone and text messaging interventions increased patient-care provider and parent-child communication and satisfaction with care. POEM Increased knowledge and self-efficacy to carry out self-management behaviors. |
| Verhoeven et al. 2007 (26) | Tele consultation, videoconferencing | HbA1c, patients’ satisfaction, cost effectiveness, transparency, quality of life, access to care | The selected studies suggest that both teleconsultation and videoconferencing are practical, cost-effective, and reliable ways of delivering a worthwhile health care service to diabetics. However, the diversity in study design did not show a significant reduction in HbA1c (0.03%,95% CI = - 0.31% to 0.24%) compared to usual care. Most of the reported improvements concerned satisfaction with technology , improved metabolic control and cost reductions. However, improvements in quality of life, transparency and better access to care were hardly observed. |
| Farmer et al. 2005 (27) | Mobile phone, text messaging, telemedicine call, voice call, modem for transfer of data | Feasibility, acceptability and effectiveness of telemedicine applications designed to improve the outcomes of care; changing HbA1c | Telemedicine for diabetes care is feasible and acceptable, but evidence for its effectiveness in improving HbA1c (−0.1%, 95% CI −0.4% to 0.04%) or reducing costs while maintaining HbA 1c levels or improving other aspects of diabetes management is not strong. Further research should seek to understand how telemedicine might enhance educational and self-management interventions and RCTs are required to examine cost-effectiveness. |
| Liang et al.2011 (19) | SMS text messaging, mobile phones, Internet | management of DM | There was strong evidence that mobile phone interventions reduced HbA1c values (SMD 0.51%, 95% CI 0.33 to 0.69%) especially in patients with DM2 compared to DM1. However, no significant differences were found for any of the other subgroup analyses. Home monitoring of DM would be cost-effective. |
Abbreviations: SMS, short message service; HbA1c, hemoglobin A1c; DM2, Diabetes type 2; DM1, diabetes type 1; BCTs, behavioral change techniques; SMART, specific, measurable, agreed upon, realistic and time-based; IT, information technology; PDA, personal digital assistant; CHO, carbohydrate; POEM, patient-oriented education management system; RCTs, randomized clinical trial; SMD, standardized mean difference.
4. Discussion
The World Health Organization (WHO) reported a nearly double increase in the prevalence of DM among adults older than 18 years from 4.7% in 1980 to 8.5% in 2014 and stated that as a part of the 2030 agenda for sustainable development, early mortality due to DM should decrease to one-third (1). On the other hand, e-health technologies including mobile phone are increasingly being used (28) and it is estimated that the global smartphone market will grow to reach 3.45 billion mobile app users by 2017. Theoretically, e-health can play its role in the management of DM through different ways including counseling, decision-aids making, appointment scheduling, educating and training for remote behavioral changes, follow-ups, using glucometer apps, reporting glycemic indices such as HbA1c, sending feedback to physicians, receiving feedback from physicians, dietary guidance, medication adherence, and sending reminders for continuity of care (5). Data show that the most number of mobile apps for medical use were made for DM and most studies that aimed to assess the clinical efficacy of m-health focused on this disease or its associated risk factors (6). In this study, we found that the effects of m-health and other types of e-health tools on different aspects of DM including prevention, diagnosis, and especially treatment were assessed by a large number of studies in many countries, especially in North America and Europe countries. Most of the research included a variety of interventions and a diversity of measured outcomes. Nearly half of the SR/MA studies proved the positive effects of these interventions on the outcome of DM contrary to another half that declared unclear, inconsistent, or non-conclusive results. The findings showed that studies in the first group were more powerful in terms of the type of included studies, had nearly three times higher total sample size, higher quality scores, and less overlap among their subset studies. However, the total study population in the total of 550 subset studies in 17 SR/MA studies included in the current analysis was not high enough in proportion to the number of available e-health tools, the variety of countries, and DM patients’ population. These figures reveal that decision-making based on available evidence is not easy and what confirms our claim in this regard is that at least 53% of the surveyed studies recommended conducting further research with stronger methods. Evidence shows that 99% of received mobile text messages are opened, 90% of all mobile text messages are read within three minutes of being received (4), and reminders have the highest impact on changing patients behaviors while they are most easily implemented compared to personalized messages, education, dashboards, gamification, and other m-health facilities (6). Similarly, the findings of our study showed that text messaging by mobile phones, especially when integrated with other tools, was the most common applied e-health intervention for improving the outcome of DM. This result came from a one high-quality MA study that was conducted in six countries (12) and another SR study with moderate quality that was conducted in nine countries (18). One study with moderate quality that studied only DM1 patients in five countries revealed that text messaging was feasible and enjoyable but its long-term effect on the glycemic index of these patients was unclear (21). The importance of long-term use and sustainability in using such tools to cause an improvement in the DM outcome were noted by only 25% of the studies (15, 16, 21, 22). The assessment and importance of considering the e-health effect on QOL and satisfaction of diabetic patients were regarded by 25% of the studies (14, 17, 18, 26) and except one study (25), none of them recommended considering patients’ views in designing such tools. The evidence shows that patients’ views, values, expectations, and feedbacks, as the main part of these processes, are actually neglected and this may be another important reason for the failure of these tools to achieve expected success following using these technologies. Another report showed that these apps have not yet had an enough significant acceptance rate by target groups and most apps are too narrow in their functionality or too technical to become a daily companion (29). Moreover, the evidence of our study revealed that the importance of considering medical professionals’ views and their experiences in designing and developing e-health tools was not regarded by any of the included studies. However, companies claimed that in 2015, in 51% of instances of m-health apps development, medical professionals were a member of their team and in 45%, they collaborated with developers of these tools (6). On the other hand, they announced that their hope for these tools to be used by medical care providers has decreased (6). Therefore, this paradox should be evaluated by non-biased research that also considers the economic impact of using these tools on the income and time of medical physicians. The evidence of companies shows that medical doctors are the most threatened group by m-health industry due to decreasing their visiting income when patients receive remote care through using these apps. Therefore, they are not welcome to use these methods (6). The educational effect of m-health on reducing HbA1c was remarked by two studies (12, 18). However, two other studies did not show a clear result and recommended doing further research on it (24, 27). Designing e-health tools based on behavior change techniques (BCTs) was emphasized by only one study (13) but it was unknown how much behavioral experts’ opinions are included in the planning of these facilities. It should be considered that BCTs are diverse, dynamic, and increasing. BCTs for remote changing of DM patients’ behaviors may differ according to the characteristics of patients in different places and in different times. It means that a kind of BCT may be successful in one group of patients or in a specific time but it may not work in another group of patients or another time. Therefore, there is no a single prescription for the behavioral changing of all DM patients in different places or in different times and participation of BCTs experts in the planning of such tools is necessary. Cost-effectiveness of e-health tools is another important aspect that should not be ignored (5). However, 18% of the included studies reported cost-effectiveness and 35% concluded unclear results or lacked enough evidence on it. Therefore, determining standard indices for cost-effectiveness is a key step for measuring this item by researchers aiming to have a holistic assessment of e-health effect on the DM management. A nearly holistic approach in conducting research about the e-health effect on the management of DM was applied by only two studies (14, 18). The characteristics of used e-health apps such as format, frequency, and timing and full testing of them were only recommended by one study (21) while most studies did not consider these points. By the above evidence, we can better understand that the management of DM by e-health is complex. The characteristics of the types of DM are varied and patients with DM in different parts of the world or during their lives show different responses to interventions. Moreover, there is an increasing trend in the production of tools and apps for the management of DM. Furthermore, health care providers’ approach and their reaction to these technologies add to the complexity of this issue. Therefore, the outcome of using these tools is based on the characteristics of all these four aspects: DM, patients, care providers, and tools themselves. In each of these aspects, many sub-items should be regarded both in designing interventions and in conducting research with the aim of assessing or evaluating their efficacy in the management of DM. For example, the type of DM, DM1, DM2, and Gestational DM, the duration of DM, the level of the glycemic index, and the severity of DM potentially can influence the outcome of DM. Patients’ characteristics including demographic, psychological, social, and economic status and their views, values, and perspectives may determine the consequence of such interventions, as well. Health care providers’ opinion and behaviors are also important in using these tools for the establishment of a synchronous or asynchronous two-way communication with users. The effect of these interventions on the income of physicians or their time may also be an important determinant of their behaviors in this regard. Tools’ features including to what extent they are set by standard criteria, are adopted by users, meet behavioral change models, and are secure, accessible, applicable, user-friendly, and costly can determine the outcome in DM patients who use these tools. Therefore, there is no doubt that no single policy or intervention can ensure or satisfy us to have significant positive effects on the improvement of all aspects of DM or have a persistent effect on it. Therefore, research, regardless that in which part of the world it is conducted, should apply a strong method to provide a less controversial evidence for decision making by designers, publishers, patients, and healthcare providers. However, the primary priority is setting standard assessment tools that consider all of the above items before conducting such studies. We recommend also establishing a surveillance system based on all mentioned items and by the participation of all stockholders to assess the efficacy of e tools in the management of chronic diseases such as DM. There are two other important points that should be regarded. The first is that in addition to the e-health tools and research that is related to the therapeutic outcomes in diabetic patients, there is also a need to design or assess the interventions that are used for the prevention of DM. The second point, as also emphasized by WHO, is that these tools cannot and should not be regarded as a replacement for higher valued decision-making, supervision on treatment, and applied care by specialists; these tools are potentially facilitators and have a contributory role in the management of DM. Our study had some limitations. We did not investigate gray literature and non-English papers and we did not conduct a secondary MA due to the overlap among six included MA studies. However, this study has some unique strengths; we included all negative results, as well as positive results, to avoid publication bias. Moreover, calculating the overlap of references among the included studies, although it was hard and time-consuming, was done precisely and presented as figures. In this study, we also categorized the included studies into two distinct groups as supportive and non-supportive studies about the effect of e-health on the management of the glycemic index of DM and then by providing their important characteristics in the last paragraph of the result section, which enables readers to compare them at a glance.
5. Conclusions
The DM knows no limit and no one is immune from the risk of this disease. Data show DM is steadily rising around the world in both poor and rich countries. On the other hand, e-health technologies including m-health tools, although may have their own side effects such as increased immobility and susceptibility to DM, are produced as the highest rank for DM patients to improve their outcome. Much primary and secondary research aimed to assess the effect of using such tools on DM outcomes and nearly more than half concluded an improvement in the glycemic indices such as HbA1c, while less than half did not conclude such result. Therefore, telling the last word boldly is not easy although the hope persists. The reason seems clear: heterogeneity in the methods of studies in terms of the difference in study patients, type of assessed DM, type of used e-health technology, measured outcomes, and duration of studies. On the other hand, most of these studies had no or a little attention to other than objective clinical outcomes such as patients’ views, satisfaction, and their QOL, health care providers’ opinions, views of BCTc experts, and cost-effectiveness of such interventions. Therefore, conducting strong studies that use standard assessment tools is recommended. There is also a need for designing and presenting standard guides to empower users to choose and use valid e-health sources. Moreover, the establishment of an electronic surveillance system that uses the evidence of these studies in long-term is recommended.