1. Background
Gestational diabetes refers to any grade of glucose intolerance that occurs or is identified for the first time during the gestational period (1). In Iran, the estimated prevalence of gestational diabetes is about 4.9% (2). Research in Canada indicated that gestational diabetes is a risk factor for the occurrence of overt diabetes years after delivery (3). Gestational diabetes is associated with many pregnancy complications such as increased hypertensive disorders, preterm delivery, macrosomia, cesarean delivery, dystocia, and respiratory distress (4). It also increases the risk of long-term outcomes in infants born to mothers with diabetes, such as persistent impaired glucose tolerance and incidence of type 2 diabetes, obesity, and metabolic syndrome in childhood and adolescence (5-7).
According to a Cochrane review study, management of gestational diabetes may be related to the improvement of pregnancy consequences; however, there is no strong evidence regarding the best treatment with more favorable outcomes for mothers and infants (8). In addition to the type of treatment, this may be affected by poor adherence of individuals to the treatment regime as a result of beliefs towards illness and low level of health literacy (9). The important role of diabetes healthcare professionals is to inform patients with their blood glucose fluctuations by taking appropriate actions such as self-care and giving them more control over the disease (10, 11).
Self-care is any action in which each individual applies to look after his or her own health and well-being independently (12). Self-care in chronic conditions can significantly decrease the utilization of the health care system and improve the quality of life in patients (13, 14). Lack of knowledge and correct information regarding the illness as well as lack of skills in patients prevent disease recovery (15). On the other hand, self-care behavior among women with gestational diabetes was compared in a study with healthy women, and the results showed that women with gestational diabetes experience less self-care (16).
In a systematic review, lifestyle interventions (education, diet modification, exercise, and self-monitoring of blood glucose) were compared with routine care or other interventions for the treatment of women with gestational diabetes. There was no substantial evidence that lifestyle interventions compared to non-intervention or routine education can decrease the risk of pregnancy-induced hypertension, C-section, and overt diabetes in the future, perinatal mortality, and hypoglycemia. However, lifestyle intervention was related to decreasing macrosomia and neonatal fat mass. Finally, it was reported in this study that the evidence provided has poor validity due to the ‘risk of bias’ in the included studies (17). The findings of another study aimed to determine the effect of self-care training on decreasing the glycosylated hemoglobin levels in participants with type 2 diabetes, which indicated that self-care program decreased fasting blood glucose and HbA1c levels by promoting awareness, attitude, and self-care behaviors (15).
2. Objectives
Given the importance of gestational diabetes, its high prevalence and adverse outcomes, and the need for further evidence on the effect of self-care, the purpose of this research was to assess the effectiveness of self-care training on some pregnancy consequences (neonatal anthropometric indices and frequency of cesarean section, preterm delivery and macrosomia) in women with gestational diabetes.
3. Methods
3.1. Design
This study is part of a large randomized controlled trial where the variables of blood glucose levels, self-care behaviors, and quality of life were assessed as primary outcomes and their results have been published in another paper (18), and the outcomes of pregnancy have been investigated as secondary objectives.
3.2. Participants
The eligibility criteria included gestational diabetes mellitus (GDM) detected by oral glucose tolerance test (OGTT) between 24 - 28 gestational age; singleton pregnancy; willingness to participate in study; ability to care for self; having at least secondary school education; and not having any known mental disease or no other physical diseases (asthma and heart disease).
The sample size in this study has been estimated by the primary (self-care behaviors) and secondary outcomes (frequency of cesarean section and anthropometric indices). Information related to sample size calculation based on the primary outcome has been mentioned in another paper and determined 42 for each group (19). In addition, the estimated sample size was 42 women, according to previous research (20) on the frequency of cesarean delivery in women with gestational diabetes (p1 = 82.9%), and with a 40% reduction in the frequency of cesarean delivery (p2 = 0.50), α = 0.05, and power = 90%. In addition, the calculated sample size was 30 women according to research by Asnafi et al. (21) on the average weight of newborns among women with gestational diabetes (m1 = 3.37) with a 10% weight loss after the intervention (m2 = 3.03), sd1 = sd2 = 0.44, α = 0.05, and power = 90%. Since the sample size was calculated based on the self-care behavior and the frequency of cesarean delivery (42 in each group) was higher, the final sample size was considered 46 women, considering a 10% possible attrition.
3.3. Procedures
After approval by the “Regional Ethics Committee of Tabriz University of Medical Sciences” (TBZMED.REC.1394.286) and obtaining the clinical trial code (IRCT2015080510324N25), pregnant women with 28 - 30 weeks of pregnancy whose gestational diabetes was confirmed by the physician based on OGTT 24 - 28 weeks of pregnancy in their pregnancy care records and who were referred to the diabetes clinic of Tohid Hospital in Sanandaj, Iran, were selected using convenience sampling. OGTT is performed routinely as a diagnostic test for all women. In this test, a blood sample is collected from pregnant women under fasting conditions, then 75 g of glucose solution is drunk and blood samples are collected again one and two hours after drinking the glucose solution. The expected values in pregnant women are < 92 mg/dL, < 180 mg/dL, and < 153 mg/dL under fasting conditions and 60 and 120 minutes after glucose ingestion, respectively. The results equal to or above these values confirm a gestational diabetes diagnosis. After selecting the pregnant women with gestational diabetes, the aims and methods were clarified to them, and they were examined in terms of meeting the eligibility criteria if they were willing to participate in the study. Then, written informed consent was received from participants who met the inclusion and exclusion criteria. The demographic questionnaire was filled out, and the participants were assigned into two groups, namely intervention (self-care training) and control through blocked randomization in block sizes of four and six and with an allocation ratio of 1:1. To conceal the allocation, the type of intervention (self-care training or routine care) was written on paper and placed into sequentially numbered opaque envelopes. The researcher opened the envelopes sequentially when a participant entered into the study, and, depending on the type of group written on the paper in the envelope, the participants were allocated to the relevant group. Blocking was done by a person not involved in the sampling.
Individuals in the experimental group received diabetes self-care training in 4 one-hour sessions per week. The sessions included lecture and question and answer, and an educational booklet was given to the participants at the end of the first session. The training sessions were held in a group and each group consisted of seven to 14 participants. The topics provided during the sessions included the definition of diabetes and its types, gestational diabetes, complications of gestational diabetes for the mother and the fetus, the concept of self-care, the method of controlling gestational diabetes with diet, the effect of exercise on diabetes, controlling gestational diabetes with exercise, important points of exercise in diabetic pregnant mothers, measurement of blood glucose levels at home, normal levels of blood glucose, prevention of infection, and foot care.
The participants in the control group received only pregnancy care education and instruction on how to control blood glucose levels at home as provided in the hospital. The researcher called the individuals in the intervention group every week and emphasized the received training. Consequences of pregnancy (weight, height and head circumference of a newborn, type of delivery, and gestational age at birth) were recorded in the checklist by the researcher through asking the mothers and referring to the delivery records.
3.4. Measurements
Data collection tools included a demographic form and a checklist of pregnancy outcomes. The demographic form included questions such as age, marriage age, educational level, job, number of pregnancies, number of abortions, and history of cesarean section. The pregnancy outcomes checklist included questions about the delivery type, gestational age at delivery, and anthropometric parameters of the newborn (height, weight, and head circumference). The validity of the demographic questionnaire and the pregnancy outcome checklist were confirmed through content and face validity. The anthropometric indices of the newborns were measured in the labor room. The infants’ weight was measured by a scale, which was calibrated with a 500-gram standard weight before each measurement, and the head circumference and height were measured with a tape measure. The participants in both groups gave birth to their children at Tohid Hospital-Sanandaj city, Iran.
3.5. Statistical Analysis
SPSS-19 was used for data analysis. The normality of quantitative data was evaluated using Kolmogorov-Smirnov test. Independent t-test, chi-square, and Fischer’s exact tests were used to examine the consistency of the groups. Independent t-test and chi-square tests were used to compare continues (weight, height, and head circumference) and dichotomous variables (macrosomia, preterm delivery, and cesarean section) between groups, respectively. General linear model (ANCOVA test) and Multivariate Logistic Regression tests were used to compare the quantitative and qualitative variables between groups, respectively. The variables of mother’s age and body mass index were entered into the models as a covariate.
4. Results
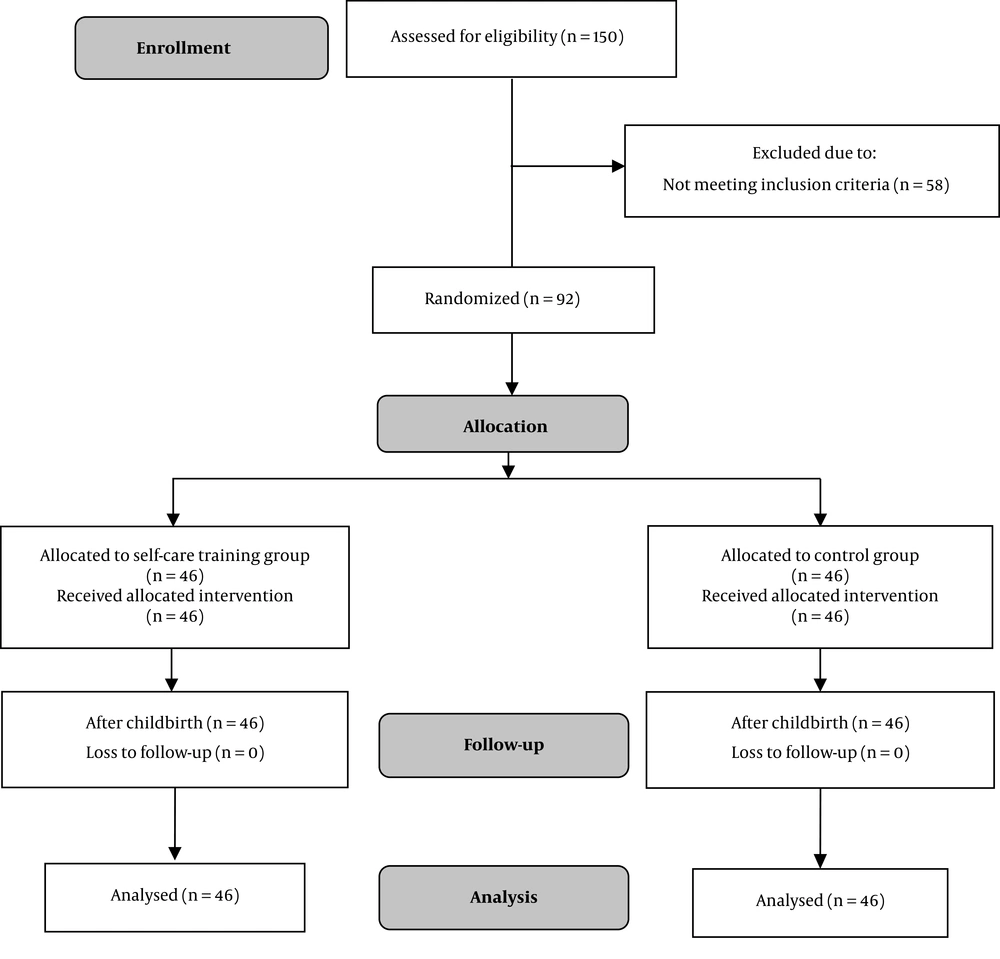
A total of 150 pregnant women with gestational diabetes were examined from Jan 18, 2016 to May 20, 2016; of whom 58 were not eligible, and finally, 92 of them participated in the study. In this research, 46 women were allocated to the training group and 46 to the routine care, and they were followed up until the postpartum period (Figure 1).
The mean ± standard deviation of participants’ age and their husbands’ age were 31.0 ± 5.0 and 35.0 ± 5.0 years, respectively. The demographic data of the participants are showed in Table 1. Two arms were similar statistically in terms of demographic features (P > 0.05).
| Items | Experimental (N = 46) | Control (N = 46) | Significance |
|---|---|---|---|
| Age, y | 30.3 ± 5.1 | 31.7 ± 4.8 | 0.979b |
| Educational level | 1.000c | ||
| Secondary school | 2 (4.3) | 2 (4.3) | |
| High school | 25 (54.3) | 25 (54.3) | |
| University | 19 (41.3) | 19 (41.3) | |
| Occupation | 0.180c | ||
| Housekeeper | 43 (93.5) | 39 (48.8) | |
| Employed | 3 (6.5) | 7 (15.2) | |
| Husband’s age, y | 34.2 ± 5.4 | 35.8 ± 5.7 | 0.635b |
| Husband’s educational level | 1.000c | ||
| Illiterate | 8 (17.4) | 9 (19.6) | |
| Elementary/secondary school | 20 (43.5) | 18 (39.1) | |
| High school/university | 18 (39.1) | 19 (41.3) | |
| Husband’s occupation | 0.817c | ||
| Unemployed | 9 (19.6) | 7 (15.2) | |
| Worker | 12 (26.1) | 14 (30.4) | |
| Employee | 25 (54.3) | 25 (54.3) | |
| BMI, kg/m2 | 26.7 ± 3.0 | 27.6 ± 3.5 | 0.233b |
| Parity | 0.834c | ||
| 1 | 14 (30.4) | 19 (41.3) | |
| 2 | 21 (45.7) | 16 (34.8) | |
| ≥ 3 | 11 (23.9) | 11 (23.9) | |
| Child number | 0.331c | ||
| 1 | 19 (76.0) | 19 (67.9) | |
| 2 | 6 (24.0) | 7 (25.0) | |
| 3 | 0 (0) | 2 (7.1) |
Socio-Demographic and Obstetrics Characteristics in Two Study Groups of Women with Gestational Diabetesa
The mean ± standard deviation of weight, height, and head circumference of the newborns were respectively 3473.9 ± 403.9 g, 49.3 ± 1.2 cm, and 35.0±0.8 cm in the intervention arm and 3551.1 ± 634.4 g, 49.2 ± 1.5 cm, and 35.0 ± 1.4 cm in the control arm. The number (percent) of preterm delivery in the intervention and control group was 5 (10.9%) and 13 (28.3%), respectively. The number (percent) of cesarean delivery in the intervention and control groups was 5 (10.9%) and 27 (58.7%), respectively. The number (percent) of macrosomia was 1 (2.2%) in the experimental group and 12 (26.1%) in the control group.
Based on the independent t-test, no difference was observed between the arms in terms of birth weight (mean difference (MD): -77.1; 95% confidence interval (95% CI): -298.0 to 143.6; P = 0.489), height (MD: 0.04; 95% CI: -0.52 to 0.61; P = 0.880), and head circumference (MD: 0.04; 95% CI: -0.44 to 0.53; P = 0.860). According to chi-square test, there was a significant difference between the arms in terms of cesarean delivery (odds ratio (OR): 0.08; 95% CI: 0.02 to 0.27; P < 0.001), macrosomia (OR: 0.06; 95% CI: 0.01 to 0.56; P = 0.002), and preterm labor (OR: 0.31; 95% CI: 0.10 to 0.95; P = 0.036) (Table 2).
| Variables | Self-Care Training (N = 46) | Control (N = 46) | ||
|---|---|---|---|---|
| Quantitative variables | Mean ± SD | Mean ± SD | MD | P Value |
| Infant weight, g | 3473.9 ± 403.9 | 3551.0 ± 634.4 | -77.1 (-298.0 to 143.6) | 0.489a |
| Infant height, cm | 49.3 ± 1.2 | 49.2 ± 1.5 | 0.043 (-0.52 to 0.61) | 0.880a |
| Infant head circumference, cm | 35.0 ± 0.8 | 35.0 ± 1.4 | 0.043 (-0.44 to 0.53) | 0.860a |
| Qualitative variables | No. (%) | No. (%) | OR (95% CI) | P Value |
| Cesarean delivery | 5 (10.9) | 27 (58.7) | 0.08 (0.02 to 0.27) | < 0.001b |
| Preterm labour | 5 (10.9) | 13 (28.3) | 0.31 (0.10 to 0.95) | 0.036b |
| Macrosomia | 1 (2.2) | 12 (26.1) | 0.06 (0.01 to 0.56) | 0.002b |
Comparison of Pregnancy Outcomes Between Two Study Groups of Women with Gestational Diabetes Based on Bivariate Tests
Results of the general linear model showed that there was no significant difference between the experimental and control group in terms of newborns’ weight, height and head circumference (Table 3). Results of the multivariate logistic regression model showed that the rate of cesarean delivery (OR: 0.073; 95% CI: 0.022 to 0.238, P < 0.001) and macrosomia (OR: 0.058; 95% CI: 0.007 to 0.492, P = 0.009) in the experimental group were reduced than the control group (Table 4).
| Variables | Unstandardized Coefficient (B) | Standard Error | Standardized Coefficient (β) | CI of B | P Valuea |
|---|---|---|---|---|---|
| Infant weight (g) (reference group: control) | |||||
| Self-care training group | -64.1 | 113.3 | 0.06 | -0.62 to 0.54 | 0.573 |
| Mother’s age, y | 2.1 | 11.4 | 0.02 | -0.07 to 0.04 | 0.854 |
| Mother’s BMI, kg/m2 | 12.0 | 17.4 | 0.07 | -0.07 to 0.10 | 0.493 |
| Infant height (cm) (reference group: control) | |||||
| Self-care training group | 0.39 | 0.29 | -0.1 | -0.62 to 0.54 | 0.894 |
| Mother’s age, y | -0.01 | 0.03 | -0.04 | -0.07 to 0.04 | 0.690 |
| Mother’s BMI, kg/m2 | 0.01 | 0.04 | 0.03 | -0.07 to 0.10 | 0.761 |
| Infant head circumference (cm) (reference group: control) | |||||
| Self-care training group | -0.58 | 0.25 | -0.02 | -0.56 to 0.44 | 0.820 |
| Mother’s age, y | 0.005 | 0.026 | 0.021 | -0.04 to 0.05 | 0.848 |
| Mother’s BMI, kg/m2 | 0.009 | 0.039 | 0.026 | -0.06 to 0.08 | 0.816 |
Comparison of Neonatal Anthropometric Indices Between Study Groups Based on the General Linear Model (ANCOVA Test)
| Variables | Unstandardized Coefficient (B) | Standard Error | Exp (β) | CI of β | P Valuea |
|---|---|---|---|---|---|
| Cesarean delivery (reference group: control) | |||||
| Training group | -2.62 | 0.60 | 0.073 | 0.022 to 0.23 | <0.001 |
| Mother’s age (y) (reference: ≤ 25) | |||||
| 26 - 30 | 1.55 | 0.87 | 4.72 | 0.84 to 26.2 | 0.076 |
| > 31 | 0.37 | 0.84 | 1.45 | 0.27 to 7.6 | 0.656 |
| Mother’s BMI (kg/m2) (reference: ≤ 24.9) | |||||
| 25 - 29.9 | 0.75 | 0.70 | 2.11 | 0.53 to 8.41 | 0.286 |
| ≥ 30 | 1.27 | 0.78 | 3.56 | 0.76 to 16.62 | 0.106 |
| Preterm labour (reference group: control) | |||||
| Training group | -1.13 | 0.59 | 0.32 | 0.10 to 1.02 | 0.055 |
| Mother’s age (y) (reference: ≤ 25) | |||||
| 26 - 30 | 0.194 | 0.838 | 1.21 | 0.23 to 6.27 | 0.817 |
| 31 and higher | 0.232 | 0.822 | 1.26 | 0.25 to 6.31 | 0.778 |
| Mother’s BMI (kg/m2) (reference: ≤ 24.9) | |||||
| 25 - 29.9 | -1.23 | 0.694 | 0.292 | 0.07 to 1.13 | 0.076 |
| ≥ 30 | -0.33 | 0.717 | 0.71 | 0.17 to 2.91 | 0.639 |
| Macrosomia (reference group: control) | |||||
| Training group | -2.83 | 1.08 | 0.058 | 0.007 to 0.492 | 0.009 |
| Mother’s age (y) (reference: ≤ 25) | |||||
| 26 - 30 | -0.004 | 1.07 | 0.996 | 0.122 to 8.15 | 0.853 |
| ≥ 31 | -0.799 | 0.99 | 0.450 | 0.057 to 3.53 | 0.627 |
| Mother’s BMI (kg/m2) (reference: ≤ 24.9) | |||||
| 25 - 29.9 | 1.75 | 1.19 | 5.76 | 0.55 to 59.7 | 0.142 |
| ≥ 30 | 2.42 | 1.22 | 11.30 | 1.03 to 124.0 | 0.047 |
Comparison of Cesarean Delivery, Preterm Labor, and Macrosomia Between Study Groups Based on the Multivariate Logistic Regression Model
5. Discussion
The results of this study showed that the frequency of cesarean delivery and macrosomia were significantly lower in the experimental arm compared to the control arm. However, there was no significant difference between the two arms in terms of other studied variables.
Results of the present study are consistent with the findings of the Hawkins et al. research. In the Hawkins et al. study the rate of macrosomic infants (21.9% vs. 29.5%) and large for gestational age (LGA) (23.1% vs. 34.4%) was significantly lower in the self-monitored arm than in the physician-monitored arm (18). In addition, the present study results are consistent with the findings of the Landon et al. research. Landon et al. determined the effect of self-monitoring of blood glucose and nutritional counseling on gestational outcomes. There was a significant decrease in the intervention group in terms of infant fat mass, macrosomia, dystocia, and cesarean delivery (22). Homko et al. (23) studied the efficacy of self-monitoring of diabetes on gestational outcomes and self-efficacy. There was no significant difference between two arms in terms of the sense of self-efficacy, preterm delivery, birth weight, Apgar score, macrosomia, cesarean delivery, and birth injury. The results of this study are not consistent with the findings of our research except in terms of birth weight. In the present study, the weight of newborn infants in the experimental arm was higher, but no significant difference was observed between the two arms. Low sample size can be a possible reason for the insignificant difference between the two groups. Also, in the Homko et al. study, only women with fasting a blood glucose of less than 95 mg/dL were recruited into the study.
A possible reason for the effectiveness of self-care training on pregnancy consequences can be related to improving the mother’s behaviors in regards to self-monitoring of blood glucose level. Based on a research in the field of peer training on self-care actions among individuals with gestational diabetes showed that overall mean score and subscales scores of self-care behaviors in the intervention arm were significantly higher compared to the control arm. In addition, the fasting and after-meal blood glucose levels were significantly lower in the intervention arm than in the control arm (24). On the other hand, decreasing the macrosomia rate can be related to less weight gain among woman with well self-care and continuous blood glucose monitoring (25).
In the present study, the rate of cesarean section was lower in the experimental arm than in the control arm. This decrease can be attributed to the reduction of macrosomia, and increased rate of vaginal delivery might be due to the provision self-care training with an emphasis on physical activity. A systematic study also suggested that physical activity during pregnancy can reduce cesarean delivery (26). Training reinforce awareness and self-care behaviors in individuals and hence reduce fasting blood glucose and HbA1c levels (15).
Observance of all principles of clinical trials, including randomization and allocation concealment, is one of the strengths of this study. One of the limitations of this research was the small sample size; perhaps with a larger sample size, effect of the training program on the outcomes would be better evaluated. Therefore, it is recommended that further researches be performed with larger sample sizes. In addition, anthropometric indices of the neonates were based on the report given by the maternity hospital. This could be another limitation of the present study. It is suggested that the effects of other educational methods such as using software and the internet on the self-care behaviors of mothers with gestational diabetes be investigated in future studies. It is also suggested that a similar study on pregnant women with overt diabetes be carried out.
5.1. Conclusions
The results showed that self-care training can affect the frequency of macrosomia and cesarean delivery in women with gestational diabetes; however, it did not affect other outcomes of pregnancy. Considering the prevalence of gestational diabetes and its short and long term effects on maternal and fetal health, appropriate training can potentially decrease the potential complications of gestational diabetes by improving self-care behaviors.