1. Background
Diabetes is well-known as the silent epidemic of the present century and as one of the biggest health problems in all countries (1). According to the modern lifestyle, diabetes prevalence is growing in both developed and developing countries (2, 3). In the 21st century, diabetes has turned into a major challenge in community health management, and it is especially more serious in the Middle East (3, 4). More than 230 million individuals worldwide currently have diabetes (5). The Eastern Mediterranean and the Middle East with a population of 592 million have the highest incidence rate in the world. Also, this region has the highest rate of death caused by diabetes in males and females (6, 7). Iran, as a Middle Eastern country, has 3.5 million diabetic patients (8). On the other hand, diabetes is the cause of many physical and mental disorders. Sexual disorders are one of the chronic mental complications of diabetes. However, sexual disorders are mainly assessed based on several sexual dysfunctions, such as erectile dysfunction ejaculation disorders and decreased sexual desire in males, and sexual arousal, orgasm, satisfaction, and pain in the females (9). In fact, sexual dysfunction is three times more in diabetic individuals compared with healthy individuals (10, 11). Reduced sexual desire is also high in people with diabetes (12). Many studies have been performed on sexual dysfunction in diabetic males and females (13, 14). Sexual disorders in diabetic males are present in 50% of cases before the age of 60, yet their prevalence appears to be lower in diabetic females (15). Besides, sexual disorders in males and females are divided to two main psychological and physical groups (genetic causes, hormonal disorders, autonomic neuropathy, atherosclerosis, and vascular failure) (16, 17). In diabetic females, vascular, neurological, and psychological problems are the main causes of reduced sexual desire, vaginal lubrication and secretions, arousal disorders, orgasmic problems, and dyspareunia (18). In male diabetic patients, neurological disorders and psychiatric problems reduce erection or decrease the number of sperms (19, 20). Although marital satisfaction and sexual function are undesirable in diabetic patients, the assessment of sexual dysfunction and marital dissatisfaction in females and males with type 2 diabetes is questionable.
2. Objectives
Considering the lack of comprehensive studies in this regard in southern Iran, the present study was conducted to investigate sexual dysfunction and marital dissatisfaction among males and females with type 2 diabetes in Zarand, Kerman.
3. Methods
This study was a cross-sectional research that was conducted on individuals referring to health care centers of Zarand city, Kerman province, Iran during year 2015. They were selected by using available sampling in accordance with the medical ethics code IR.KMU.REC.1395.121. This study used a total of 480 individuals, which enrolled within two healthy (n = 120 males and females) and diabetic groups (n = 120 diabetic males and females). The criteria for entering the study included: Non-pregnant women that were at the pregnancy age, being able to read and write, being married, having at least three years of marital life, not having a chronic illness in the partner, such as depression, history of diabetes greater than one year, not affected by retinopathy, kidney failure, amputation, and non-development of cerebrovascular accidents, and cardiac events over the past 12 months.
3.1. Instruments
Files and questionnaires of patients comprised of two parts. The first part included a demographic questionnaire that determined age, physical complications caused by diabetes, such as heart diseases (blood pressure and electrocardiography), nephropathy (urine analysis and Albuminuria) retinopathy (ophthalmology examination and microvascular injuries), and neuropathy (peripheral and autonomic examination). The second part contained questions regarding sexual dysfunction. Rosen female sexual function index (2000) contains 19 items with six subscales of sexual desire, sexual arousal, vaginal moisture, orgasm, dyspareunia, and sexual satisfaction, scored between two and 36. The highest score of this scale shows the best sexual function and less pain (21). Male sexual function: Participants completed questions one to five of the international index of erectile function (IIEF) questionnaire, which is a multidimensional scale for assessing erectile dysfunction (22). The primary outcomes were erectile function score, calculated as the sum of questions one to five from the IIEF with a maximum score of 25. Also, the respondents’ reduced sexual desire and sexual dysfunction at erection in males and vaginal lubrication in females were measured by using the Laumann questionnaire (22, 23). Meanwhile, the researchers tried to do their best to diminish their distrust through assuring them about anonymity and confidentiality of their data and overall analysis of the questionnaires. In addition, the questionnaires were completed in a private room by the subjects with no direct observation of the researcher.
3.2. Data Analysis
The collected data were analyzed using SPSS 16 software. Variables with Shapiro-Wilk values P > 0.05 were considered normal and used from independent samples t-test for comparing them between the two groups. The frequency and relative frequency of demography characteristics were presented based on health situation (healthy and diabetic). The presence or absence of diabetic complications were presented and compared between diabetic males and females using chi-square test and differences with P ≤ 0.05 were considered significant.
4. Results
The mean age of the respondents in the healthy and diabetic female group were 43.29 ± 4.77 and 42.65 ± 4.4, respectively (Table 1) and the mean age of the respondents in the healthy and diabetic male group were 43.87 ± 5.68 and 42.99 ± 4.68, respectively (Table 1). There were no significant differences between healthy and diabetic females on age (P = 0.29), employment condition (P = 0.6), educational level (P = 0.89), place of residence (P = 0.24), economical condition (P = 0.18), and cigarette or alcohol consumption (P = 0.43, Table 1). Also, there were no significant differences between healthy and diabetic males regarding age (P = 0.19), employment condition (P = 0.18), place of residence (P = 0.52), economical condition (P = 0.22), and cigarette or alcohol consumption (P = 0.31, Table 2). A higher number of healthy males with college or higher educational level were reported than diabetic males (P < 0.001, Table 2). On the other hand, the number of healthy and diabetic males were statistically significant at different educational levels in this study (P < 0.05, Table 2).
| Variables | Health Situation | P Valueb | |
|---|---|---|---|
| Healthy | Diabetic | ||
| Age, y, mean ± SD | 43.29 ± 4.77 | 42.65 ± 4.4 | 0.29 |
| Job | 0.6 | ||
| Employed | 64 (53.3) | 68 (56.7) | |
| Housewife | 56 (46.7) | 52 (43.3) | |
| Educational level | 0.89 | ||
| Primary school | 28 (23.3) | 28 (23.3) | |
| High school | 36 (30.1) | 31 (25.8) | |
| Diploma | 34 (28.3) | 38 (31.7) | |
| College or higher | 22 (18.3) | 23 (19.2) | |
| Place of living | 0.24 | ||
| City | 61 (50.8) | 52 (43.3) | |
| Village | 59 (49.2) | 68 (56.7) | |
| Economic situation | 0.18 | ||
| Goodc | 70 (58.3) | 80 (66.7) | |
| Moderatec | 50 (41.7) | 40 (33.3) | |
| Cigarette or alcohol consumption | 8 (6.6) | 6 (5) | 0.43 |
aValues are expressed as No. (%) unless otherwise indicated.
bP < 0.05 was considered statistically significant. Chi- square test and t-test were used for comparing these variables.
cGood economic situations: family income per mouth > 4 × 106 Rial; moderate economic situation: families receive income per mouth between 1.5 - 4 × 106 Rial.
| Variables | Health Situation | P Valueb | |
|---|---|---|---|
| Healthy | Diabetic | ||
| Age, y, mean ± SD | 43.87 ± 5.68 | 42.99 ± 4.68 | 0.19 |
| Job | 0.18 | ||
| Employed | 82 (68.3) | 72 (60) | |
| Housewife | 38 (31.7) | 48 (40) | |
| Educational level | < 0.001 | ||
| Primary school | 21 (17.5) | 38 (31.7) | |
| High school | 25 (20.8) | 30 (25) | |
| Diploma | 36 (30) | 41 (34.2) | |
| College or higher | 38 (31.7) | 11 (9.1) | |
| Place of living | 0.52 | ||
| City | 58 (48.3) | 53 (44.2) | |
| Village | 62 (51.7) | 67 (55.8) | |
| Economical situationc | 0.22 | ||
| Good | 84 (70) | 75 (62.5) | |
| Moderate | 36 (30) | 45 (37.5) | |
| Cigarette or alcohol consumption | 41 (34.16) | 46 (38.33) | 0.31 |
aValues are expressed as No. (%) unless otherwise indicated.
bP < 0.05 was considered statistically significant. Chi- square test and t-test were used for comparing these variables.
cGood economic situations: family income per mouth > 4 × 106 Rial; Moderate economic situation: families receive income per mouth between 1.5 - 4 × 106 Rial.
In the present study, the diabetic males and females suffered from diabetes for 4.75 ± 2.5 and 4.88 ± 2.57 years, respectively (Table 3). Overall, 96.7% of males and 97.5% of females had more than 140 mg/dL two-hour blood sugar, therefore, they received both Met and GBC pins. Moreover, there were 5.8% males and 3.3% females with heart problems. Overall, 8.3% of diabetic males and 6.7% of diabetic females had liver disorders, whereas, 5.8% of males and 5% of females were observed by nephropathy. Retinopathy was the most common diabetic complication (29.2% of males and 20% of females), which were observed in this study. Furthermore, 13.3% of diabetic males and 12.5% of females suffered from neuropathy (Table 3).
| Variables | Diabetic Individual, N = 240 | P Value | |
|---|---|---|---|
| Men, N = 120 | Women, N = 120 | ||
| Duration of diabetesb, y | 4.75 ± 2.5 | 4.88 ± 2.57 | 0.7 |
| Medication, No. (%) | |||
| Met + GBC | 116 (96.7) | 117 (97.5) | 0.7 |
| Biochemicalb | |||
| FBS, mg/dL | 153.25 ± 65.85 | 148.22 ± 63.7 | 0.55 |
| HbA1c, % | 10.05 ± 2.84 | 10.42 ± 2.37 | 0.28 |
| 2-hour blood sugar, mg/dL | 146.1 ± 2.19 | 146.33 ± 1.87 | 0.37 |
| Insulin, µU/mL | 224.24 ± 84.83 | 211.04 ± 77.38 | 0.21 |
| Physical, No. (%) | |||
| Heart problems | 7 (5.8) | 4 (3.3) | 0.35 |
| Liver problem | 10 (8.3) | 8 (6.7) | 0.62 |
| Nephropathy | 6 (5) | 7 (5.8) | 0.78 |
| Retinopathy | 35 (29.2) | 24 (20) | 0.1 |
| Neuropathy | 16 (13.3) | 15 (12.5) | 0.85 |
Abbreviations: GBC, glibenclamide; Met, metformin.
aValues are expressed as mean ± SD unless otherwise indicated.
bP < 0.05 was considered statistically significant. Chi- square test and t-test were used for comparing these variables.
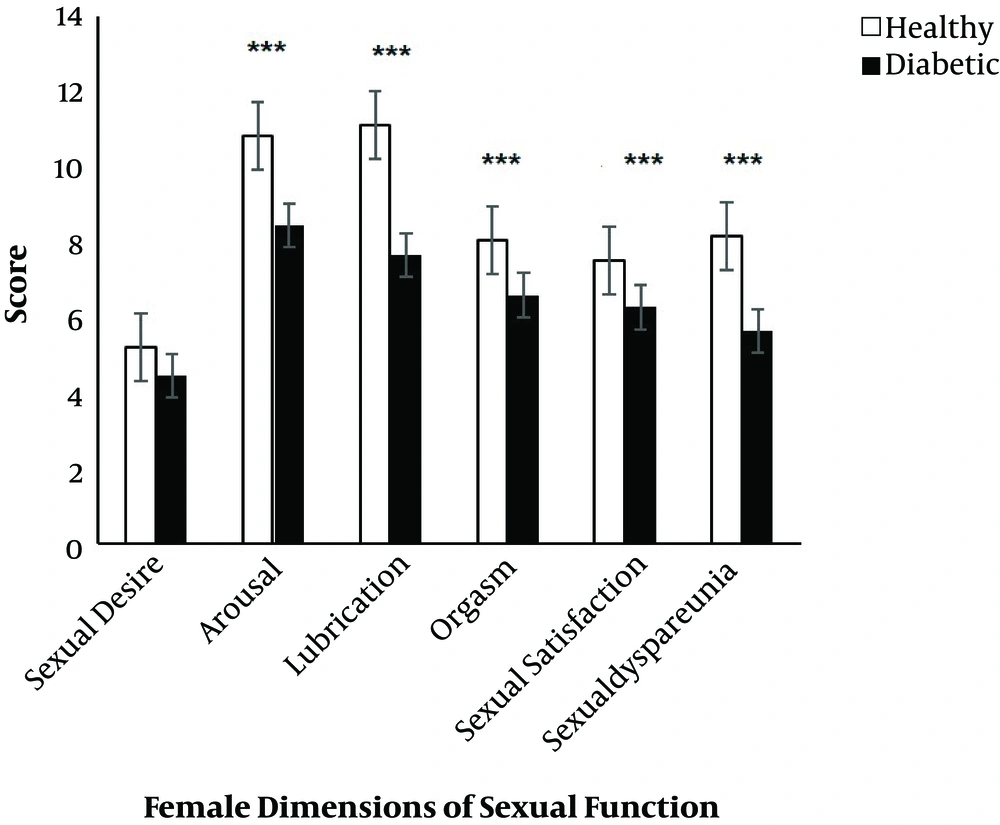
Different dimensions of sexual function in diabetic and healthy females are presented in Figure 1. The female sexual function indices were scored between two to 36, and the highest score showed the best sexual function and less pain. There was no significant difference in sexual desire between healthy and diabetic groups. Sexual arousal was significantly (P < 0.001) lower in the diabetic group compared with healthy individuals. In addition, sexual lubrication (P < 0.001), orgasm (P < 0.001), satisfaction (P < 0.001), and dyspareunia (P < 0.001) scores were significantly higher in the healthy group in comparison diabetic individuals (Figure 1).
The mean and standard error of scores of different dimensions of sexual function (sexual desire, arousal, lubrication, orgasm, sexual satisfaction and sexual dyspareunia) in diabetic and healthy women. *** Present significant differences (P < 0.001) between two groups by Mann-Whitney U test.
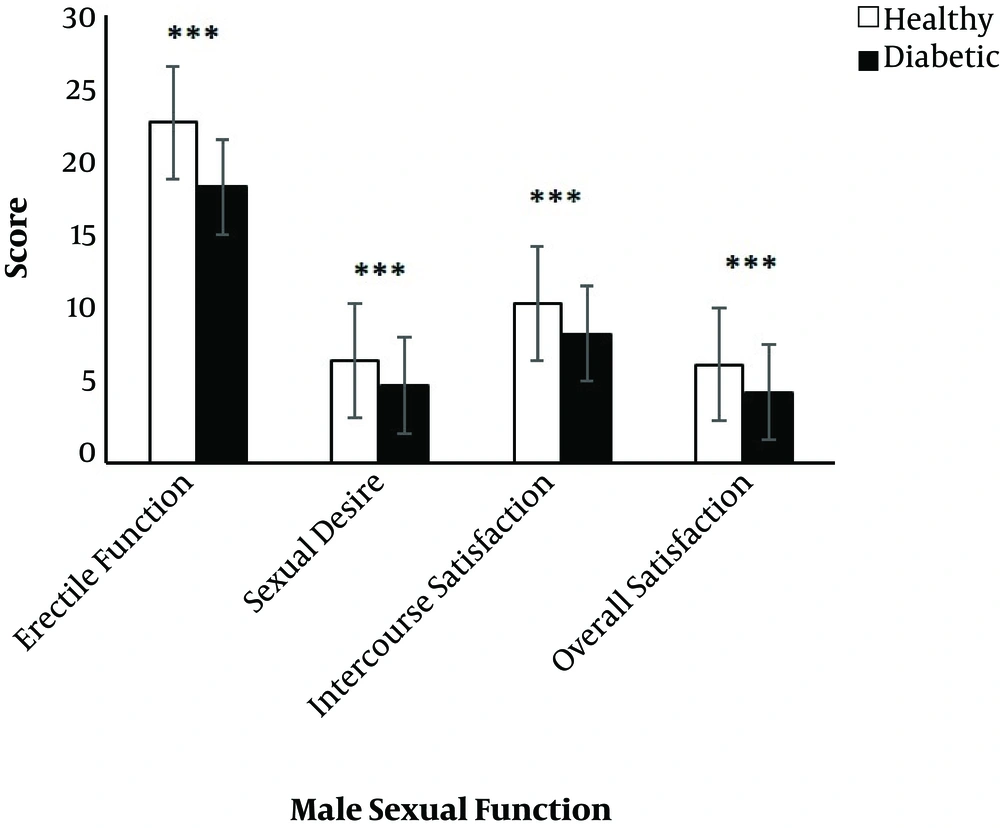
In Figure 2, the four main domains of male sexual function in healthy and diabetic males with IIEF questionnaire are presented. Severe erectile dysfunction was observed significantly (P < 0.001) greater in diabetic than healthy groups. However, sexual desire, the amount of intercourse satisfaction and overall satisfaction were significantly (P < 0.001) lower in diabetic males compared to healthy males.
Generally, 41 diabetic individuals (17.08%) from all diabetic participants had impaired sexual function, 29 of which (70.73%) were male (with higher rates in males than females, P < 0.05). In addition, 12 diabetic patients (5%) had decreased sexual desire, 66.6% of which were diabetic males.
5. Discussion
This study was conducted to investigate the relationship between type 2 diabetes, sexual function, and marital dissatisfaction in males and females with type 2 diabetes in Zarand, Kerman. The basic characters in diabetic and healthy subjects indicated that the incidence of type 2 diabetes was not affected by educational and economic conditions, cigarette or alcohol consumption and place of residence in females, yet type 2 diabetes incidence was significantly lower in males with college or higher educational level. As diabetes mellitus is related to some sociodemographic factors within the Iranian population (24), the researhcers could not find any data regarding educational, economical situations, urban-rural differences and cigarette or alcohol consumption prevalence of type 2 diabetes in Zarand, Kerman. The results conducted on educational level of males were in line with previous investigations (25, 26). Rahmanian et al. reported that diabetes is most prevalent in Iranian individuals with lower educational level (26). In addition, a higher prevalence of diabetes mellitus in an urban area of different Iranian provinces has usually been reported compared with rural areas (27, 28).
In addition, some diabetic complications, such as nephropathy, neuropathy, and retinopathy were observed between diabetic individuals. Vafaeimanesh et al. presented significant correlations between sexual dysfunctions and retinopathy and nephropathy. They suggested that chronic problems, such as retinopathy and nephropathy can be considered as risk factors for sexual dysfunction (21, 29).
The comparison of the mean scores of sexual functions in type 2 diabetic and healthy individuals indicated that type 2 diabetes can influence sexual dysfunction and marital satisfaction in both males and females. These findings were in line with previous studies (30-32). In addition, the current findings indicated a significantly lower score of sexual function and marital satisfaction in diabetic males compared to diabetic females. It was shown that its prevalence is higher in diabetic males and it is estimated to influence 20% to 85% of diabetic males, while, this issue is probably less common in diabetic females (29). Seid et al. reported 35% to 90% of diabetic males have erectile dysfunction that can be the result of high blood glucose-induced penile microvascular injuries (33). As marital dissatisfaction increases, physical and mental pressures can reduce one’s sexual and physical health and ability (34). In addition, sexual dysfunction and marital dissatisfaction could lead to divorce and end up in the breakdown of marital life (35).
5.1. Conclusions
Based on the results of this study and other studies, it could be suggested that type 2 diabetes causes chronic sexual dysfunction and reduced sexual desire in both genders. Therefore, counseling and control of type 2 diabetes in females at gestational age and males at different ages are recommended.