1. Background
The healthcare sector is one of the most important areas in public service delivery and an index for social welfare and development, which its economic analysis is very important for policy-makers (1). Among all healthcare sectors and systems, the treatment sector and hospital system, as one of the most important and influential sectors of the society, play an important role in providing vital services and promoting public health (2, 3). A major share of national health expenditures of gross national product (GNP) is spent on hospitals (4). In the developing countries, hospitals account for about 50% to 80% of healthcare expenditures and employ a large part of trained healthcare professionals (3). National Statistics in Iran show that about 40% of healthcare expenditures in public sector are for hospitals (5). Moreover, with the implementation of the Health Sector Evolution Plan since May 2014 and its impact particularly on hospitals, the share of healthcare expenditure and hospitals of GNP even raised (6). Since in each healthcare system, hospitals are the main consumers of healthcare resources (7), the issue of current hospitals’ expenditures without quality reduction is considered by national healthcare systems in most countries. In addition, hospitals, especially in the developing countries, are characterized by inefficient resource management, low productivity, non-professional service provision, and inflexible hierarchical organizational structure (8). Such poor management in hospitals usually leads to the waste of resources; while they can be spent on provision, expansion of access, and improvement of the quality of services (9). In this regard, improvement in productivity and efficiency is considered as the main option for expenditure planning and waste minimization in hospitals (10). Hospitals in Iran are no exception, and the strategies of hospital managers should inevitably approach the reduction of expenses and increase of productivity.
Any attempts to improve productivity, as the major responsibility of the executive agencies, especially in hospitals as the largest and costliest operation unit of the healthcare sector, need a reasonable analysis of input and output changes that should be associated with careful planning to improve efficiency and effectiveness (11, 12). Therefore, measuring the amount of changes in productivity and identifying its effecting factors as a cornerstone of analyses and decisions lead to taking corrective measures to improve productivity (12). It is difficult for policy-makers and planners to make decisions if productivity is not measured and practically, the made decisions are not scientific and applicable, and in a wider context, results in wasting the valuable healthcare resources (13). Therefore, an appropriate standard to measure productivity is of great importance in the decision-making process of authorities (14). Two general approaches to measure productivity are data envelopment analysis (DEA) and indices methods. In the Kendrick-Creamer index, the total factor and marginal productivity of hospitals, as well as the productivity growth rate are measured by estimating the production function. In DEA, the productivity of hospitals can be measured using the Malmquist Index, a powerful tool to monitor the productivity of hospitals. In addition, in this method, productivity changes are divided into changes caused by efficiency and technology (15-17). The Malmquist index is applicable to multi-input multi-output environments without price information, and assesses productivity in a one-year or multi-year period (18). There are few studies on measuring the productivity of hospitals by the Malmquist and the Kendrick-Creamer indices. For example, Nabilou et al. in a case study in Iran using DEA method concluded that technological efficiency changes have the greatest influence on productivity decrease compared with other factors (17). In another study by Kirigia et al., in Angola hospitals, the results showed that technological changes were the main cause of decrease in total factor productivity in the studied period (19).
2. Objectives
The current study aimed at determining the changes in productivity and measuring productivity in hospitals affiliated to Lorestan University of Medical Sciences, Iran from 2010 to 2016, using DEA model based on the Malmquist productivity index and the Kendrick-Creamer index. It is expected that health planners and managers be familiar with the process of productivity and the most important influencing factors, and accordingly take the effective measures to optimally allocate resources and improve the productivity.
3. Methods
The current retrospective study with descriptive-analytical design employed surgical interventions as output variable in the employed model, and the psychiatric hospital was excluded from the study due to lack of surgery ward. In addition, the two newly established Shaheed Rahimi and Shahid Valian hospitals in Aligudarz City were also excluded from the study due to lack of records in the defined period. Finally, all of the hospitals affiliated to Lorestan University of Medical Sciences (N = 12), except for the three abovementioned hospitals, were studied from 2010 to 2016. In order to observe ethical considerations, the results were provided with relevant numbers assigned to each hospital. The data and information required by the studied hospitals and the Treatment Department of Lorestan University of Medical Sciences were collected using a researcher-made checklist. According to previous studies, a combination of the most important and common inputs and outputs was selected to estimate the changes in total factor productivity. The data included inpatient and outpatient admissions, the number of surgeries, and bed occupancy rate as outputs, and the number of active beds, doctors, nurses, and other personnel as inputs (18, 20-23).
Data analysis was conducted in three phases as follows: in the 1st phase, after collecting data from the hospitals, the DEA method was employed to study hospitals from 2010 to 2016. There are several DEA models of which three classic models are extensively used to measure relative efficiency and productivity. The Malmquist index is one of the most significant models to measure and analyze five factors including total technical efficiency changes, technological efficiency changes, managerial efficiency changes (or pure technical efficiency), scale efficiency changes, and total factor productivity changes (ΔTFP) for hospitals based on DEA. The Malmquist productivity index is defined using distance functions as follows:
Where,
Total productivity changes = Managerial efficiency changes × Scale efficiency changes technological changes
If the Malmquist index, with minimization of production factors assumption, is less than 1, it indicates better performance; but if the Malmquist index is greater than 1, it implies the performance worsening in the study period (17).
The Deap 2.1 software was employed to measure the Malmquist productivity index.
Since DEA standard approach includes a relative measurement in which the efficiency and productivity scores of hospitals are calculated in comparison with those of the best hospitals in the model, there is always at least one hospital that achieves the performance score of 1 with 100% efficacy; and if the number of variables used to measure the relative efficiency of hospitals increases, the number of efficient hospitals also increases, which can lead to inability to identify hospitals with poor and good performances (21). Therefore, the main DEA models, due to the lack of full ranking between the efficient units, do not support comparison between efficient units and, accordingly, the need to rank effective units is inevitable (24, 25). In the 2nd phase, in order to rank the efficient hospitals, the Anderson-Peterson (AP) coefficient, which is a non-relative performance, was employed. Another approach to rank efficient hospitals noted in other studies was the evaluation of the number of referrals to each unit and assessing hospitals` positive/negative slacks to such an extent that hospitals with more referrals as well as the ones with negative slacks were more efficient, and there was usually a general agreement between this method and the AP coefficient to identify hospitals with super-efficiency (21).
In the 3rd phase, the Kendrick-Creamer index was used to measure TFP. To calculate the index, the elasticity of total production with respect to the factors of production should be estimated and for this purpose, the production function should be estimated first. To estimate the production function, Frontier 4.1 software was employed, and accordingly, it was a Cobb-Douglas function. In this function, the coefficients of each of the production factors indicate its corresponding elasticity.
Function of production:
In this phase, using the elasticity of the production factors, the TFP of the studied hospitals were calculated with the Kendrick- Creamer index. The mathematical form of the Kendrick-Creamer function is as follows:
where TPi is the total productivity of hospital; Oi output, which in the current study was bed occupancy rate; P, the number of physicians; N, the number of nurses; B, the number of active beds; op, the number of other personnel; ep, elasticity of physicians; en, elasticity of nurses; eb, elasticity of active beds and eop, elasticity of other personnel in the studied hospitals.
Productivity growth, based on the Kendrick- Creamer index, was calculated using the following equation:
In the abovementioned equation, if all the production values are related to the physical quantity of the production factors, the equation value is zero, and the production growth is totally attributed to the growth of production factors. But if the value is positive, it indicates increased productivity in the studied hospitals (4).
Finally, the marginal productivity of production factors; i.e., the amount of change in total production per unit of change in the application of the production factor, was estimated using the production function; and the elasticity obtained for the inputs was estimated by the following equations:
where Q/P is the minor (medium) productivity for the physician; Q/N, the minor productivity (medium) for the nurse; Q/B, the minor productivity (medium) for the active bed; Q/OP, the minor productivity (medium) for other personnel; α, the elasticity output with regards to the physicians; β, the elasticity output with regards to the nurses; γ, the elasticity output with regards to active beds, and ρ, the elasticity output with regards to other personnel.
4. Results
Table 1 provides a summary statistic about input and output variables of the hospitals over the study period.
| Hospital | Inpatient Admissions | Outpatient Admissions | Number of Surgical Procedures | Bed Occupancy Rate | Number of Active Beds | Doctors | Nurses | Other Personnel |
|---|---|---|---|---|---|---|---|---|
| 1 | 9282 | 142796 | 3893 | 17404 | 91 | 22 | 66 | 67 |
| 2 | 10776 | 92812 | 510 | 37093 | 135 | 46 | 167 | 91 |
| 3 | 3957 | 6505 | 1129 | 8064 | 42 | 16 | 41 | 55 |
| 4 | 31268 | 282337 | 92198 | 40722 | 338 | 98 | 237 | 238 |
| 5 | 4239 | 4256 | 1157 | 9198 | 46 | 13 | 36 | 46 |
| 6 | 9800 | 105272 | 655 | 31033 | 109 | 47 | 146 | 103 |
| 7 | 12053 | 109977 | 3795 | 24566 | 116 | 40 | 82 | 97 |
| 8 | 4953 | 101801 | 2438 | 8458 | 48 | 13 | 71 | 83 |
| 9 | 15648 | 131403 | 7221 | 33410 | 167 | 34 | 232 | 134 |
| 10 | 7975 | 20674 | 5453 | 23518 | 103 | 36 | 132 | 125 |
| 11 | 11227 | 11747 | 4305 | 34401 | 119 | 26 | 124 | 89 |
| 12 | 5445 | 46202 | 3600 | 13705 | 56 | 19 | 53 | 81 |
| Mean | 10552 | 87982 | 10531 | 23464 | 114 | 34 | 116 | 101 |
The results of estimating the TFP using the Malmquist index and analysis of its changes based on the factors affecting it are shown in Tables 2 and 3. In the current study, the year 2010 was considered as the base year.
| Year | Technical Efficiency | Technological Developments | Managerial Efficiency | Scale Efficiency | Total Productivity Changes |
|---|---|---|---|---|---|
| 2011 | 1.025 | 0.949 | 0.996 | 1.029 | 0.973 |
| 2012 | 1.001 | 1.07 | 0.996 | 1.005 | 1.072 |
| 2013 | 0.996 | 0.891 | 0.985 | 0.982 | 0.861 |
| 2014 | 1.044 | 1.107 | 0.998 | 1.046 | 1.155 |
| 2015 | 1.025 | 1.106 | 1.01 | 1.015 | 1.134 |
| 2016 | 0.942 | 1.035 | 0.967 | 0.974 | 0.975 |
| Average period | 1 | 1.023 | 0.992 | 1.008 | 1.023 |
| Hospital Code | Technical Efficiency | Technological Developments | Managerial Efficiency | Scale Efficiency | Total Productivity Changes |
|---|---|---|---|---|---|
| 1 | 1 | 0.957 | 1 | 1 | 0.957 |
| 2 | 0.963 | 0.987 | 0.967 | 0.996 | 0.951 |
| 3 | 1.077 | 1.098 | 1 | 1.077 | 1.183 |
| 4 | 1 | 0.915 | 1 | 1 | 0.915 |
| 5 | 1.035 | 1.026 | 1 | 1.035 | 1.062 |
| 6 | 1.002 | 1.022 | 1 | 1.002 | 1.024 |
| 7 | 0.961 | 1.05 | 0.973 | 0.988 | 1.009 |
| 8 | 1 | 1.059 | 1 | 1 | 1.059 |
| 9 | 1 | 1.052 | 1 | 1 | 1.052 |
| 10 | 0.959 | 1.06 | 0.962 | 0.996 | 1.016 |
| 11 | 0.997 | 1.007 | 1 | 0.997 | 1.004 |
| 12 | 1.01 | 1.061 | 1 | 1.01 | 1.071 |
| Mean | 1 | 1.023 | 0.992 | 1.008 | 1.023 |
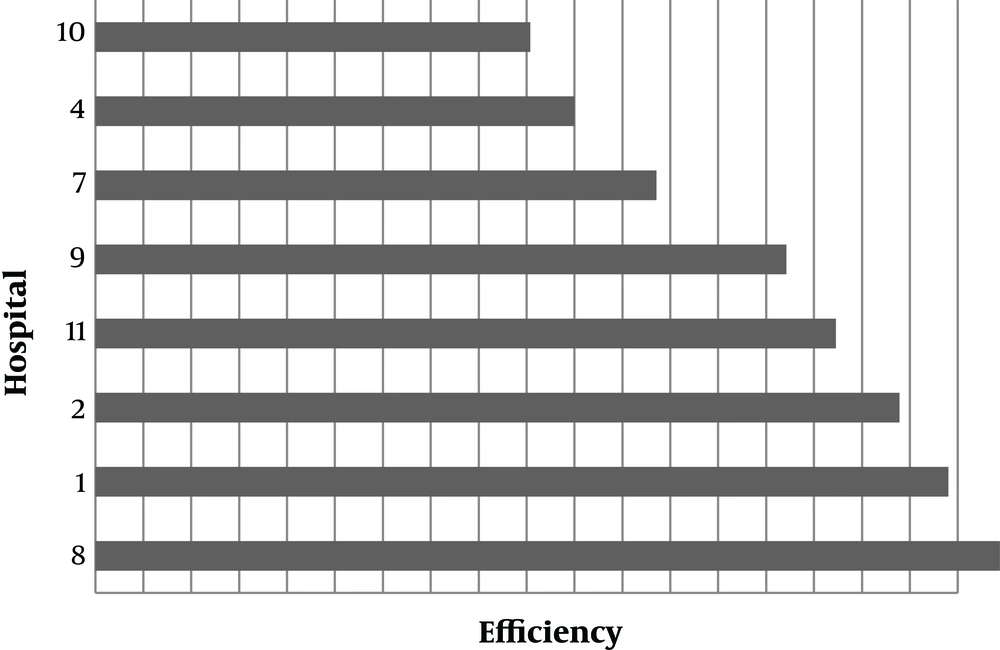
According to Table 3, only three hospitals showed productivity improvements, while nine other hospitals showed a decrease in productivity. Also, in terms of total productivity changes, hospitals 3 and 4 had the worst and best performances, respectively. The analysis of changes in the Malmquist productivity index, by the influencing factors, showed that on average, over the study period, the highest and lowest impacts on productivity were attributed to technological and technical efficiency changes, respectively. In the second phase, the ranking of eight hospitals is illustrated in Figure 1.
According to Figure 1, the lowest productivity score belonged to Hospital 10, which was not referenced to any other hospitals and had positive slacks.
In the next phase, the Kendrick-Creamer index was employed to measure TFP. To calculate this index, the production function was first estimated and accordingly, the Cobb-Douglas function was detected; the results are shown in Table 4. In this function, the coefficients of each of the production factors indicate its corresponding elasticity.
| Variable | Coefficient | Standard Error | T-Statistic |
|---|---|---|---|
| β0 | 5.2 | 0.605 | 8.7 |
| β1 | 0.05 | 0.112 | 0.45 |
| β2 | 0.34 | 0.082 | 4.2 |
| β3 | 0.63 | 0.153 | 4.2 |
| β3 | 0.063 | 0.075 | 0.83 |
| LR | 32 | ||
| MLE | 108 | ||
The results of TFP and productivity growth of the studied hospitals as well as the marginal productivity of inputs are shown in Tables 5 and 6.
| Hospital | Technical Efficiency | Productivity Growth | Total Productivity |
|---|---|---|---|
| 1 | 0.82 | 0.19 | 204.8 |
| 2 | 0.89 | 0.15 | 251.8 |
| 3 | 0.69 | 0.107 | 180.6 |
| 4 | 0.41 | -0.07 | 130.7 |
| 5 | 0.82 | 0.07 | 211.7 |
| 6 | 0.89 | 0.12 | 247.9 |
| 7 | 0.83 | 0.025 | 228.8 |
| 8 | 0.58 | 0.024 | 145 |
| 9 | 0.64 | 0.11 | 176.8 |
| 10 | 0.74 | 0.19 | 202.8 |
| 11 | 0.95 | 0.033 | 285.05 |
| 12 | 0.90 | 0.04 | 242.5 |
| Mean | 0.77 | 0.083 | 209.06 |
| Hospital | Active Bed | Nurse | Physician | Other Personnel |
|---|---|---|---|---|
| 1 | 119.7 | 127.7 | 40.94 | 10.8 |
| 2 | 172.6 | 76.4 | 45.2 | 17.2 |
| 3 | 119.4 | 66.6 | 28.3 | 28.04 |
| 4 | 78.2 | 55.4 | 19.7 | 8.9 |
| 5 | 126.6 | 87.7 | 37.3 | 10.7 |
| 6 | 178.2 | 71.9 | 33.2 | 12.6 |
| 7 | 134.1 | 97.9 | 30.6 | 36.2 |
| 8 | 110.5 | 40.7 | 33.96 | 16.02 |
| 9 | 126.1 | 50.6 | 50.4 | 6.7 |
| 10 | 143.4 | 62.3 | 34.7 | 17.9 |
| 11 | 18.9 | 99.6 | 67.3 | 11.85 |
| 12 | 153.7 | 108.3 | 35.2 | 25.42 |
| Mean | 137.1 | 78.8 | 38.1 | 16.87 |
Table 5 showed that the mean TFP of the studied hospitals, calculated using the Kendrick-Creamer index, was 209.06 over the study period; i.e., the output per unit of the production factor in all the studied hospitals was 209.06 on average. According to Table 5, the highest negative productivity growth was observed in Hospital 4, and the highest positive growth productivity was observed in hospitals 10 and 1, using the Kendrick-Creamer index during the studied period.
Table 6 also shows that the marginal productivity of physicians, nurses, active beds, and other personnel inputs during the study period was 38.1, 78.8, 137.1, and 16.87, respectively. In other words, for per unit of change in the application of the above inputs, the change in total production was 38.1, 78.8, 137.1, and 16.87, respectively. The results of calculating the marginal productivity of each of the production factors indicated that, on average, the highest marginal productivity of the physicians was 67.3 in Hospital 11, and the lowest was 19.65 in Hospital 4. Also, the highest marginal productivity of nurses in the studied period was 127.7 in Hospital 1 and the lowest was 40.7 in Hospital 8. The highest marginal productivity of active beds was 182.9 in Hospital 11 and the lowest was 78.2 in Hospital 4. The highest marginal productivity of other personnel was 36.18 in Hospital 7 and the lowest was 6.7 in Hospital 9.
5. Discussion
The importance of high expenditures in healthcare sector in the past decades was the basis of studies on productivity and efficacy since the results of such studies were effective in the better management of resources, and consequently the reduction of expenditures. Therefore, studies can be used as an instrument for policy-making in the healthcare area. In this regard, the current study aimed at evaluating the productivity of hospitals. Evaluation of the performance of the hospitals enables the authorities to identify the optimal points and potentials of each hospital, and by comparing the performance of hospitals with those of the successful ones, identify their promotion capacities.
Of the 12 studied hospitals from 2010 to 2016, only three showed increased productivity, and in nine of the hospitals, productivity had a decreasing trend. Changes in the productivity of hospitals ranged from 0.915 to 1.183; while it was 0.861 to 1.155 in the studied period. Afonso and Fernandes, after the evaluation of the efficiency and productivity of 68 general hospitals in Portugal, from 2000 to 2005 and using the Malmquist index, indicated a slight increase in productivity, and the mean TFP for the studied hospitals ranged 0.917 to 1.109; in addition, such fluctuations were also observed in the studied years (26).
Also, on average during the study period, changes in the efficiency of the scale and technology had a negative impact on TFP, while managerial efficiency changes had a positive impact on TFP. The study on the productivity of Eastern Ethiopian hospitals showed that on average, the scale of production reduced productivity by 1.2% (27). The results of the study in Zambia showed that the size of hospitals was the main cause of inefficiency (28). The mean TFP changes, based on the findings obtained by DEA, was 1.023 during the study period, which indicated a productivity decrease by 2.3% during the same period. The low productivity rate, as reported in the current study, warns top university authorities to take serious measures and put the issue of better management of hospital resources in the agenda. For the hospitals with high productivity, investment in new technologies may be reasonable in order to improve productivity. In contrast to the hospitals in Lorestan province, hospitals in some countries had productivity growth. The decrease in the productivity of hospitals in the current study was further influenced by technological changes, which indicated that the hospitals did not properly utilize the advanced medical technology. Therefore, it is suggested holding training courses for employees in proper application of new technologies in hospitals that technology changes are the main reason for their productivity decrease.
Technological advancement plays an important role in increasing the productivity of large-scale hospitals (29). In line with the results of the current study, most studies in the developing countries, e.g., the study by Kirigia et al., in Angola and the study by Yawe in Uganda highlighted the technological changes as the main cause of TFP reduction (19, 30). Also, the study by Pang and Wang showed that technological changes had the largest share in productivity changes (31). A study by Torabipour et al. in Iran estimated the mean of productivity changes in Ahvaz city hospitals as 1.214, which represented a 2.4% reduction in productivity, of which technological changes had the most significant effect on this trend (32). Data analysis showed that 25% of hospitals could not use their resources to optimize their output. According to Kirigia et al., the inefficiency meant that the studied hospitals had surplus input or output shortage compared with the efficient frontier hospitals (19). The surplus inputs indicate that provincial policymakers and authorities can reorganize their resources to reduce inefficiencies and the hospitals expenditures. If inefficiencies are eliminated or reduced, additional resources can be used to improve healthcare quality, invest on new technologies, and train staff in the required expertise. Therefore, it is recommended to use the results of the current study as well as other similar ones for future planning and allocation of resources in hospitals. One of the important results of the current study was to determine the enhancement capacity of the studied hospitals based on the type of returns-to-scale (RTS) to such an extent that hospitals working under decreasing returns-to-scale (DRS) conditions (four hospitals) should reduce their inputs, since under such circumstances, with the assumption of a constant output rate, increased input is greater than increased output in the hospital. Therefore, since the long-run marginal cost and consequently the long-run total cost increase, reduction of the amount of input is economically justified. Based on the findings, capacity enhancement was applicable in four (33%) hospitals with increasing return to scale (IRS). Therefore, in order to improve healthcare services in other medical centers of Iran, more precise planning can be initiated by employing such techniques aimed at minimizing the consumption of resources. In Kerman province, Iran, 53.8% of hospitals had a constant RTS, 30.7% DRS, and 15.3% IRS (33). Therefore, it can be concluded that enhancement capacity was more evident in Lorestan province hospitals. In order to eliminate the scale inefficiencies in hospitals with IRS, two methods are available: first, the integration of close and small hospitals that is not very logical due to access restrictions; second, implementation of complementary projects through which the production scale is increased in small hospitals in order to optimize the capacity of such hospitals. To overcome the scale inefficiency, in the cases in which the scale inefficiency is the outcome of DRS, the overall hospital structure should be reviewed, and the best option is to adjust human and capital resources (34). Therefore, policymakers should avoid entering unwanted resources into hospitals in order to prevent accumulation of human and capital resources in non-economic production areas and, consequently, the final negative production.
The results of the stochastic frontier analysis (SFA) showed that the mean technical efficiency of the hospitals in the current study was 0.77; lower than those of other countries (35-37). In other words, the potential to raise productivity in the studied hospitals without an increase in the executive expenditures and new hiring was 23%. In fact, 23% of production factors played no role in the production process. Accordingly, there was a high potential for efficacy improvement in Lorestan province hospitals. This rate was 10% in the hospitals covered by Social Security Organization (20), and 4% in the hospitals affiliated to Tehran University of Medical Sciences based on the study by Farzianpour et al. (38). The efficiency of hospitals in Lorestan province was lower than those of other provinces of Iran (7). A study in the Netherlands showed that the mean inefficiency of hospitals in the country was 16%, resulting in €1.5 million loss annually in the public hospitals (39). A study in Iran showed that less than 60% of hospitals in the country were technically efficient, and therefore, they had low productivity, since the efficiencies of all the departments are directly related to the trend of productivity in hospitals (40). One way to increase technical efficiency is to reduce the length of stay and increase hospital size. Masayuki showed that larger hospitals were more efficient. By doubling the size of the hospital, productivity increases by 10 % (41). Of course, the effects of the mean stay of patients should be controlled simultaneously. Also, based on the results of the Kendrick-Creamer index, Hospital 4 had the highest negative growth rate and hospitals 10 and 1 had the highest positive growth rate over the studied period. In line with the results of the study by Hadian et al. (2), the elasticity of production in the current study with regards to the active beds factor was greater than that of other factors, which indicated the greatest effect of this factor on the production rate of hospitals compared with other assessed factors. The finding was expected and indicated that policymakers and hospital managers can improve efficiency by better management of hospital beds and taking measures to increase bed occupancy rate.
The current study had some limitations. The most important limitation of the current study was that due to lack of access to information, the authors could not examine some factors affecting the efficiency and productivity of hospitals; for example, database did not provide information on patient safety, patient satisfaction, and quality of healthcare. Kiadaliri et al. suggested that improvement of the process of data collection in the databases of the Iranian hospitals by a standard approach may affect the value of studies in this regard (7). Second, the authors had no access to reliable documents and information regarding case-mix. Therefore, hospitals admitting and treating non-complicated cases may have higher efficacy and productivity scores. Another limitation of the study was that the sample size was small and limited just to Lorestan province; therefore, the results cannot be generalized to other regions and organizations.
5.1. Conclusions
The authors found evidence that hospitals could not use their resources to optimize their output. Therefore, the current study results had several policy proposals for managers and policymakers. To achieve more widespread and rapid hospital productivity growth, policymakers should avoid capital accumulation in non-economic production. In order to increase the productivity and efficiency of hospitals, strategies such as increasing the managerial authorities to better control and more accurately monitor inputs and employments based on the hospital needs (both in terms of number and expertise) and saving on input resources (e g, optimal allocation of beds) can be helpful. It is also suggested using this method in hospitals with maximum productivity to measure productivity in different departments in order to compare the performance of different departments of a hospital to plan for better performance. Also, access to data and financial information, real human resources, and the expenditures of each department provides a platform for further studies on the various aspects of hospital productivity.