1. Background
Endometriosis is a common disease in women of reproductive age and it can present diverse symptoms, including pain and infertility (1). Despite various medical treatments, laparoscopy is the gold standard diagnostic method that provides simultaneous therapeutic management (2, 3). Although laparoscopy has great benefits compared with open procedures, postoperative pain remains an important complication (4).
Postoperative pain after laparoscopic procedures is usually a diffuse pain in abdomen, shoulder, and back that is suggested to originate the stretching of the intra-abdominal cavity (5) and the residual carbon dioxide (CO2) in the peritoneal cavity that may cause peritoneal inflammation and phrenic nerve irritation (6). Shoulder pain is also a frequent complaint (35% to 80%) after gynecological laparoscopic surgery (7), resulting from peritoneal insufflation, mainly in exaggerated Trendelenburg position (8). Thus controlling the postoperative pain is essential, and insufficient postoperative pain control can prolong the recovery time and decrease patient satisfaction (9).
The efficacy of various analgesics, including bupivacaine, levobupivacaine, clonidine, and naloxone have been widely investigated on postoperative pain (10). Research has revealed the ease of use and safety of local anesthetic agents that directly act on the target tissue (11, 12) and are suggested to efficiently reduce postoperative pain after laparoscopic surgery (13). Dexmedetomidine (DEX) is a α2-adrenergic agonists similar to clonidine that provides sedation, analgesia, anxiolysis, analgesia, and sympatholysis (14). The DEX has a greater α2-receptor affinity and shorter half-life than clonidine (15) and the specificity of DEX to α2- receptors is of great interest in regional anesthesia. Moreover, the addition of DEX, as an adjuvant to bupivacaine, is proven to be effective in postoperative pain relief in various procedures such as cesarean section (16), abdominal hysterectomy (17), and other gynecologic surgeries (18, 19). However, as far as the authors are concerned, it has not been confirmed in the laparoscopic procedure for patients with endometriosis.
2. Objectives
The present study aimed to assess the analgesic property of DEX combined with bupivacaine administered intraperitoneally and compare it with the intraperitoneal administration of bupivacaine alone and normal saline in patients undergoing laparoscopy for endometriosis.
3. Methods
In the present randomized, clinical trial study, patients who were candidates of laparoscopic surgery for endometriosis in Rasoul-e-Akram Hospital, a tertiary- Medical University Center in Tehran, were recruited from January 2016 to May 2017.
After approval of the Institutional Ethics Committee (IR, IUMS, rec, 1395, 27252), STATA software was used for estimating the sample size. The test power was equivalent to 80.
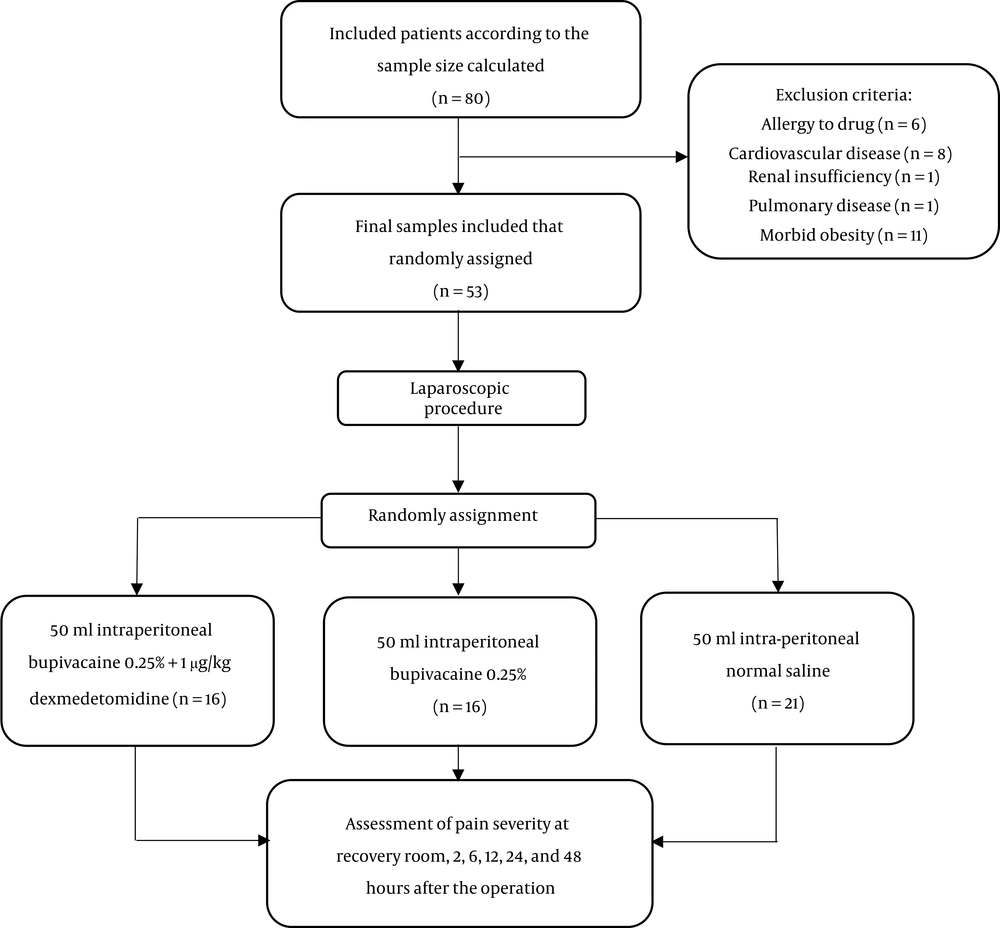
Fifty-three patients who met the inclusion criteria were randomly divided into three. This study was three-blinded, thus the researcher, patient, and statistical analyst were blinded to the allocation of the three groups. All patients signed the written informed consent form before the intervention.
Inclusion criteria for this study were the age between 20 - 48 years, being scheduled for elective laparoscopic surgery for the diagnosis of endometriosis, and the American Society of Anesthesiologists (ASA) class 1 and 2. Each patient with a positive history of allergy to local anesthetics or DEX, cardiac disease, renal or hepatic failure, severe pulmonary disease; in addition, pregnant and comorbid obese patients were excluded from the study. Finally, 53 patients were included in the study (Figure 1).
During operation, the subjects were monitored for vital signs using electrocardiogram, pulse-oximeter, capnography, and noninvasive blood pressure. The patients received 2 µg/kg fentanyl + 1.5 mg midazolam intravenously (IV) and 2 mg/kg propofol + 0.2 mg/kg cisatracurium were applied to anesthesia induction. Anesthesia was maintained with 100 µg/kg propofol. End Tidal (ET) CO2 was maintained between 35 - 40 mmHg.
Laparoscopic procedures were performed using standard direct entry with 11-mm port at the umbilicus, while for those who required difficult deep infiltrative endometriosis interventions, 5.5 mm and 11 mm ports were placed in the bilateral lower quadrants and suprapubic zone, respectively. The patients were placed in 15 - 20°C Trendelenburg’s position. During the procedure, the intra-abdominal pressure was maintained at 12 - 14 mmHg. A minimum sample size of 14 was calculated to be needed in each group to achieve a study power of 80% with regard to P value less than 0.05 as a significant result. In this regard, the subjects were randomly (using randomization table) divided into three groups, including Group 1 (n = 21) received 50 mL intraperitoneal normal saline as negative control, group 2 (n = 16) received 50 mL intraperitoneal bupivacaine 0.25% as positive control, and group 3 (n = 16) received 50 mL intraperitoneal bupivacaine 0.25% plus 1 µg/kg DEX. At the end of the laparoscopic procedure, study drugs prepared in a sterile syringe were given to the researcher who was blinded to the nature and characteristics of the drugs. After homeostasis was achieved, intraperitoneal administration was guided by a camera on the port site and pelvic peritoneal surface before removal of the port in Trendelenburg’s position. Then CO2 was removed using compression of the abdomen manually at the end of the procedure. The pain severity was assessed at the recovery room, 2, 6, 12, 24, and 48 hours after the operation, by visual analogue scale (VAS) in which zero score corresponds to ‘no pain’ and 10 corresponds to ‘maximum’ or ‘the worst pain’. Rescue analgesia consisted of 50 mg suppository of diclofenac sodium, administered to patients who reported VAS ≥ 3 or on the patient’s request. Total analgesic consumption was recorded within 48 hours.
All analyses were performed by SPSS software version 17.0 (Chicago, USA). Data were presented as mean and standard deviation (SD) for quantitative variables and number (percentage) for categorical variables. One-way analysis of variance (ANOVA) test followed by post-hoc test were used to compare quantitative variables across the groups. Kruskal-Wallis H test was employed to compare variables with non-parametric distribution. The chi-square test was also used to determine the association between categorical variables. The P value of less than 0.05 was considered statistically significant.
4. Results
Mean age ± SD of the patients included in the study was 32.50 ± 7.21. There was no significant difference in terms of age and body mass index (BMI) among the three study groups (P = 0.2; Table 1).
| Intraperitoneal Normal Saline, Group 1 (N = 21) | Intraperitoneal Bupivacaine Group 2 (N = 16) | Intraperitoneal Bupivacaine + DEX, Group 3 (N = 16) | P Valueb | |
|---|---|---|---|---|
| Age, y | 31 ± 6.82 | 32.06 ± 8.47 | 34.93 ± 6.06 | 0.2 |
| BMI, kg/m2 | 23.87 ± 4.68 | 25.62 ± 3.56 | 26.34 ± 4.13 | 0.1 |
Demographic Characteristics of the Study Population, According to the 3 Groupsa
There was one case of hysterectomy due to deep infiltrative endometriosis (DIE) in group 1, one in group 2, and two cases in group 3. There were no significant differences with respect to the type and duration of the surgery between the groups (P = 0.4; Table 2).
| Intraperitoneal Normal Saline, Group 1 (N = 21) | Intraperitoneal Bupivacaine, Group 2 (N = 16) | Intraperitoneal Bupivacaine + DEX, Group 3 (N = 16) | P Valueb | |
|---|---|---|---|---|
| DIE resection | 10 (47.6) | 10 (62.5) | 11 (68.8) | 0.4 |
| Endometrioma resection | 10 (47.6) | 5 (31.3) | 3 (18.8) | 0.4 |
| Hysterectomy | 1 (4.8) | 1 (6.3) | 2 (12.5) | 0.4 |
The Frequency of Type of Procedures, According to the 3 Groupsa
The postoperative VAS scores were significantly lower in group 3 than other groups in the recovery room, and 2, 6, 12, 24 and 48 hours after the surgery (P < 0.001). However, there was no significant difference between the groups of 1 and 2 (Table 1). Furthermore, total VAS in the first 24 hours was significantly lower in group 3 than the two other groups (P < 0.001). The VAS score was greater in group 2 compared with group 1; however, no significant difference (P > 0.99).
The fewest mean of total diclofenac suppositories was used in group 3 compared with the other two groups (P < 0.001) (Table 3).
| Intraperitoneal Normal Saline, Group 1 (N = 21) | Intraperitoneal Bupivacaine, Group 2 (N = 16) | Intraperitoneal Bupivacaine +DEX, Group 3 (N = 16) | P Value | |
|---|---|---|---|---|
| Diclofenac consumption | 2 ± 1 | 3.8 ± 0.98 | 1.18 ± 1.16 | < 0.0001 |
Total Analgesic Consumption in 48 Hours Postoperatively
We observed no significant difference in the site of maximum pain across the three groups (P = 0.3). The incidence of shoulder pain was lower in group 3 without statistically significant difference (33.3%, 50%, and 31.3% in groups 1, 2, and 3, respectively) (P > 0.05).
According to our findings, 5 patients in group 3 and 1 patient of in group 1 did not need any analgesic (Table 2).
5. Discussion
The results of the present study on the assessment of postoperative VAS scores showed significantly less pain in group 3 (DEX + bupivacaine) than group 2 (bupivacaine) and group 1 (normal saline) in the recovery room, and 2, 6, 12, 24, and 48 hours after the surgery (P < 0.001) and fewer rescue analgesic requirement in group 3. While the longest time to the first rescue analgesic requirement was in group 2. As pain relief after gynecologic laparoscopic interventions has remained a critical issue, researchers broadly investigated to determine the highest safety and tolerance to analgesic techniques among patients who planned for surgery (20). Our study demonstrated that intraperitoneally distillated DEX with bupivacaine significantly attenuated postoperative pain and declined postoperative rescue analgesic consumption compared with intraperitoneally administered bupivacaine alone or normal saline. Meta-analysis studies on minor gynecologic procedures (such as tubal ligation) confirmed the efficacy of intraperitoneal bupivacaine on postoperative pain (21). However, research on patients undergoing minimally invasive gynecologic surgery has provided diverse results on the efficacy of intraperitoneal administration of bupivacaine on postoperative pain control. In this regard, Rivard et al. has found it efficient (19), while other researchers did not find any improvement in the pain control, narcotic use, length of hospital stay, or the level of patients’ satisfaction following the use of bupivacaine (22, 23), which is consistent with our study findings. It may also reflect this fact that intraperitoneal normal saline and intraperitoneal bupivacaine alone have similar effectiveness, as reported by Esmat and colleagues (6). As hypothesized, the local anesthetic agent administration causes visceral afferent signaling, and modification of visceral nociception that will block sodium channels (24). Thus recent studies have evaluated the efficacy of the combination of intraperitoneal bupivacaine with another local anesthetic agent. Ahmed et al. showed that intraperitoneal instillation of meperidine or DEX in combination with bupivacaine 0.25% significantly decreased the postoperative analgesic requirements and the incidence of shoulder pain compared with bupivacaine 0.25% alone in patients undergoing laparoscopic gynecological surgeries (25). Memis et al. also demonstrated that administrating a combination of clonidine and bupivacaine via intra-peritoneal root could provide more effective analgesia compared to bupivacaine alone during the early postoperative period (26). Narasimham and Rao also found that the intraperitoneal administration of bupivacaine alone or combined with DEX or tramadol could relieve procedure-related following after laparoscopic cholecystectomy (27). The prolonged sedation of DEX is attributed to its longer half-life than clonidine (28). The results of the above-mentioned studies are consistent with the results of the present study, confirming the efficacy of the combination of DEX with another analgesic; however, the surgical type and the adjuvant analgesic differ among studies.
Similar to the results of the present study, other researchers have also revealed that intraperitoneal administration of DEX with bupivacaine, in laparoscopic gynecologic surgeries, was associated with a reduction in VAS and postoperative analgesic requirements in the hours of surgery (29-31). In addition to these results, the present study showed maximum painlessness at 48th hour postoperatively in DEX plus bupivacaine group.
Additionally, there was no statistically significant difference in the place of maximum pain in 24 hours and administration of local anesthetic had no efficiency on trocar site pain. As far as the authors are concerned, the combination of DEX with bupivacaine has not been studied on the laparoscopic procedure for the treatment of endometriosis and the origin of postoperative pain depends on the surgical technique. Therefore, further studies on the pain origin of this specific type of surgery may elucidate the mode of analgesia in the present study.
The strengthening point of the present study was comprised of a combination of gynecologic procedures such as retroperitoneal dissection, endometrioma, endometriotic nodule resection, and hysterectomy; all patients were postoperatively planned for similar pain regimen, suggesting the differences in pain controlling due to administrating intra-peritoneal local anesthetics. Also, the extended follow-up period of 48 hours (compared to 24 hours in previous studies) is the other strength of our study. The limitation of our study included small sample size and all surgeries were not performed by a single surgeon; however, the surgical techniques and equipment were unified.
As there are few studies on using a combination of DEX and bupivacaine, further studies considering different dosages and roots of local anesthetics are required to compare this approach of analgesia with other regional techniques with the goal of achieving more benefit with regard to postoperative pain relief along with minimized adverse effects following laparoscopic surgeries.
5.1. Conclusions
Our study showed that the administration of the intraperitoneal local anesthetic agent, DEX, in combination with bupivacaine can effectively reduce the need for prescribing postoperative analgesic drugs as well as decrease postoperative pain severity in minimally invasive laparoscopic surgery.