1. Background
Healthy adults need 7.5 to 8.8 hours of sleep per night (1). Sleep deprivation is the most common health problem among night shift nurses (2). Gold et al. reported that 30.9% of the nurses had experienced a near-miss (an unplanned event) while driving home after a night shift during the preceding year (3). Impaired alertness and decreased attention (4), sleepiness, and fatigue (5) are the major adverse effects of sleep deprivation, which can lead to road traffic collisions (RTCs) (6).
A study indicated most of the RTCs among night shift health cares occurred between 8 AM and 9 AM in the morning after a night shift when they were driving home (7).
Based on findings of the previous studies, night time napping is an effective method to increase alertness, improve cognitive performance (8), and reduce sleepiness (9). Planned napping at the workplace is one way to reduce fatigue and sleepiness among health care workers (10). Night shift nurses frequently experience sleepiness, however, planned napping can decrease both sleepiness (11, 12) and the risk of RTC (13) when driving home after shifts. Nurses taking a nap during their night shifts is reported to diminish sleepiness while driving home after their shifts (13). Silva-Costa et al. reported that the efficacy of napping during night shifts is similar to that of night time sleep at home (14).
A study by Gillberg showed that an hour nap at 4:30 AM can improve performance at the end of the shift (7 AM) compared to no nap (15). Taking a nap at 2 AM and 3 AM is reported to improve the reaction time and reduce fatigue after the shift (11, 16, 17).
A main challenge of shift work is the conflict between displaced work hours and an internal body clock in the brain that produces circadian rhythms; it exists in the suprachiasmatic nuclei of the hypothalamus (18). This body clock produces a signal that results in a pronounced 24-hour alternation in all physiological and psychological functions such as body temperature, alertness, sleepiness, and hormone levels. Melatonin has a high point at ~04:00 AM and a low point at ~16:00 PM, and is closely associated with temperature and alertness (19). The circadian adjustment of shift workers is slow, about one hour every day. If no adjustment occurs, work at the circadian nadir will be performed at low levels of physiological activation, alertness, and behavioral efficiency (20).
It has been shown that more than 90% of RTCs are due to human errors and driver behavior (21, 22). Thus, traffic psychology tests have become highly important to assess safe driving (21).
2. Objectives
In this study, by using a validated computerized test system (23), we examined the relationship between two nap times (00:00 - 03:00 AM versus 03:00 - 06:00 AM) and the psychomotor skills required for safe driving after a night shift for the first time in Iran. These skills include attention, concentration, reactive stress tolerance, perceptual speed, peripheral perception, visual pursuit ability, visuo-motor coordination, and time-movement anticipation.
3. Methods
3.1. Participants and Procedure
A cohort study was conducted on 19 night shift female nurses working at the Sina Hospital in Tehran (Iran) during 2015 and 2016 through an announcement in all departments. In this hospital, night shift nurses work 12 hours from 7 PM to 7 AM, and they can take three hour naps from 00:00 to 03:00 AM or from 03:00 to 06:00 AM by their choice.
Participants in our study also chose their nap times based on their preferences. Eight participants chose to nap from 00:00 to 03:00 AM (group one) and 11 chose to nap from 03:00 to 06:00 AM (group two).
Criteria for inclusion were as follow: healthy female nurses aged 20 to 40; at least one year of work experience; holding a driver’s license; being a frequent driver, and working only one shift during the 24 hours preceding the study.
Nurses attended a training session to practice with the traffic psychological assessment battery of Vienna test system (VTS). Then, on the day of the study, they completed the VTS test set one hour before the beginning of the night shift at 6 PM. Then, they completed the same tests again at the end of the night shift in the following morning at 7 AM before returning home. The participants were asked to abstain from drinking coffee or taking any medication that could affect their sleep during the test sessions.
3.2. Data Collection Tools
The demographic and circadian type inventory (CTI) questionnaires were used for data collection. CTI questionnaire measures rhythm, stability, and amplitude of circadian rhythm. Flexible/rigid (FR) states the flexibility of sleeping habits. Rigid types denote to those who cannot sleep at irregular hours. Languid/vigorous (LV) explains the amplitude of circadian cycles. Languid types cannot overcome sleepiness in the condition of lack of sleep, while vigorous types are more alert during the day and need less sleep than languid types. Vigorous and flexible types show better adaptation with shift work (24).
Also, traffic psychological battery of the Vienna test system was used for assess psychomotor ability of driving after night shift. The eight VTS tests used in this study were as follow: the determination test (DT); cognitrone test (COG); reaction time test (RT); adaptive tachistoscopic traffic perception test (ATAVT); peripheral perception test (PP); visual pursuit test (LVT); two hand coordination test (2HAND); and time-movement anticipation test (ZBA). The validity and reliability of the tests have been reported in several studies (23, 25). Detailed explanation of the tests is provided in the Supplementary File Appendix 1.
3.3. Statistical Inference
To better understand the results, we defined scores as follows:
Scores obtained before the shift (SOBS); scores obtained after the shift (SOAS); changes in SOAS, compared to SOBS (CABS), and difference of CABS between the two study groups (DCABS). An interpretation was made based on the comparison of DCABS between the two groups. Therefore, the DCABS was calculated for every test and compared between the two study groups, using independent student’s t-test and Wilcoxon Rank test.
All statistical analyses were performed using IBM SPSS Statistics, version 20.0. Significance level was set at 0.05.
3.4. Ethical Consideration
The study protocol was approved by the Research Ethics Committee of Tehran University of Medical Sciences and in accordance with the ethical guidelines of the 1975 Declaration of Helsinki (reference number: IR TUMS.REC.2015.1984- 7/12/2015). All the participants provided written informed consent.
4. Results
Table 1 demonstrates the comparison of baseline characteristics between the study groups. There was no statistically significant difference in the baseline characteristics of the study groups.
| Characteristics | Group 1, 00 - 03 AM Nap, (N = 8) | Group 2, 03 - 06 AM Nap, (N = 11) | P Value |
|---|---|---|---|
| Age | 29.5 ± 4.14 | 28.73 ± 4.10 | 0.69b |
| Driving experience | 7.00 ± 2.51 | 5.27 ± 4.34 | 0.33b |
| Sleep duration within last 24 hours | 8.87 ± 1.96 | 8.73 ± 2.41 | 0.89b |
| Marital status | 0.66c | ||
| Single | 5 (62.5) | 7 (63.3) | |
| Married | 3 (37.5) | 4 (36.4) | |
| Circadian rhythm | |||
| Flexible | 2 (25) | 2 (18.2) | 0.57c |
| Rigid | 6 (75) | 9 (81.8) | |
| Langui | 1 (12.5) | 1 (9.1) | 0.68c |
| Vigorous | 7 (87.5) | 10 (90.9) | |
| RTC history | 0.17c | ||
| No | 4 (50) | 9 (81.8) | |
| Yes | 4 (50) | 2 (18.2) |
Baseline Characteristics of the Study Groupsa
Table 2 presents the mean CABS in the study groups as well as the DCABS.
| Tests | Variables | Unit | CABS, Type of Nap | DCABS, Mean (SE) | P Value | |
|---|---|---|---|---|---|---|
| Group 1, 0:00 - 03:00 AM | Group 2, 03:00 - 06:00 AM | |||||
| ZBA (time-movement anticipation) | Median deviation time SQRT transformed | s | -0.26 ± 0.21 | 0.05 ± 0.21 | -0.31 (0.097) | 0.005a |
| 2 Hand (viso motor coordination) | Overall mean duration (2Hand1) | s | 0.46 ± 6.30 | -4.41 ± 5.33 | 4.89 (2.6) | 0.087a |
| Overall percent error duration (2Hand2) | - | -0.11 ± 1.86 | -0.24 ± 1.19 | 0.11 (0.69) | 0.88a | |
| ATAVT (perceptual speed) | Overview | - | 2.25 ± 3.92 | -0.64 ± 2.54 | 2.89 (1.48) | 0.068a |
| DT (choice reaction time) | Correct response (DT1) | n | 2.37 ± 12.96 | 2.9 ± 12.53 | 6.25 (-15.81) | 0.68a |
| Incorrect response (DT2) | n | 0.25 ± 3.10 | -0.40 ± 4.88 | 0.43 (1.91) | 0.82a | |
| Omitted response (DT3) | n | -0.12 ± 2.95 | -1.70 ± 3.97 | 2.69 (2.08) | 0.21a | |
| Median reaction time (DT4) | s | -0.01 ± 0.02 | -0.002 ± 0.04 | -0.01 (0.01) | 0.47a | |
| LVT (visual orientation) | Score [based on viewing times] (LVT1) | - | 0.25 ± 1.67 | 0.30 ± 3.23 | 0.16 (1.12) | 0.89a |
| Score [based on working times] (LVT2) | - | 0.87 ± 1.73 | 0.60 ± 2.80 | 0.58 (2.34) | 0.44b | |
| PP (peripheral perception) | Field of vision (PP1) | ° | -4.26 ± 20.30 | 1.2 ± 4.73 | 0.16 (13.37) | 0.8b |
| Tracking deviation (PP2) | - | 0.8 ± 0.96 | -0.11 ± 0.84 | 0.23 (0.94) | 0.49b | |
| RT (simple reaction time) | Mean reaction time (RT1) | ms | -14.37 ± 63.65 | 8.7 ± 48.71 | -20.28 (25.34) | 0.43a |
| Mean motor time (RT2) | ms | -1.5 ± 28.97 | 31.10 ± 80.49 | 15.58 (62.04) | 0.49b | |
| Cog (selective attention) | Sum hits (Cog1) | n | -0.13 ± 1.25 | -0.30 ± 0.95 | -0.26 (1.05) | 0.72b |
| Correct rejections (Cog2) | n | -0.13 ± 1.36 | 0.40 ± 1.71 | 0.16 (1.50) | 0.60b | |
| Mean time correct rejection (Cog3) | s | 0.09 ± 0.40 | 0.05 ± 0.28 | 0.06 (0.15) | 0.72a | |
The Mean Score Change (CABS) of Psychomotor Abilities of Driving Variables as well as the Mean Differences (DCABS) Among the Study Groups
The mean CABS in case of the “median deviation time” (ZBA test) was negative in group one (-0.26 ± 0.21) and positive in group two (0.05 ± 0.21). The DCABS was statistically significant in case of this variable (P = 0.005).
The DCABS in the subtests of other VTS tests (COG, LVT, RT, DT, ATAVT, PP, and 2Hand) failed to reach significant level (P > 0.05) (Table 2).
5. Discussion
The present study aimed at determining the change in the psychomotor skills of driving in nurses after a night shift, according to their nap time during their shift.
Each participant passed the tests before and after the night shift. The CABS is influenced by fatigue and sleepiness, as well as the learning curve mechanism. Therefore, if one group shows less improvement (or deterioration) in the test scores obtained after the shift compared to the other group, then, we can conclude that the timing of the nap taken by that group was not as effective as the other group.
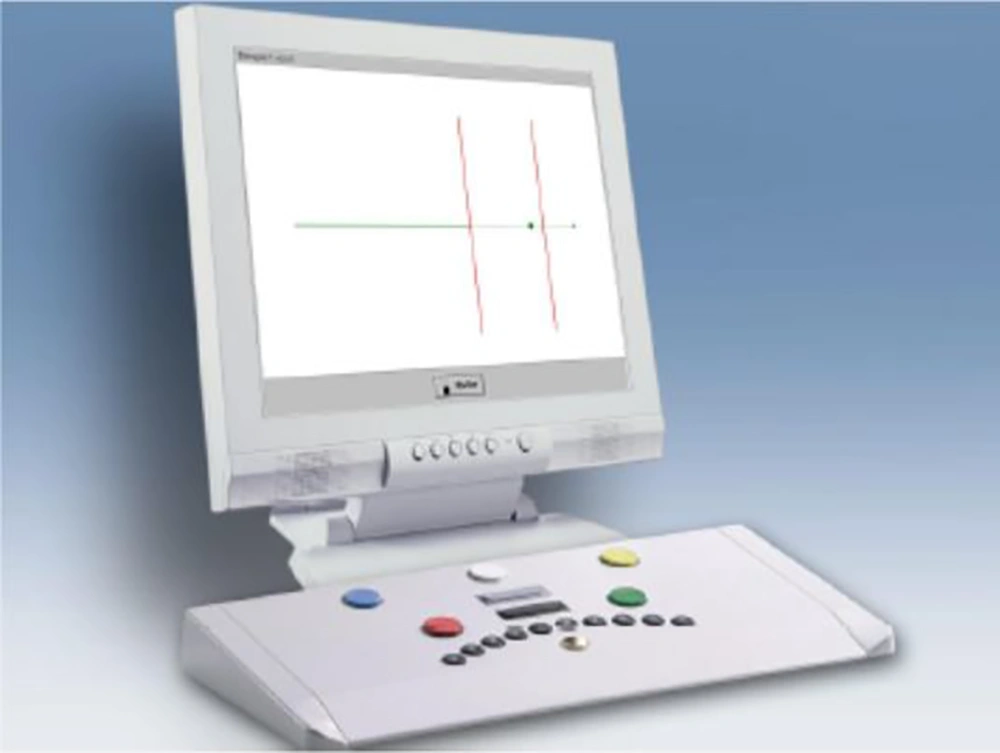
Based on the results, improvement in the participants’ ability of time-movement anticipation was significantly higher in group one, compared to group two in the ZBA test. The ZBA test could be related to the ability of estimating the time to collision of two vehicles that are moving at a constant speed (26). In this test, a ball moving slowly appears on the monitor. Then, in an unexpected moment, this ball disappears and two red lines appear; one line is positioned at the point where the ball has disappeared, and the other is considered the target line. The participant should press one button the second he/she thinks the ball crosses the target line (Figure 1).
The advantage of a 00:00 to 03:00 nap time compared to 00:03 to 00:06 may be explained by sleep inertia, a physiological state characterized by a deficit of motor skills directly after rapidly waking up and damaged alertness may affect physical and mental performance (27, 28). Another explanation could be the quantity and quality of sleep during nap opportunity. A study of nurses revealed that those who napped from 00:00 to 03:00 AM slept 147.5 minutes, while those who napped from 03:00 to 06:00 AM slept 112.0 minutes only. Shorter napping during this period could be related to medical procedures in the hospital before 7 AM that increase noise levels and interrupt the naps. Furthermore, anxiety about getting ready to leave (29) for another job may be another reason for shorter naps during the 03:00 to 06:00 AM naps.
In this study, we did not detect a statistically significant difference between the two nap groups in the change of test scores before and after the shift with respect to other psychomotor driving abilities. These tests include two hand coordination, peripheral perception, selective attention, visual pursuit, reactive stress tolerance, reaction time, and perceptual speed. This could be due to the limited sample size of our study or the lack of advantage between the two nap times. Studies with larger sample sizes are required to identify the equality of nap times with regards to the above-mentioned tests.
Previous researches directed to measure fitness to drive had focused on the RTC rates. However, this measure has several disadvantages. RTCs rarely occur, follow poison distribution, and are multi-causal (23). Other methods for measuring the risk of RTC including information gathered through self-reporting, insurance companies, and official sources are significantly different in agreement levels (30). Comparison of self-reported and recorded driving memories information revealed that 80% of minor RTCs and most of the near-accidents would be forgotten in two weeks (31). Several studies have designed standardized driving tests as an alternative measure of respondents’ fitness to drive (32, 33). VTS is among the best-known tests and its validity and reliability for measuring fitness to drive have been reported in several studies (25, 34). The VTS battery used in our study is a standard computer system that assesses essential psychomotor requirements for safe driving. It is legally used in 25 countries to assess drivers who commit violations (35).
To our knowledge, this is the first study that has utilized a reliable objective tool to compare the association of nap time with fitness to drive after night shift.
The limitation of our study was its small sample size. Moreover, we did not consider job difficulty and the personality traits of the participants. In addition, the quality of the nap and the environmental situation of the nurses’ rest room were not documented among the individuals.
5.1. Conclusions
Our study revealed that time-movement anticipation ability of night shift nurses who took a nap at 03:00 to 06:00 AM was deteriorated compared to a similar group of nurses who took a nap at 00:00 to 03:00 AM; considering the fact that time-movement anticipation is an important factor for safe driving, hazard control, and RTC prevention. We can conclude that night shift nurses who nap at 03:00 to 06:00 AM are at a higher risk of RTC while driving home after a night shift. However, further studies with larger sample sizes are needed to investigate the effect of nap types on the other psychomotor skills needed for safe driving.