1. Context
Medicines play a vital role in maintaining people’s health after inpatient and outpatient care (1, 2). Medicine demand is an unusual process. The consumers have limited discretion in the selection of medicines. Indeed, buying medicines is a multi-level process. First, the physician prescribes the medicine; then, the pharmacist prepares it and finally, the patient or insurer pays for it (3, 4).
The induced demand for medicines is multifactorial. Asymmetric information, the patient expectation for specific drug prescription, patient poor health literacy, and uncertainty about efficacy are among the characteristics of the medicine buying process, which can lead to induced demand (4, 5).
Customer experience in the pharmaceutical sector depends on the ability of the product to perform as expected by the patient (3). Desirable experience of consuming medicine and customer satisfaction can increase brand loyalty among consumers (6). A consumer who experienced the utility of consumption is not able to comprehend that whether the quality was due to previous requirements or not; therefore, healthcare professionals, as sellers, determine the need(s) of the consumer. If the healthcare professional has the ability to provide medical services to consumers, the problem of ‘fraud’ arises that influences healthcare expenditures (6).
Pharmaceutical expenditure is the third largest expenditure component of health care spending (7). Total pharmaceutical expenditure accounts for about 30% of the total health expenditure, on average, in low-income countries, which is a major cause of household impoverishment (1). Most countries have experienced irrational increases in medicine expenditure, which has turned into a severe economic crisis (1, 8). Since medicine expenditure consists of a significant proportion of health system costs, controlling medicine overuse is a priority. The price elasticity of pharmaceutical products is low, so consumer payments can have a negative impact on both health and equity (9). The increased percentage of unnecessary prescribed medicines not only exposes the financial burden on individuals and the entire society, but also may have side effects with negative influences on the health system performance (10, 11). Therefore, to control unnecessary prescriptions, we should identify factors influencing the induced demand for medicines. Due to the extensive and complex nature of the induced demand, the current study aimed to investigate factors affecting the induced demand for medicines and provide strategies to address the issue. Our results can be used to develop policies and control strategies at a macro level.
2. Evidence Acquisition
Scoping review is a knowledge synthesis technique aiming at collecting and evaluating the current state of knowledge of a particular issue. It is used when data collection and analysis techniques of reviewed studies are different. In this article, we followed the five stages of Arksey and O’Malley’s framework (12), as discussed in the following.
- Stage 1: Identifying research questions. The questions in this review were what are the factors affecting the induced demand for medicines and which strategies are appropriate to prevent it?
- Stage 2: Identifying relevant studies. We performed comprehensive literature searching in three major databases, i.e., PubMed, Cochrane Library, and Embase, covering the period of 1990 to 2016. Google Scholar was also used to find relevant documents and reports. To increase the accuracy of our search, we also checked the reference lists of all selected papers. The research query included terms about induced-demand for medicine, irrational use of medicine, and preventive strategies.
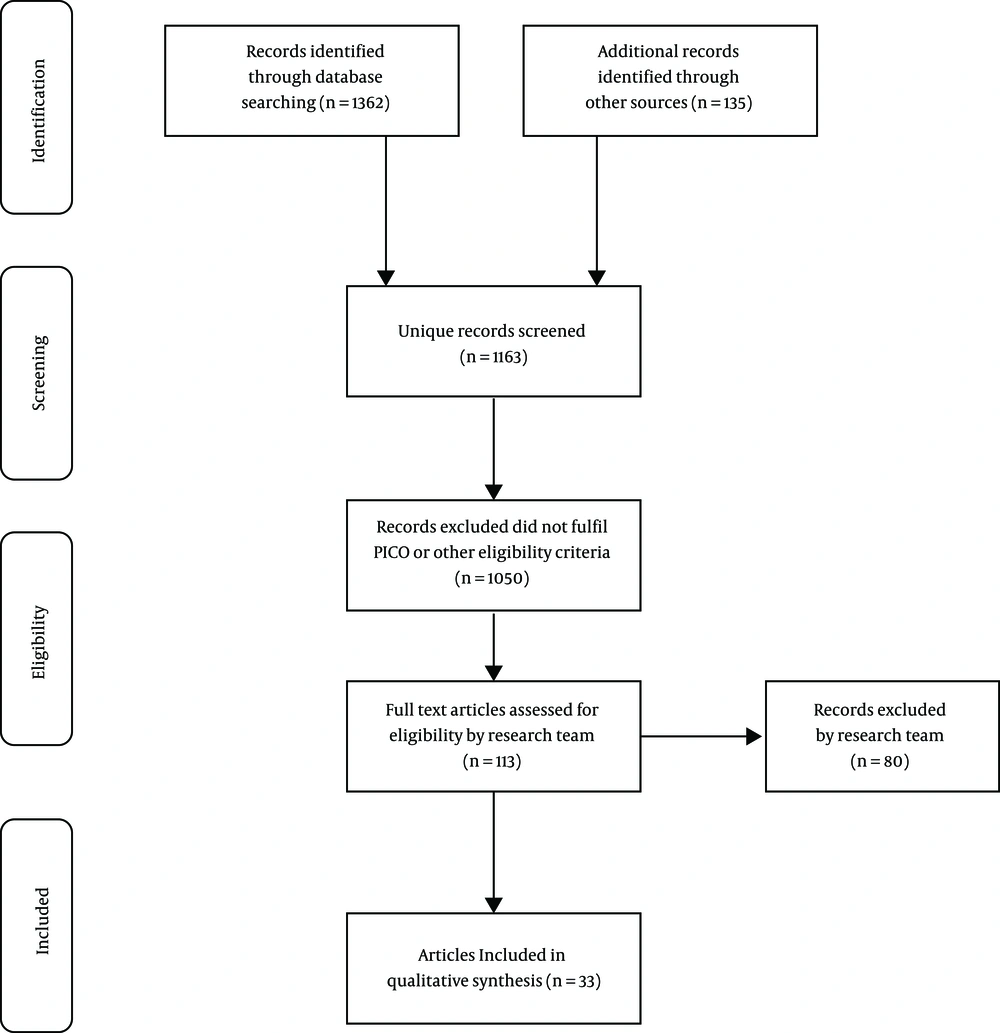
In the initial search, 1,497 records were identified and checked for the inclusion criteria. After deleting duplicates, 1,163 English studies remained. Three authors (MM, MAS, and LZ) followed the above-defined search strategy independently, screened the studies by title and abstract, and reached an agreement for about 90% of the articles. In this stage, there were 113 eligible studies. Following the inclusion criteria, 77 articles were excluded and 33 remaining papers were included (Figure 1).
- Stage 3: Study selection. In this review, we selected papers of any type of publication (systematic review, review, quantitative, and qualitative) between January 1, 1990 and March 10, 2017 in English among those presenting data about the induced-demand for medicines, irrational medicine use, medicines, prescription, payment, insurance, overuse. Finally, we excluded articles not focusing on topics that may be related to the induced-demand for medicines.
- Stage 4: Charting the data. For managing the data, the authors created a worksheet in Excel and record the data of each study including article title, name of authors, year of publication, study design, country (Table 1), and the main data about findings (factors and strategies) (Table 2).
| Authors (Ref.) | Study Design | Year | Country | Title |
|---|---|---|---|---|
| Riahi et al. (13) | Qualitative | 2016 | Iran | Induced demand: A challenge on the way of Iran health revolution program |
| Khorasani et al. (14) | Qualitative | 2015 | Iran | Identification of the healthcare services with potential induced demand |
| Busfield (15) | Quantitative and qualitative | 2015 | England | Assessing the overuse of medicines |
| Tsiantou et al. (16) | Cross-sectional | 2015 | European regions | General practitioners’ intention to prescribe and prescribing patterns in selected European settings: The OTCSOCIOMED project |
| Rezal et al. (17) | Systematic review | 2015 | UK | Physicians’ knowledge, perceptions and behavior towards antibiotic prescribing: A systematic review of the literature |
| Belrhiti (18) | Qualitative | 2015 | Morocco | Why health care managers are reluctant to rational use of medicines? Case study in a regional hospital Morocco |
| Jain et al. (19) | Qualitative review | 2015 | India | A systematic review of prescription pattern monitoring studies and their effectiveness in promoting rational use of medicines |
| Nouraei Motlagh et al. (20) | Quantitative | 2014 | Iran | Factors Influencing pharmaceutical demand in Iran: Results from a regression study |
| Chen et al. (21) | Quantitative | 2014 | China | Does economic incentive matter for rational use of medicine? China’s experience from the essential medicines program |
| Adebayo et al. (22) | Retrospective cross-sectional | 2013 | Nigeria | Influence of health insurance on rational use of drugs |
| Lu (23) | Audit study approach (quantitative) | 2013 | China | Insurance coverage and agency problems in doctor prescriptions: Evidence from a field experiment in China |
| Currie et al. (24) | Audit study | 2012 | China | Using audit studies to test for physician-induced demand: The case of antibiotic abuse in China |
| Pedlow (25) | Review | 2012 | USA | Assessing the impact of cost sharing on the induced demand for prescription drugs to support part d Medicare pricing |
| Lee et al. (26) | Systematic reviews | 2012 | USA | A systematic review of reference pricing: Implications for US prescription drug spending |
| Ron et al. (27) | Quantitative | 2010 | Lao People’s Democratic Republic | Medicine prescribing and the provider payment method in community-based health insurance in Lao People’s Democratic Republic |
| Mohanty et al. (28) | Quantitative | 2010 | India | Prescription pattern in the department of medicine of a tertiary care hospital in South India |
| Lo et al. (29) | Quantitative | 2010 | Hong Kong | Does vocational training in family medicine have an impact on antibiotic prescribing pattern? |
| Mohammadzadeh (30) | Qualitative | 2010 | Iran | The study of profitability of drugstores in Iran’s pharmaceutical system |
| Sarikaya, et al. (31) | Cross-sectional and qualitative | 2009 | Turkey | Exposure of medical students to pharmaceutical marketing in primary care settings: Frequent and influential |
| Huh et al. (32) | Quantitative | 2008 | USA | Prescription drug coverage and effects on drug expenditures among elderly Medicare beneficiaries |
| Morgan (33) | Quantitative and qualitative | 2007 | Vancouver | Direct-to-consumer advertising and expenditures on prescription drugs: A comparison of experiences in the United States and Canada |
| Iizuka (34) | Quantitative | 2007 | Japan | Experts’ agency problems: Evidence from the prescription drug market in Japan |
| Rohra et al. (35) | Quantitative | 2006 | Pakistan | Critical evaluation of the claims made by pharmaceutical companies in drug promotional material in Pakistan |
| Maio et al. (36) | Review | 2005 | USA | Pharmacy utilization and the Medicare modernization act |
| Pauly et al. (37) | Review | 2004 | USA | Medicare drug coverage and moral hazard |
| Lam et al. (38) | Quantitative | 2003 | Hong Kong | What are the non-biomedical reasons which make family doctors over-prescribe antibiotics for upper respiratory tract infection in a mixed private/public Asian setting? |
| Ess et al. (10) | Review | 2003 | Swiss | European healthcare policies for controlling drug expenditure |
| Chou et al. (39) | Quantitative | 2003 | Taiwan | Impact of separating drug prescribing and dispensing on provider behavior: Taiwan’s experience |
| Schneeweiss et al. (40) | Quantitative | 2002 | USA | Impact of reference-based pricing for angiotensin-converting enzyme inhibitors on drug utilization |
| Patricia and Mark (41) | Quantitative | 2002 | Pennsylvania | Health insurance and the grown in pharmaceutical expenditures |
| Wazana (42) | Qualitative review | 2000 | Canada | Physicians and the Pharmaceutical Industry: Is a Gift Ever Just a Gift? |
| Braae et al. (43) | Review | 1999 | New Zealand | Managing Pharmaceutical Expenditure while Increasing Access |
| Palmer and Bouchner (44) | Quantitative | 1997 | Massachusetts | Parents’ and Physicians’ Views on Antibiotics |
| Authors (Ref.) | Factors | Strategies |
|---|---|---|
| Riahi et al. (13) | The health revolution program has increased the induced demand through social factors (incremental demand, physician-centered system), fundamental factors (lost influence of referral and family physician programs), the organizational structure (weakness in the educational system, ignoring medicine ethics, lack of regulatory programs), and interested parties (suppliers and receivers). | This can be managed using such strategies as improving managers’ insight for supporting the induced-demand control, appropriate planning in healthcare system, correcting the educational system in the field of healthcare, and correcting the payment and referral systems. |
| Khorasani et al. (14) | Pecuniary motivations, little knowledge of physicians | - |
| Busfield (15) | The inaccuracy of doctors 'diagnosis and doctors' reluctance to risk, Failure to treat people who may benefit from antibiotics, as well as problems associated with unwillingness to prescribe medication | - |
| Tsiantou et al. (16) | The lack of an integrated primary care system and policies to promote the rational use of medicines | Demand-side factors that modify the behavior of prescribing drugs such as training, audit, decision support systems, guidelines, and financial incentives |
| Rezal et al. (17) | Patients' expectations, severity, and duration of infections, uncertainty overdiagnosis, possibility of losing patients and influence of pharmaceutical companies, Pocket-sized guidelines seen as an important source of information for physicians | Assessing the level of knowledge of doctors about antibiotics, methods of achieving, maintaining and improving this knowledge, including strategies for the rational use of antibiotics, patient education, and physician performance review based on existing guidelines |
| Belrhiti (18) | Lack of management information system, little commitment of experts and lack of effective organizational communication | Technical support from the executive levels in the Ministry of Health and institutionalize committee consisting of physicians, dentists and pharmacists are obliged to implement the rational use of medicines in hospitals |
| Jain et al. (19) | Failure of physicians to follow the guidelines | Control of drug prescription pattern |
| Nouraei Motlagh, et al. (20) | Changes in income will change the demand and consumption of drugs by households, age group and type of illness, government commitment to insurers | Developing policies such as increasing insurance resources, rationalizing resource allocation, setting up service packages based on the price elasticity of demand, and implementing coinsurance based on the type of drug used |
| Chen et al. (21) | Absence of physicians’ active involvement in shaping policies such as introduction of the essential medicines, formulation and implementation of essential medicines Policy from the top, pressure exerted by patients, no education of patients about the right way to take medicines by health workers, and neglect of their responsibilities because of overwork or because they are too eager to please their patients | Participation of many stakeholders, a national training system with financial support from central and local governments for the training of medical personnel, especially for less qualified pharmacy personnel and general practitioners in rural areas, patient involvement |
| Adebayo et al. (22) | Affordability of patients, lack of knowledge and training of prescribers and householders, low utilization of physicians and pharmacists from similar formularies, willing to prescribe brand drugs and the benefit from prescribing expensive drugs | Increasing public awareness through mass media, increasing training courses for prescribers, adopting policies for using formularies and provide a list of essential drugs |
| Lu (23) | Doctors' expectation to obtain a proportion of insured patients' drug expenditures | Doctors' expectation to obtain a proportion of insured patients' drug expenditures |
| Currie et al. (24) | Financial incentives, patient perspective, patient satisfaction, little knowledge of physicians, donations to doctors by pharmaceutical companies | Modifying payment systems |
| Pedlow (25) | Insurance coverage of medicines | Sharing the costs through copayment or coinsurance, coverage of physicians visits by insurances, control over managed care, limiting the services package and paying attention to the essential or non-essential medicines |
| Lee et al. (26) | Insurance coverage of medicines, patient’s age | - |
| Ron et al. (27) | Prescribing as a revenue-generating mechanism for the provider, satisfying the patient and “old habits”, without spending adequate time on examination and consultation, lack of monitoring of prescribing | Using appropriate payment methods, such as per capita, because this method prevents the prescription of expensive drugs for patients, encouraging the rational use of medicines, informing patients, setting payment ceilings in government sectors, and controlling profits, developing a drug committee in the hospitals |
| Mohanty et al. (28) | Advertisements and visits by pharmaceutical companies, doubt about efficacy and bioavailability of generic formulations, prescribers’ ignorance of the price variations between generic and brand drugs, Lack of information of the availability of generic formulations from pharmaceutical companies | Using drug and therapeutic committees to formulate and standardize drug policy, conducting regular audits and checking on the undue influence of high power salesmanship, correct and timely diagnosis, educational interventions, encouraging prescription based on the list of essential medicines |
| Lo et al. (29) | Not running family physician courses | Training family physicians |
| Mohammadzadeh (30) | Increasing drugstores | Some new policies like giving some special commercial credits and privileges or covering some legal expenses by the government that decisionmakers must consider them thoroughly. |
| Sarikaya et al. (31) | Interaction between pharmaceutical companies and medical personnel | Improving the skill of the rational use of medicines, implementing strategies to overcome drug marketers |
| Huh et al. (32) | Medicaid programs that provide drug coverage | - |
| Morgan (33) | Direct advertising for consumers | - |
| Iizuka (34) | Obtained markup by physicians, non-separation between prescribing and dispensing drugs, physicians’ pocket, the difference between the wholesale price set by companies and the retail price | - |
| Rohra et al. (35) | Exaggerated claims/ Ambiguous claims/ False Claims/ Controversial claims of pharmaceutical advertising claims | - |
| Maio et al. (36) | - | Capping the number or total value of prescriptions reimbursed, cost-sharing mechanisms like copayments, coinsurance, and deductibles, prior authorization; the most common tool used to manage prescription drug costs and utilization is the formulary, therapeutic substitution, generic substitution |
| Pauly (37) | Drug coverage increase | - |
| Lam et al. (38) | Age and seniority of doctors, practicing in private sector, to satisfy the patient or his/her career, fear of medicolegal problem if patient deteriorates, persistence of patients to obtain drugs, save time and financial implication | - |
| Ess et al. (10) | - | Three types of pricing policies can be recognized: product price control, reference pricing, and profit control. To control costs, the use of generic drugs should be encouraged, defining a list either of drugs reimbursed (positive list) or one of the drugs not reimbursed (negative list), patient co-payments, policies intended to affect physicians’ prescribing behavior including guidelines, information (about price and less expensive alternatives) and feedback, and the use of budgetary restrictions |
| Chou et al. (39) | Physicians both prescribe and dispense drugs | - |
| Schneeweiss et al. (40) | - | Policies like reference pricing, increasing patients’ participation in costs (cost-sharing) |
| Patricia and Mark (41) | Growth in insurance coverage and reduction of the true cost of drugs, new drug therapies | - |
| Wazana (42) | The relationship between doctors and pharmaceutical companies | Educational system reform, policy for controlling the relationship between doctor and pharmaceutical companies |
| Braae et al. (43) | Subsidies make patients and doctors reluctant to the price signals or budget constraints that might otherwise regulate demand, demand driven by demographic factors, the medicalization of common conditions and advertising to consumers | Managing the pharmaceutical schedule and the list of drugs subsidized, controlled access to subsidy, price competition between pharmaceutical companies, managing expenditures on subsidies through reference pricing, expenditure caps, targeting and restrictions on access to subsidy, tendering for the sole supply or the preferred brand |
| Palmer and Bauchner (44) | The patient’s request and his view on some medications | Informing and educating parents is a way to reduce the demand for drugs, especially for antibiotics |
- Stage 5: Collating, summarizing, and reporting the results. We used a narrative method to extract common themes about factors and strategies and conduct a qualitative analysis.
3. Results
3.1. Description of Studies
In this study, thematic analysis was used. Table 2 shows the eight factors that can affect the induced demand and six strategies to address them based on previous studies.
3.2. Factors Influencing the Induced Demand for Medicine
3.2.1. Monitoring Mechanisms
Inadequate monitoring mechanism is an essential factor affecting the induced demand (27). Some physicians do not use clinical guidelines. Some people believe that these guidelines should be localized and some are not familiar with them or do not regard them as useful (17). The practical gap between the rational use of medicine policy and the real measures of physicians in hospitals stem from the inappropriate information management systems (18).
3.2.2. Demand-Side Factors
Studies show that increasing household income, patient’s perspective, and patients’ gender are the demand-side biological factors influence the demand for medicines (20, 44). Non-biological factors, such as patient’s demand for prescribing antibiotics, are influencing on physicians’ prescription behavior in more than 50% of consultations (38).
3.2.3. Supply-Side Factors
Financial incentives and physician preferences for prescribing expensive brand medicines are the primary factors of induced demand. Job experience and superiority of physicians, expectations to acquire income from prescriptions, prescription habits, and ignoring clinical practice guidelines also can affect thee induced demand. Some studies pointed to the limited knowledge of physicians and their inaccuracy in disease diagnosis, their unwillingness to accept the risk of disease and fear of losing clients, as well as high job load or enthusiasm to keep patients and satisfying them (17, 21, 24, 27, 38).
3.2.4. Structural Factors
In countries with an integrated healthcare system, rational prescribing behaviors still are not fully developed (16). The integration of the prescription and distribution process is one of the reasons for the induced demand (39).
3.2.5. Legal and Political Factors
The lack of physicians’ active participation in developing policies such as an essential drug list and top-down approaches to develop and implement such policies are among other influencing factors (16, 21).
3.2.6. Insurance Coverage and Subsidies
Expanding medicine insurance coverage and subsidies reduce the price of medicines and therefore, reduce the physician’s sensitivity to prices and budget limitations and incentive them to prescribe more (43).
3.2.7. Commercial Interactions and Advertisement
Advertisement and visits of pharmaceutical companies (17, 28), interactions between pharmaceutical companies and medical personnel, pressures of pharmaceutical companies (17) and giving gifts to physicians are factors that can influence the induced demand (33, 42, 43).
3.2.8. Educational Factors
Unawareness of physicians and prescribers, as well as households, and preferences to prescribe brand products can influence the induced demand (21, 22).
3.3. Strategies to Address the Induced Demand for Medicines
3.3.1. Monitoring Mechanisms
Studies mentioned that the induced demand can be reduced by audits and guidelines (16), performance evaluation of physicians (17, 19), regular supervision to reduce the impact of pharmaceutical companies on physician prescription (28), and developing guidelines and providing information about prices and substitute medicines with lower prices (10).
3.3.2. Legal and Political Factors
Lack of physicians’ participation in the development of an essential medicine list and its top-down implementation are among the leading barriers to address the induced demand (21). Also, appropriate policy-making about the interaction between pharmaceutical companies and physicians and adopting policies to use formularies can reduce the induced demand (22, 42).
3.3.3. Education and Awareness Promotion
Increasing public awareness through public media, revising the education system (13, 22, 28), and establishing a national education system to train less qualified personnel at remote areas (21, 31) can reduce the induced demand. Promoting managers’ perspectives about supporting the control of induced demand and appropriate planning in the health system at a macro level are also effective for reducing the induced demand (13).
3.3.4. Structural and Operational Factors
Correcting medicine prescription behaviors, such as strategies to cope with pharmaceutical marketers, and establishing medicine and treatment committees at hospitals to formalize and standardize pharmaceutical strategies are methods to reduce the induced demand (16, 18, 22, 27, 28). A study of challenges of Iran’s health transformation plan recognized the appropriate planning of the health system, revision of payment method, and establishment of the referral system as fundamental strategies to reduce the induced demand (13).
3.3.5. Insurance and Financial Policies
Insurance and financial policies were among the most important strategies in most of the reviewed studies. Medicine consumption mechanisms may include establishing a maximum level for medicines (quantity and costs), cost-sharing methods such as deductible, requiring insurance confirmation to prevent high-cost medicines, developing a benefits package based on price elasticity, and replacement of generic medicine (10, 36). Also, developing policies such as increasing the financial resources of insurances, rationalization of resource allocation, increasing cost-sharing, and appropriate payment methods are suggested. Besides, controlling medicine’s profit through reference price setting, competitive prices between pharmacists, and price control can limit irrational prescription (20, 27, 43).
3.3.6. Supportive Policies
Adopting supportive policies are effective in reducing the induced demand, such as compensating the share of costs by the government for pharmacies that have rational behavior in prescription and permissions to sell cosmetics, providing some advertisement and marketing facilities, encouraging them for rational prescription based on essential medicine lists and providing financial stimulators to them (16, 27, 30).
4. Conclusions
Physicians, as the patients’ agents, can directly control the use of many medical inputs, particularly medicines, so that their decisions have a profound impact on quantity, quality, and costs of healthcare systems. In this study, we aimed to investigate the key factors that affect the induced demand for medicines and strategies to address it. The extracted themes were categorized into eight groups: Monitoring mechanisms, demand-side factors, supply-side factors, structural factors, legal and political factors, insurance coverage and subsidies, commercial interactions and advertisement, educational factors.
Concerning monitoring mechanisms, denying clinical practice guidelines (CPGs) on antibiotic consumption by physicians and lack of a monitoring system for prescription or lack of information systems are the promoters of the induced demand. The studies by Ron et al. (27), Jain et al. (19), and Belrhiti (18) proposed the following solutions to limit the induced demand: controlling prescription, stronger monitoring of physicians and their assistants, technical supports by operational levels of the Ministry of Health and institutionalization of medicine committees comprising physicians, dentists, and pharmacists to require health personnel for rational prescriptions in hospitals (45). Rezal et al. also mentioned these problems and argued that physician performance monitoring can be an appropriate strategy (17).
Discussing supply-side and demand-side factors is an important issue in the arena of induced demand for medicines. In health systems, especially in developing countries, often there is a perspective among patients that the more a physician prescribes medicines, the better is his performance. If the physician performance is not consistent with their expectations, even when the prescription is not necessary, the patient insists on more medicines. However, sometimes physicians prescribe unnecessary medicines to satisfy their patients and assure future consultations. Adebayo et al. believed that this perspective roots in the unawareness of patients (22). Rezal et al., Palmer, Currie et al., and Lam in their studies noted that insistence on prescribing a medicine, particularly by parents, is one of the reasons for rising antibiotics consumption (17, 24, 38, 44). Chen et al. also argued that physicians prescribe unnecessary medicines to satisfy the patients (21). In addition, like regular goods, if income increases, the demand for medicines also increases. Nouraei Motlagh et al. recognized this issue as a factor that increases patient’s demand (20). Nouraei Motlagh et al. (20), Maio et al. (36), Schneeweiss et al. (40), and Pedlow (25) noted some strategies to address demand-side factors, including medicine consumption mechanisms such as setting caps for both quantity and costs, cost-sharing (e.g. co-payment, coinsurance, deductible), and requiring pre-approval, particularly for expensive, unnecessary, and high-risk medicines, and also developing benefit packages based on price elasticity of demand. Another way to control the induced demand is patients’ training and increasing their awareness of side effects of excessive medicine consumption. If patients acquire sufficient information, information asymmetry would be minimized and therefore, the induced demand decreases. Chen et al. (21), Ron et al. (27), Palmer and Bauchner (44), and Tsiantou et al. (16) emphasized these issues.
Physician financial incentives to achieve the target income is another important factor. By prescribing brand medicine and acquiring a share of profit of prescribing expensive medicine, physicians earn a significant income. Adebayo et al. noted the limited use of formularies, preferences to prescribe brand medicine, and gaining benefit from prescribing expensive medicines as factors that increase medicine consumption (22). Mohanty et al. also mentioned the physicians’ ignorance of the price difference between brands and generic medicines and subsequent financial burden as an important factor (28). Khorasani et al. emphasized physician financial incentives as the stimulator of induced demand and proposed mechanisms such as reference pricing, emphasizing generic medicines, limiting compensation or stopping it by developing a list of medicines with insurance coverage (14, 23, 24, 27, 38, 46). In the health system, uncertainty is an inseparable concept and often physicians, especially less experienced physicians, prescribe unnecessary services and medicines to avoid risks and complaints. For highly experienced physicians, old habits are an important factor. For both groups, ignoring the guidelines and limited knowledge can result in increasing irrational prescription. Busfield (15), Lam et al. (38), and Chen et al. (21) noted the physicians’ unwillingness to accept the risk as a factor that results in the induced demand. Ignoring guidelines is a common factor that was emphasized in most of the investigated studies. Physicians and pharmacists’ active participation in developing guidelines as an incentive factor for rational prescription and monitoring their performance based on these guidelines are among the recommended solutions (10, 16, 17, 19, 36, 47). In addition, Adebayo et al. have noted that by using formularies and developing essential medicine lists, unnecessary prescription can be reduced (22). From a political perspective, in most countries, developing medicine policies has a top-down approach, which reduces physicians and pharmacists’ incentives to comply with these policies and rational prescription. Therefore, engaging stakeholders in regulation and developing policies besides the establishing an integrated primary healthcare system is among the best strategies to control the induced demand, as mentioned in previous studies (16, 21, 45).
Belrhiti noted the low commitment of specialists due to the lack of active participation in developing policies as a factor that influences irrational consumption of medicines and believed that the solution is to establish medicine committees in hospitals and engaging physicians in developing inter-organizational policies for rational consumption (18). Riahi et al. also mentioned the weaknesses of regulatory programs in the health transformation plan in Iran as a factor that creates the induced demand and believed that improving managers’ perspectives about supporting the control of induced demand along with appropriate planning can be useful (13). Besides the political and legal factors, structural factors also limit the control of medicine consumption. Iizuka (34) and Chou et al. (39) indicated that when prescription and distribution of medicines are not separated, monitoring and supervision are irrelevant. If medicine production and distribution are not rational and the market is not balanced, the separation of these two processes and structural revisions are the best strategies to solve the problem. Cost-sharing and availability of a third party to compensate for costs and allocating subsidies clearly change the financial incentives of patients and physicians because it reduces real prices. Insurance coverage reduces physicians’ concerns about patients’ ability to pay and incentives them to prescribe more. Pauly (37), Huh et al. (32), Schneeweiss et al. (40), Patricia and Mark (41), Ess et al. (10), Pedlow (25), and Lee et al. (26) pointed to the expansion of insurance coverage as a reason for the increased demand for medicines. These studies recognized developing a list of covered medicines, determining prescription cap per each patient, and increasing cost-sharing as strategies to cope with the problem (48). Ron et al. noted that subsidies have an important role in physician prescriptions and their negligence of budget limitations and discussed demand regulation in the market to manage the consumption of medicines with subsidies (27).
Many authors, such as Mohanty et al. (28), Sarikaya et al. (31), Rezal et al. (17), Wazana (42), and Currie et al. (24), noted that the commercial interaction with pharmaceutical companies is a reason for physicians’ incentive for irrational prescriptions (49). By tempting physicians (giving gifts, offering free travel tours, sharing profits, and other financial incentives), pharmaceutical companies assure their market share. In addition, disease mongering and advertisement to consumers are important factors that influence medicine consumption. “Disease mongering and drug marketing are a process that tries to ensure that essentially well people are sick or slightly sick people are very ill in order to expand the markets for treatment” (50). Many medicines, such as slimming drugs, are selling through this way. Morgan (33), Rohra et al. (35), and Braae et al. (43) mentioned this problem in their studies. To control these issues, strategies must be employed to control marketers, for example, by using medicine instruction books and alternative medicines such as the generic ones. Also, by developing the list of covered medicines, insurance compensation can be limited. Periodic monitoring can also be employed (28, 31).
The weakness of the education system is another important factor, which influences the induced demand. Physicians’ unawareness of irrational prescription and their preference for prescribing brand medicines besides the lack of training programs for patients can influence medicine consumption. Lo et al. noted the absence of family physician training (29), Rezal et al. indicated the inadequate knowledge and limited information of physicians about antibiotic resistance, and Chen et al. pointed to the lack of patients’ training by health personnel as the factors that influence consumption of medicines (17, 21). Increasing public awareness through public media, enhancing training programs for prescribers about using formularies, and developing essential medicine lists are strategies mentioned in Adebayo et al. study (22, 45).
As a strength, this scoping review was based on a comprehensive analysis of different studies in details in which, a summary of mentioned factors was extracted based on various documents and perspectives. Also, corrective strategies were proposed based on reviewed perspectives and belief of policymakers. The main limitation of the current study was the language barrier as only English language studies were considered. Therefore, some studies may have been missed.
Although research on rational use and the induced demand for medicines is an evolving field, there is still much ground to cover and work to do. This study concludes that a large number of components can affect the demand for drugs induced by physicians, each of which has a unique strategy to prevent. It means that the best corrective strategy depends on the time and situation in which the induced demand is occurring. Since in developing countries the most important factors are the lack of a comprehensive monitoring system and supply-side factors, it seems that monitoring mechanisms such as performance audit and guideline development can reduce the financial burden of the demand for medicines in healthcare systems.