1. Background
To having a healthy lifes, people have to use health services or in other words, purchase the services, to improve and restore their health if their health diminishes. Based on the type of health system, using this health service may impose different financial pressures on people in different societies, and if these expenses are paid out of pocket (OOP), it can cause financial difficulties for households, which may lead to poverty (1). On the other hand, the WHO has declared household financial protection as one of the goals of the health system in recent years (1-3). Evidence indicates that one of the barriers to health services access is the costs that patients have to pay (4-6). Meanwhile, OOP payment is the most common and the most important methods of financing in Asian countries and other developing countries (7). There are a large number of studies that show the distribution of OOP and their effect on impoverishment and household welfare (8, 9). Baji et al. in their study in Hungary showed that most people pay OOP for health services, and financing dropped so that the Kakwani indicator was negative in this country (10). Recent studies in India (11), Georgia (12), China (13), the United States (14), and Turkey (15) have shown that OOP payments lead to catastrophic household health expenditures and put them at risk. In Iran, the turnout in the provision of health spending during 2000 - 2009 was always above 50%; moreover, households’ contribution to the healthcare system were 58.36% and 61.01% in 2000 and 2009, respectively (16).
Cardiovascular diseases are known as the first cause of death in Iran (17), and it is the leading cause of healthcare costs (18). Surgical treatment such as coronary artery bypass grafting or CABG is a basic method for the treatment of coronary artery disease and is now one of the most common surgical procedures (19) which can be used effectively to reduce the number of deaths (20). CABG is a critical intervention for heart disease and during the recovery period poses some problems for the patient and his/her family (21).
The last recent reform of the health system in the Islamic Republic of Iran is the Health Sector Evolution Plan (HSPE). The Ministry of Health and Medical Education started HSRP regarding to the 20-year-old legal provisions vision for May 2014 with three approaches of people’s financial protection, access to health services and improvement of the quality of services (22). This project consists of seven basic instructions, one of which consisting of the programs to reduce the amount paid by patients admitted to hospitals affiliated with the Ministry of Health and Medical Education. Based on this instruction, hospitalized patients only pay 6% of the fees and other costs will be covered by insurance companies (23).
2. Objectives
Given that the core of Health Sector Evolution Plan (HSEP) is to reduce the amount of patient payment and, on the other hand, many of the patients with coronary artery disease have to do costly surgical procedures; therefore, this study aimed to investigate the health development plan based on the patient’s contribution to CABG in Shiraz’s Namazi Heart Hospital. The findings of this study could offer useful information to hospital managers and health policy-makers, as well as taking appropriate measures to promote the increased quality of service and household financial protection.
3. Methods
This cross-sectional study was conducted as descriptive-analytic in Namazi Teaching Hospital as the largest hospital in the south of Iran in 2017. The study population included all patients who were undergoing CABG surgery in Namazi Hospital in Shiraz during two years; before (2012 - 2013) and after the implementation of HSPE (2015 - 2016). Due to the limited number of patients undergoing CABG, the samples were selected according to census and a total of 316 patients participated in the study. Of these, 50% of the patients were under CABG surgery before the implementation of HSPE (2012 - 2013).
The data collection employed a standard checklist based on the research objectives. This checklist included; row, patient medical records number, age, sex, type of insurance, having supplementary insurance, length of stay, admission date, total costs, patient’s OOP payment (patient’s contributions to total cost), the share of insurance (insurance contributions to total cost), plan’s share, supplementary insurance contributions, patient’s discount, supportive assistance (assistance by charities and people’s organizations), and other donations. The validity of the checklist was confirmed by 7 faculty members in the health services management in Shiraz University of Medical Sciences.
In order to collect information on the costs, the researcher first referred to management and security department of the hospital to coordinate and then to the cost accounting unit. The checklists were completed with information on the hospital’s health information system or HIS from 15 May 2012 to 15 May 2016. HIS is a comprehensive, integrated information system designed to manage all the aspects of a hospital's operation, such as medical, administrative, financial, and legal issues and as well as corresponding processing of services. Hospital information system is also known as hospital management software or hospital management system.
After completing the checklist, the data was analyzed using SPSS (SPSS Inc., Chicago, IL, USA) software 23. In this regard, t-test and One-way ANOVA at a significance level of α = 5% were used. It should be noted that because of moral considerations in research, the participants’ information was confidential.
3.1. Ethical Considerations
The study was approved by the Ethics Committee of Shiraz University of Medical Sciences, Shiraz, Iran (code: 14404).
4. Results
The results of this study showed that 58% of the patients who underwent CABG were male and 41.1% of them were under rural insurance coverage. About 96.5% of the subjects did not have supplementary insurance. Half of the patients had undergone CABG surgery before HSPE (158 patients). The mean age of the patients’ before HSPE was 63.4 and after that was 64.0 and in total, it was 63.7 years old. The mean length of stay of the patients were 5.8 and 6.1 days before and after HSEP, respectively. Also, in total, it was 5.9 days.
Moreover, the average cost of CABG surgery before HSEP (years 2012 - 2013) was calculated as 1198.59$, and after HSEP (2014 - 2015) it was 3260.36$. Among these, the average patient’s share of the total costs, before the plan was estimated as 213.22$ and after that it was estimated as 243.28$. The average of insurance contribution of the total cost before and after HSEP was 943.71$ and 2652.46$, respectively. The average of the plan’s share of the total cost after HSEP was 302.05$. The information on the cost of the patients is shown in Table 1.
| Average ($ American) | Standard Deviation | Minimum | Maximum | |
|---|---|---|---|---|
| Total cost | ||||
| Before implementation of the plan | 1198.59 | 378.71 | 152.72 | 4420.32 |
| After implementation of the plan | 3260.36 | 2146.08 | 1257.27 | 26998.41 |
| Patient’s contributions | ||||
| Before implementation of the plan | 213.22 | 166.38 | 0 | 2991.0 |
| After implementation of the plan | 243.28 | 227.19 | 0 | 7623.08 |
| Insurance contributions | ||||
| Before implementation of the plan | 943.71 | 294.59 | 0 | 2991.0 |
| After implementation of the plan | 2652.46 | 841.68 | 1079.93 | 7623.08 |
| Plan’s share | ||||
| Before implementation of the plan | 0 | 0 | 0 | 0 |
| After implementation of the plan | 302.05 | 210.97 | 0 | 1214.92 |
| Discount ka | ||||
| Before implementation of the plan | 26.31 | 29.95 | 0 | 293.80 |
| After implementation of the plan | 4.61 | 15.23 | 0 | 132.34 |
| Supplementary insurance | ||||
| Before implementation of the plan | 6.48 | 39.48 | 0 | 415.56 |
| After implementation of the plan | 9.52 | 60.86 | 0 | 439.38 |
| Patient’s discount | ||||
| Before implementation of the plan | 0 | 0 | 0 | 0 |
| After implementation of the plan | 44.78 | 52.91 | 0 | 497.61 |
| Supportive assistance | ||||
| Before implementation of the plan | 6.88 | 29.71 | 0 | 269.98 |
| After implementation of the plan | 3.13 | 23.16 | 0 | 2170.46 |
| Other discounts | ||||
| Before implementation of the plan | 1.99 | 7.55 | 0 | 53.73 |
| After implementation of the plan | 0.527 | 3.94 | 0 | 39.70 |
aDiscount k: K surgery referred to as a fee or tariffs for a medical service. The discount k is also part of k surgery for some services that is not paid by patients and is considered as a discount.
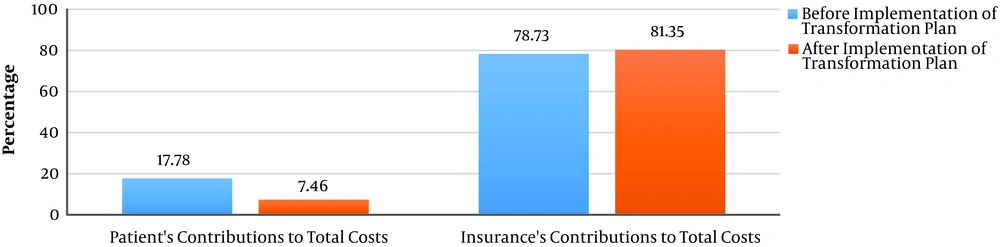
According to the results, the percentage of patients’ OOP payment to total cost for CABG surgery decreased from 17.78% to 7.46% after HSEP and it was statistically significant (P < 0.001). Moreover, the percentage of insurance contribution to the total cost for this surgery before and after the plan was 78.73% and 81.35%, respectively. (Table 2 and Figure 1).
| Average (Percentage) | Standard Deviation | F | Sig. | |
|---|---|---|---|---|
| Patient’s contribution of total cost | 12.58 | 0.000 | ||
| Before implementation of the plan | 0.1778 (17.78) | 14.39 | ||
| After implementation of the plan | 0.0746 (7.46) | 6.13 | ||
| Insurance contributions of total cost | 1.90 | 0.168 | ||
| Before implementation of the plan | 0.7873 (78.73) | 12.5 | ||
| After implementation of the plan | 0.8135 (81.35) | 8.63 |
The findings also showed that the increase in the average of total cost, patient share, insurance contribution, and plan’s share before and after the program were significant (P < 0.05) (Table 3).
| The Average Cost Before and After the Plan | F | P Value | |
|---|---|---|---|
| Total cost | Increase | 17.54 | 0.000 |
| Patient’s contribution | Increase | 7.82 | 0.001 |
| Insurance’s contribution | Increase | 48.83 | 0.000 |
| Plan’s contribution | Increase | 149.88 | 0.000 |
The results showed that patients’ OOP payment with rural insurance, health service and social security insurance has significantly decreased after the HSEP (P < 0.05). However, for Imam Khomeini Relief Foundation insurance, although this difference increased, it was not significant (P > 0.05) (Table 4).
| Type of Insurance | Before and After Implementation of Reform Plan | P Value |
|---|---|---|
| Rural | 13% decrease | 0.000 |
| Health service | 10% decrease | 0.008 |
| Social security | 5% decrease | 0.000 |
| Imam Khomeini Relief Foundation | 1% increase | 0.490 |
5. Discussion
This study compared the patients’ OOP payment for CABG surgery before and after the implementation of HSPE. The findings of this study showed that the total cost for CABG increased after the implementation of HSEP, while the share of patients and insurance also increased significantly. However, this increase in the total cost was due to an increase in the general level of prices. Therefore, considering this issue, the average of patients’ share of the total cost after the implementation of HSPE has significantly decreased, and on the other hand, the average of insurance contributions to the total cost has also increased, which is not significant.
Reduction the ratio of patients’ share to the total cost may be due to the addition of the plan’s share after the implementation of the HSPE, which significantly reduced the cost of the patient. It also may be due to the allocation of resources from the targeted subsidies and one percent of the value added tax in the form of health subsidies. The increase in insurance payments is as well as an important step in the implementation of HSEP.
The results of some similar studies indicate a reduction in the ratio of patients’ share to the total costs. Zare and Hoshmandi (24) in their study showed that HSEP has caused an increase in the cost of health insurance; also, the patients’ OOP payment share of the total costs revealed a significant decrease. The results of Yazdanpanah and Noruzi’s (25) study showed that the patients’ OOP payment in Namazi Hospital significantly reduced after HSPE. According to the findings of Kheiri et al. (26) whose study has been carried out in some hospitals in Iran, HSEP has been effective in reducing patient OOP payments. Heidarian and Vahdat (27) in their study reported that by taking inflation into account, the average amount of OOP payments has decreased and also the cost of any medical records in 2014 compared to 2013 increased 2 times, so that the patient’s OOP payment in 2014 decreased 1.8 times over the previous year.
However, the research of Etemadian and Izadi (28) in the study of the cost of coronary artery bypass surgery before and after the implementation of HSEP in private hospitals in Shiraz showed that the share of patients from the total cost for private sector services has increased. The reason for the difference between the results of this study and the present study is the type of hospitals surveyed.
The results showed that for all three types of rural insurance, Health Service and Social Security insurance, the ratio of patients’ OOP payments significantly decreased. However, this payment has increased for Imam Khomeini Relief Foundation, which has not been significant and can be explained by the low number of patients for this type of insurance.
Insurance organizations as purchasers of health services can cause an increase in out of pocket payments of the insured people as well as informal payments by delaying their reimbursements and limiting the health service packages. According to this explanation and due to the fact that the shares of the patients were about 70% of total cost (cost of hospitalization) before implementing the health sector evolution plan, the findings of this study showed that the share of out of pocket of the insured people has declined. This reduction may be due to an effective step of HSEP to decrease the share of people from their health costs. Nevertheless, it seems it’s a long way to go yet to reform the insurance payment system.
In confirmation of the findings of this study, the Panahi et al. (29) study showed that the government can take appropriate actions with the major development of insurance to reduce OOP payments. Similarly, Aryeetey et al. (30) and Xu et al. (31) in their studies reported that lack of health insurance coverage is considered as the reason for catastrophic expenditures in the health system.
Our study suffers from some limitations. One of the limitations of the current study is the lack of previous studies in Iran regarding OOP payments after implementation of the HSEP to compare with the results of the current study. In order to perform upcoming researches, it is suggested that the causes of the total cost increase for CABG surgery should be investigated after implementation of the HSEP. It is also recommended that the cost of other cardiac surgeries should be evaluated before and after the implementation of the HSEP. Finally, considering the results and benefits of the HSEP in reducing OOP payments, it is recommended that the plan be continued and its weaknesses reviewed and resolved.
5.1. Conclusions
In general, after the implementation of the HSEP, the ratio of patient’s OOP payment for CABG has decreased. Thus, one of the most important goals of the plan has been achieved. However, the average of patients’ OOP payment has increased.