1. Introduction
Cleft lip-palate (CLP) is a common facial deformity that affects esthetic, speech, and also hearing (1). Various treatment modalities have been attempted in CLP patients to resolve these problems. Primary surgical correction of lip and nose usually leaves CLP infants with an unpleasant wide scar, because of excessive amount of stretching of the skin. Also, nasal esthetics reduced due to decreased columella length, and increased columella width. Moreover, the primary surgical correction is followed by a secondary alveolar bone grafting to correct widened alveolar cleft gap (2). To address these issues, the idea of infant orthopedics was developed when buccal plates were used in order to approximate the separated cleft edges in 1950 by McNeil (3). Over the years, many changes have taken place in appliance designs. All of those orthopedic appliances only move alveolar segments together and do not modify the nasal architecture.
Matsuo et al., described that high plasticity can be explained by increased levels of hyaluronic acid as a result of high maternal estrogen level at early postnatal stages (4). Based on this concept, Grayson et al., developed an intraoral molding plate with nasal stents, which actively mold the nasal cartilage and alveolar segments (nasoalveolar moulding, NAM) (5). It was also suggested that NAM, produced an interstitial expansion by stimulating immature nasal chondroblasts, and therefore, improved the nasal morphology (6, 7). Conventional NAM requires taking impression from the neonate, which is very challenging. Therefore, procedures that circumvent this limitation are needed.
Monasterio et al., first reported the use of a paperclip lined with plastic as the nasal elevator, combined with an elastic band attached to the forehead to match the cleft segments. To avoid the intraoral plate, the paper tape was substituted for the combination of paper tape and elastic band (DynaCleft®, Canica Design Inc, Almonate, Ontario, Canada) (8). The nasal elevation technique is less invasive and has a lower risk of nostril airway obstruction. Lack of intraoral appliance in this technique also reduces the risk of injuries to oral mucosa. Further, since the adjustments can be done by nurses, it does not require a dental specialist and therefore, chair time treatment costs are reduced. Moreover, it is easier for parents to understand and manage.
2. Case Presentation
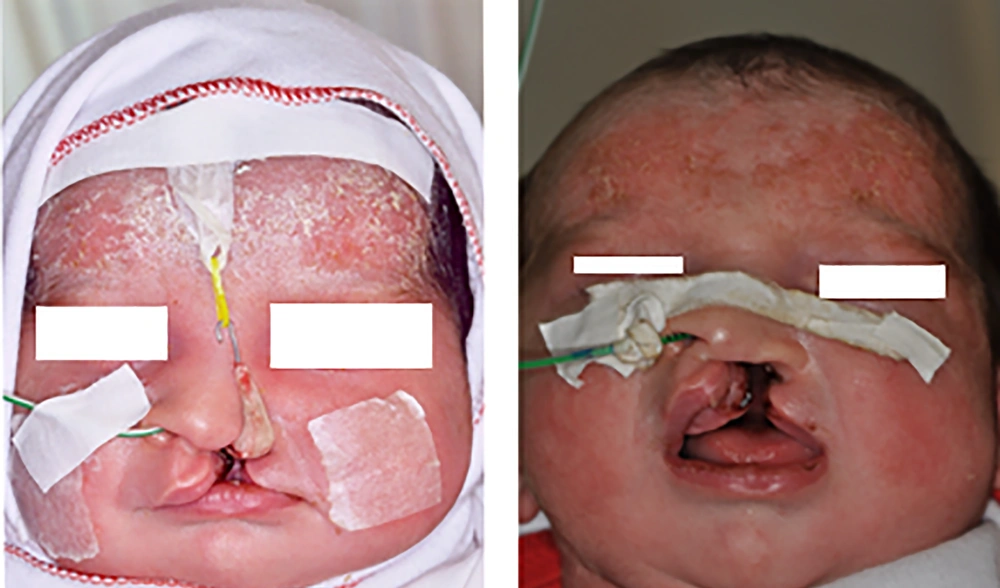
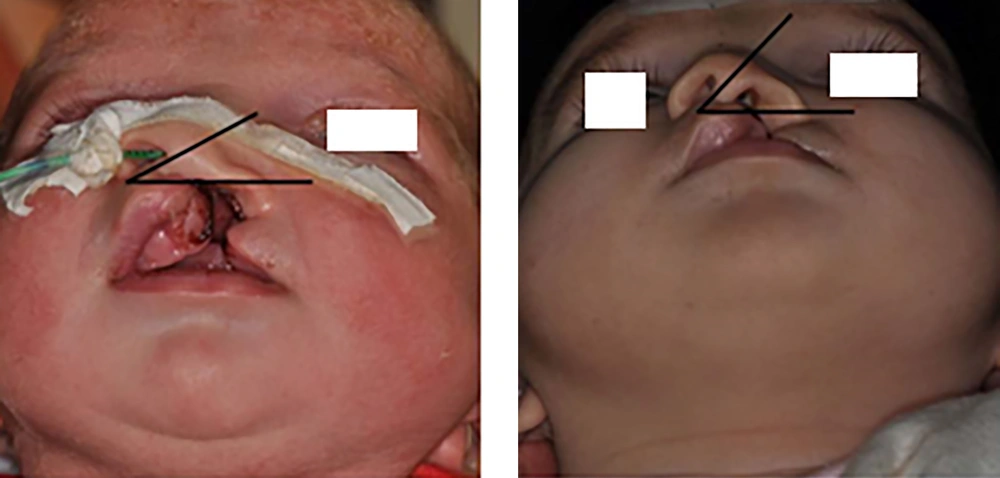
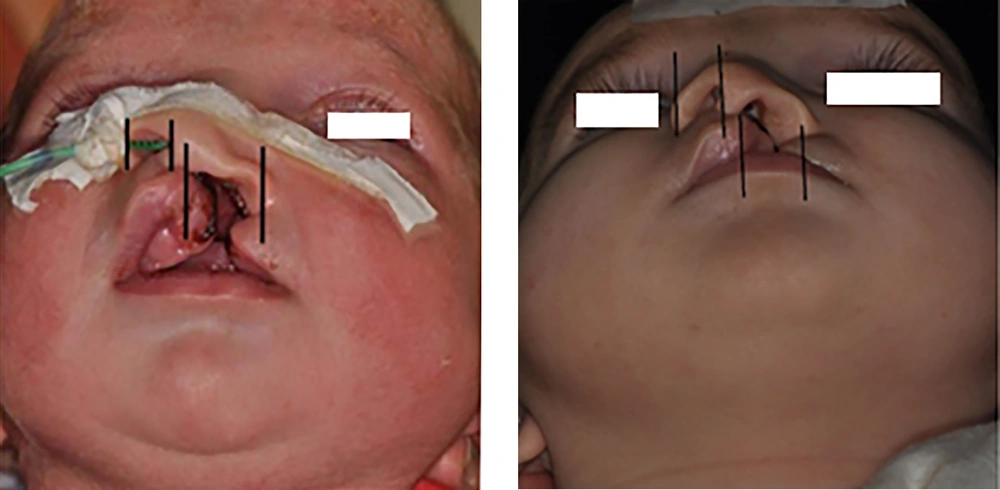
A female neonate (7 days old) with unilateral cleft lip and palate fed by nasogastric tube was referred to our department. Photographs were authorized by the patients’ parents. At the beginning and end of treatment, an impression with silicone elastomer (Coltene/Whaledent, Germany) was taken from the maxillary arch with awaken prone lying patients. Before lip surgery, the patient received pre-surgical therapy with the nasal elevator device and tape for three months (Figure 1). The first two square form tapes were adhered to the left and right cheeks and then the tapes were crossed horizontally from the right cheek to the left cheek. These tapes were anti sensitive and were replaced by parents every day. The unilateral nasal stent was made from a 0.7 mm stainless steel wire, which was attached to acrylic resin (Acropars, Iran) at its end. The acrylic resin was covered by a thin layer of soft liner (Coe-soft, GC America INC, USA). It also had a hook at the other end. There was an orthodontic elastic band (Dentaurum, 5/16 inch diameter, Munich, Germany) for traction fixed with tape to the forehead in the appropriate vector and attached to the hook at the other end. Tension was applied until minor blanching of the skin was seen (Figure 2). The parents were taught on how to use and replace the tapes and were instructed on how to clean the nasal stent daily and adjust the magnitude of tension as needed, upon observing any skin irritation of nostril. The patient was observed every week to check the nasal elevator. After NAM, the patients underwent lip surgery for complete reconstruction of the lip and nose (Figure 3).
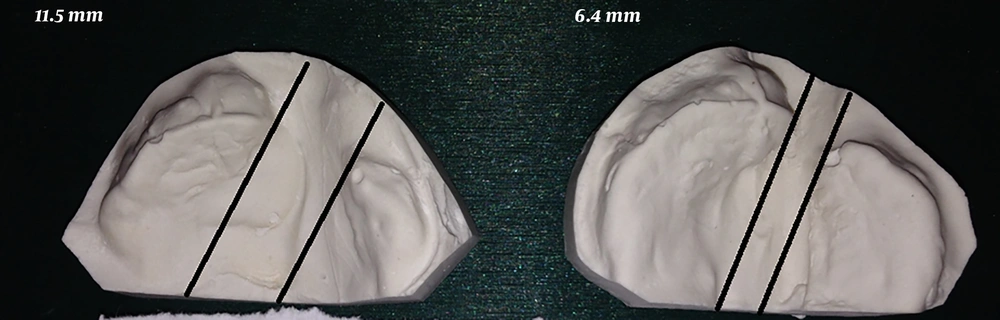
Cleft width, anterior arch width, and arch length were measured on the maxillary casts. Standard anterior position and worm-eye view photographs were taken before and after treatment. The magnification of all images was kept constant. Columellar deviation angle, nostril width and height, intercommissural distance, and soft tissue cleft width were all measured based on the photographs (Figures 4-8). Linear measurements were done directly using a ruler; a goniometer was used to measure columellar angles. To assess the improvement in the size of the soft tissue cleft, the ratio between the intercommissural distance and the soft tissue cleft was calculated for the cleft and non-cleft nostrils.
Measurements on maxillary cast showed that the cleft width was reduced to 5.1 mm (pre-treatment: 11.5 mm, post-treatment: 6.4 mm), the anterior arch width was reduced to 1 mm, and arch length was reduced to 2.5 mm. Measurements on photographs showed that columellar deviation angle increased 20 degrees. The initial nostril width ratio was 2.8 and the post-treatment nostril width ratio was 1.7. The initial nasal height ratio was 0 and the post nasal height ratio was 0.8. The initial cleft width in the soft tissue was 11.5 and the post-treatment ratio was 6 (Figures 4-8 and Table 1).
| Cleft Width; Cast, mm | Anterior Arch Width, mm | Arch Length, mm | Columellar Deviation Angle, º | Nostril Width Ratio | Nasal Height Ratio | Cleft Width; Soft Tissue, x, mm | Intercom-Misural Distance, y, mm | x/y | |
|---|---|---|---|---|---|---|---|---|---|
| Before | 11.5 | 32.5 | 27 | 25 | 2.8 | 0 | 11.5 | 33 | 0.34 |
| After | 6.4 | 31.5 | 24.5 | 45 | 1.7 | 0.8 | 6 | 35 | 0.17 |
3. Discussion
Pre-surgical NAM has been used by many groups (5, 9-12). NAM has some advantages in comparison with the primary surgical correction of the nose and lip. NAM actively molds the symmetric nasal cartilage and alveolar cleft and leaves less scars and fistula; therefore, the need for secondary alveolar bone grafts is reduced (1).
So far, many studies have been conducted to evaluate the effect of NAM. Ezzat et al., observed a significant reduction in the distance of displaced segments and increase in the maxillary arch width (13). Spengler et al., reported that there was a significant improvement in the nasal symmetry in bilateral CLP patients and the shape of arch was improved (14). Baek et al., used 3D analysis and found that the cleft gap was significantly reduced after NAM (15). Shetty et al., concluded that patients before one month of age benefit the most from NAM effects on nasoalveolar morphology, although older patients still benefit to a lesser extent (16).
The conventional technique was very difficult for parents to manage and it also injured the oral mucosa, therefore, many parents refused to use this appliance. Monasterio used the nasal elevator plus the DynaCleft instead of intraoral appliance with nasal stent for NAM. This technique eliminated the need to take impression from neonate and it was so easier to handle. In conventional NAM, the appliance acts directly on the maxillary flanges while nasal elevator functions indirectly on the maxillary segments by lip’s traction pressure. Monasterio et al., compared the conventional NAM technique with NAM plus DynaCleft and concluded that both methods significantly reduced the cleft width and improved the nasal asymmetry (8).
However, it should be mentioned that the use of DynaCleft increases the cost of treatment. In our case we used anti-sensitive tape (3M, USA) instead of DynaCleft to make treatment more affordable for the family of the patient. The cleft width was reduced as shown in Figure 3 and the nasal architecture was improved. We have not observed any complications during treatment and follow-up sessions. Therefore, our study shows that NAM, with nasal elevation, can reduce the cleft width and improve the nasal architecture significantly.