1. Background
Hallux valgus (HV) is a medial deviation of the first metatarsal and lateral deviation and/or rotation of the hallux, which can cause dislocation of first metatarsophalangeal joint (MTPJ) (1-3). Pes planus, primary varus of first metatarsus, rheumatoid arthritis, collagen deficiency, neuromuscular disorders, dislocation of MTPJ, and genetic predisposition are the internal risk factors; shoes with high heels and a narrow toe head are the most common external risk factor of HV (2-5). HV is three to five times more prevalent in women than men and its prevalence is estimated as 23% in adults with the age range of 18 - 65 years and 35.7% in individuals older than 65 years (6).
Although most HV patients have no pain or limitation of leg movement, in certain cases, HV can induce inflammation, redness and pain around the MTPJ, corns and calluses, intermittent or persistent pain, and movement limitation of MTPJ (7, 8). In mild cases of HV, non-surgical methods are used to reduce pressure to first MTPJ. These include exercise and use of appropriate shoes, orthotic latex, and overnight splints (9). However, joint deformity, pain or difficulties in wearing shoes, and limitation or inhibition of movement are indications of surgical therapy of HV. There are several surgical methods for HV treatment including capsulotendon balancing or exostectomy, resectional arthroplasty, first MTPJ arthrodesis, bunionectomy, and osteotomy; the main goals of all of them are pain elimination and correction of the deformity of the first leg toe (9). Among them, osteotomies such as proximal crescentic, proximal chevron, proximal opening wedge, Ludloff, Mau, closing wedge, and scarf are the most successful methods in treatment of HV, due to resection and true correction of bone and joint (3, 4, 9).
Previous studies demonstrated that proximal crescentic osteotomy (PCO) and proximal opening wedge osteotomy (POWO) had better outcomes concerning decreasing pain, correcting HV and intermetatarsal angles, and improving function and patients’ satisfaction (1-3, 9). However, there are disagreements between scientists about the preferred method in the treatment of HV.
2. Objectives
Therefore, in the current study we aimed to evaluate and compare the therapeutic general outcomes of PCO and POWO of first metatarsus in patient with moderate to severe HV. We hypothesized that the functional outcome and patients’ satisfaction may be better in the POWO technique.
3. Methods
3.1. Patients
The protocol of this retrospective analytical study was approved by the Ethical Committee. Totally, 110 moderate (HV angle: 21° - 39°, intermetatarsal angle: 9° - 11°) and severe (HV angle ≥ 40°, intermetatarsal angle ≥ 18°) unilateral HV patients who underwent osteotomy in an academic referral center were enrolled. They were categorized in PCO (n = 58) as the first group and POWO (n = 52) as the second group. All patients were operated by one surgeon (First author) with the PCO method from September 2010 to October 2012 and with the POWO method from November 2012 to September 2015.
3.2. Surgical Interventions
Patients were placed in the supine position and general anesthesia following with administration of thigh tourniquet were performed for all patients in both groups. Medial bunionectomy of apex of first metatarsus and release of adductor halluces tendon, medial, and lateral capsules of the first MTPJ and transverse metatarsal ligament were performed in both groups. In the first group, the senior author performed all operative interventions according to the procedure described by Coughlin and Mann (10, 11). Through the dorsal approach and using a crescentic sawblade, a crescentic osteotomy with the concave surface was done 1 cm distal to the metatarso-cuneiform joint. The metatarsal shaft is rotated laterally and the osteotomy was kept using two smooth cross pins. The end of the pins was bent, placed under the skin, and then removed after 6 weeks.
In the second group (10, 12), longitudinal capsulotomy of the first MTP joint and excision of medial bunion was considered. After creating a medial midline incision from the base of the first metatarsus, an osteotomy of the base of 1st metatarsal was made perpendicular to the shaft with direction from the dorsomedial to plantarlateral. Since the lateral cortex of base of first metatarsus was intact and osteotomy place was filled with extracted autologous bunion bone of medial side, the surgical place was stable and pins were not applied, except in four cases.
3.3. Postop Rehab
All patients were advised to have NWB for four weeks and were then allowed to partially bear the weight as they tolerated; we did not recommend any kind of special splint slap or supports.
3.4. Evaluations
Patients were followed-up every 2 weeks in the first two months’ post-operation and then followed up at three and six months. Demographic information and data was related to the side of involvement, severity of HV, changes in HV and intermetatarsal angles, MTPJ status, visual analogue scale (VAS) of pain, and patients’ satisfaction; functional status of patients pre- and post-operation based on American Orthopedic Foot and Ankle Society (AOFAS) score were recorded. AOFAS scores between 91 - 100 were considered as excellent, 81 - 90 as good, 71 - 80 as fair, and ≥ 70 as poor. Also, data about post-operative complications such as discomfort, pin tract infection (PTI), Varus deformity, and relapse of the valgus deformity were extracted from their medical records. All patients were recalled for a final follow-up in March of 2016 and were followed again for all of the above-mentioned parameters.
3.5. Statistical Analysis
All data were inserted in SPSS version 19 and analyzed using chi-square and two independent sample t-tests. P < 0.05 was considered as significant difference.
4. Results
Thirteen cases in the PCO group and nine cases in POWO group were lost to the follow-up. Finally, 45 patients with PCO (5 males (11.1%) and 40 females) with a mean age of 39.68 ± 8.08 years were included in the study. In the POWO group we included 43 cases (5 males (11.6%) and 38 females) with the mean age of 35.36 ± 12.65 years. No significant differences were detected in gender (P = 0.939), mean age (P = 0.058), age categories (P = 0.768), and side of involvement (P = 0.996) between the two groups. Mean follow-up time was 5.3 and 3.2 years in PCO and POWO groups, respectively. There were no loss of correction in any of the groups at the final follow-up.
Discomfort in the pin area was seen in 18 patients of the PCO group and among them, three patients were treated successfully with antibiotics due to superficial PTI. Of all POWO patients, four cases were needed to be fixed with pin, of whom, one patient had discomfort in the pin site. Demographic information and clinical data of both PCO and POWO groups at pre- and post-operation are presented in Table 1.
| PCO (N = 45) | POWO (N = 43) | P Value | |
|---|---|---|---|
| Male:female | 5:40 | 5:38 | 0.939 |
| Age, y | 39.68 ± 8.08 | 35.36 ± 12.65 | 0.058 |
| Age group, y | 0.768 | ||
| ≤ 30 | 6 (13.3) | 7 (12.3) | |
| 31 - 40 | 20 (44.5) | 21 (48.8) | |
| ≥ 41 | 19 (42.2) | 15 (34.9) | |
| Side of involvement | 0.996 | ||
| Right-sided | 22 (48.9) | 21 (48.8) | |
| Left-sided | 23 (51.1) | 22 (51.2) | |
| Hallux valgus severity | 0.912 | ||
| Moderate | 8 (17.8) | 8 (18.6) | |
| Severe | 37 (82.2) | 35 (81.4) | |
| AOFAS score | |||
| Pre-operative | 43.1±6.38 | 44.37±6.92 | 0.335 |
| The third month after surgery | 81.27 ± 6.18 | 81.10 ± 8.21 | 0.894 |
| The sixth month after surgery | 92.06 ± 6.53 | 92.5 ± 6.87 | 0.714 |
| Current reexamination | 94.75 ± 6.72 | 94.13 ± 12.4 | 0.734 |
| AOFAS (excellent/good/fair/poor) | |||
| Pre-operative | 45/0/0/0 | 43/0/0/0 | |
| The third month after surgery | 1/24/17/3 | 1/22/51/5 | |
| The sixth month after surgery | 26/16/3/0 | 30/10/3/0 | |
| Current reexamination | 36/7/2/0 | 38/4/1/0 | |
| VAS for pain | |||
| Pre-operative | 7.96 ± 1.18 | 7.96 ± 1.09 | 0.996 |
| The third month after surgery | 2.04 ± 0.90 | 1.98 ± 1.43 | 0.762 |
| The sixth month after surgery | 0.83 ± 0.89 | 0.74 ± 0.77 | 0.558 |
| Current reexamination | 0.47 ± 0.97 | 0.35 ± 0.71 | 0.447 |
| VAS for patient | |||
| Pre-operative | 2.01 ± 1.57 | 2.08 ± 1.55 | 0.834 |
| The third month after surgery | 7.96 ± 1.11 | 8.91 ± 1.62 | 0.0001 |
| The sixth month after surgery | 9.14 ± 1.18 | 9.25 ± 0.95 | 0.588 |
| Current reexamination | 9.32 ± 1.15 | 9.35 ± 0.89 | 0.439 |
| Hallux valgus angle | 0.841 | ||
| Pre-operative | 38.06 ± 10.47 | 38.86 ± 11.33 | |
| Post-operative | 14.68 ± 5.22 | 15.15 ± 5.2 | |
| Intermetatarsal angle, degree | 0.841 | ||
| Pre-operative | 14.37 ± 3.89 | 14.66 ± 4.08 | |
| Post-operative | 6.47 ± 2.93 | 6.42 ± 2.82 | |
| Postoperative complications | 0.599 | ||
| Varus deformity | 3 (6.7) | 2 (4.6) | |
| Relapse of the valgus deformity | 3 (6.7) | 1 (2.3) |
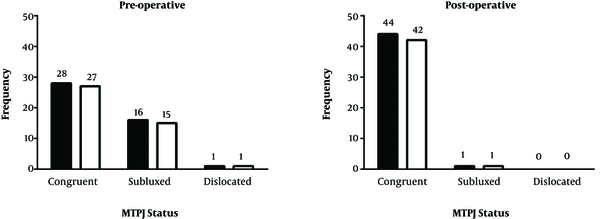
Mean VAS of patients’ satisfaction in the 3rd month follow-up in the POWO group was significantly higher than the PCO group (P = 0.0001). However, this value showed insignificant difference between the two groups at six months and final follow-up. No significant differences were detected in the AOFAS scale in any of the follow-up periods between the two groups (P = 0.570). Mean VAS of patients’ pain and satisfaction, AOFAS score, HV, and intermetatarsal angles showed improvement during all different follow-up periods (P = 0.0001), however, these changes were not significant between the two groups (P > 0.05). MTPJ status was significantly improved after surgery in both the PCO and POWO group (P = 0.0001, Figure 1).
As shown, pre-operative congruent status was seen in 28 (62.2%) and 27 (62.8%) patients in the PCO and POWO groups. Although this status increased after surgery and was seen in 44 (97.8%) and 42 (97.7%) patients in the PCO and POWO groups, respectively, MTPJ status was not significant different between two groups, neither pre-operative (P = 0.997) nor post-operative (P = 0.974).
5. Discussion
MTPJ dislocation in HV patients can cause a progressive deformity and induce pain and dissatisfaction. Soft tissue surgeries or distal first metatarsal osteotomies can be used for mild to moderate cases, however, in moderate to severe cases, proximal first metatarsus osteotomies are recommended (7-9). PTI is a common complication after orthopedic interventions, which can increase the duration of follow-up, induces osteomyelitis, and forces antibiotic therapy or surgery. Patients and surgical related risk factors, pin characteristics, use of prophylactic antibiotics, and post-operative pin care conditions are important factors in induction/prevention of PTI. In most cases, PTI was treated by wound care and use of oral antibiotics. Nonetheless, in severe cases, which do not respond to antibiotic therapy, pin extraction must be performed (13). In the present study, PTI occurred in only three patients in the PCO group at four weeks after surgery and all of them successfully responded to the antibiotic therapy. No PTI was detected in four patients in the POWO group who received pin.
We found improvements of patient’s satisfaction in all follow-up times in both groups. In addition, patient’s satisfaction in the 3rd month after operation in the POWO group was significantly higher than the PCO group, however, in the 6th month and final follow-up no significant differences were seen between the two groups. Lower short-term patient satisfaction in the PCO group may be due to pin application in all patients, possible infection, inherent instability, and lack of allowance to put weight on the surgical area. Our findings regarding both methods are in line with previous studies. For instance, Zettl et al. (14) evaluated 96 moderate to severe HV patient (114 legs) who underwent PCO of metatarsus and distal soft tissue surgery and found 91% of patient satisfaction as good or excellent. Also, Shurnas et al. (15), investigated the outcomes of POWO of metatarsus using arthrex LPS (R) first metatarsal system in 78 patients (84 legs) for mean follow-up of 2.4 years. They found that 90% of patients reported good to excellent outcomes (15).
We found obvious improvement in the mean of AOFAS score at all follow-up times in both PCO and POWO groups. In line with our findings, Chow and collaborators reported that the mean AOFAS score was increased from 57.9 to 90.5 during 2.7 years follow-up in 26 HV patients (32 legs) who underwent plate fixation for metatarsal crescentic osteotomy (16). Also, in another retrospective study, an increase in mean AOFAS score from 51.3 to 86.8 was detected in 64 legs, which were operated using POWO by help of low profile plate for correction of HV in mean follow-up of 20 months (17). Based on the occurrence of discomfort in 19 cases among 53 patients with pin, it seems that use of low profile plate can be helpful in treatment of HV.
In this study, pain decreased significantly during the follow-up period in both groups. This finding is in agreement with those reported previously. Shurnas et al. (15) reported that the VAS of pain decreased from 5.9 ± 2.2 to 0.5 ± 0.8 after surgery. Badekas et al. (12), in a retrospective study evaluated 85 cases (107 feet) with moderate to severe hallux valgus. The operation technique was POWO using a medially applied locking plate for osteotomy fixation. The mean pre-op to post-op HV angle was 39 and 11.8 degrees, respectively. They found the POWO technique to be safe and reproducible.
In addition, Chuckpaiwong (18) evaluated the outcomes of 125 proximal and distal metatarsus osteotomies of moderate to severe HV and found that although patients in both groups experienced lower pain, no significant differences existed between the two groups after one year follow-up. In addition, Mann et al. (19), evaluated the outcomes of 75 patients (109 legs) with HV deformity who underwent soft tissue releasing, cutting of medial eminence, plication of internal part of capsule, and PCO of first metatarsus for 34 months follow-up in a retrospective study. They found a decline in HV angle from 31° to 9° after operations (18). This improvement in HV angle was 14.7° in the Saragas report (17). Although, improvements in the intermetatarsal angle after surgery in both PCO and POWO groups were detected, these two groups showed no significant difference together. A mean decrease of 8° and 8.3° in intermetatarsal angle after PCO and POWO were also reported by Mann et al. (19), and Saragas (17), respectively.
No significant differences were detected between pre- and post-operative HV severity in any of the groups. Also, no significant differences were detected in post-operative complications between two groups; all complications were seen just in severe HV. Our detected complications were lower than all previous reports and also differed in types. Cooper et al. (20), reported that open wound, drifting of HV angle, and delay in union were the major complications in 23 HV patients who underwent POWO of metatarsus and combination of distal soft tissue and exostomy. Smith reported that the most complications after POWO of metatarsus in 47 HV patients (49 legs) were mild inflammation, nonunion, and delayed union (21).
One of the limitations of this study is the low number of patients, which decreases the value of generalizability of the study. Performing studies with longer evaluation time is recommended for better evaluation of post-operative complications. Also, it is recommended that future studies would be performed in multicenter academic hospitals with randomized design to lower the biases. Due to the inherent instability of the PCO, the pin insertion was mandatory; this was the main reason that we changed our protocol to the POWO technique. Usually surgeons change their protocol to perform an operation with better outcomes. It is inevitable to have such bias in every “change protocol studies”, which caused another limitation in our study.
5.1. Conclusions
Conclusively, based on our findings it can be said that both osteotomies showed beneficial outcomes, however, patient satisfaction in short-term follow-up was higher in the POWO group in comparison to the PCO group. Therefore, in similar conditions, POWO is highly recommended for patients with moderate to severe HV.