1. Background
A major dilemma following the extraction of impacted mandibular third molars is the inferior alveolar nerve (IAN) bundle injury (1). A precise preoperative evaluation of the relationship between IAN and the mandibular third molar roots can help us predict and potentially prevent sensory impairments (1, 2). A close relationship has been established between the third molars and the mandibular canal, suggesting the higher risk of IAN injury (3). Narrowing, diversion, and loss of the cortical lines of IAN, interruption of the lamina dura, and root darkening are among the most important radiological markers, indicating a close relationship between the mandibular canal and the third molars (4-7).
A novel radiographic marker is the juxta-apical radiolucency (JAR), which is known as a significant prognostic marker of IAN injury due to third molar surgery. This marker appears as a well-circumscribed radiolucent region lateral to the root of the third molar rather than the apex on panoramic radiographic images (8). To the best of our knowledge, only few studies have evaluated JAR, and controversial results have been reported regarding the relationship between JAR and IAN.
Nascimento et al. found that JAR was in contact with the IAN canal (4). Conversely, Kapila et al. reported no close relationship between JAR and IAN (9). Evidence suggests that mandibular cortex preservation is essential for inhibiting injury to IAN (10-12). However, few studies have suggested that JAR is associated with cortical thinning (4, 9, 13). In this regard, a previous study showed that JAR may lead to the increased occurrence of paresthesia following the extraction of third molars (13). Considering the discrepancies between the results of previous studies, further investigation is necessary in this area.
2. Objectives
In the present study, we hypothesized that JAR is a continuity of IAN; therefore, we evaluated its relationship with IAN on cone-beam computed tomography (CBCT) images. We also postulated that JAR leads to thinning of the cortical bone.
3. Methods
The Local Ethics Committee of Shiraz University of Medical Sciences approved this descriptive, cross-sectional study (No: #IR.SUMS.REC.1394.S1117). From an initial sample of 450 cases, we selected 20 patients with JAR (a well-defined radiolucent area lateral to the lower third molar root). Besides, we selected 20 age-matched patients without JAR from the archives of a maxillofacial radiology center.
The inclusion criteria were a close relationship between IAN and the third molar in the control group and the presence of JAR in the case group. On the other hand, the exclusion criteria were as follows: (1) the presence of a carious lesion; (2) large restorations; (3) endodontic treatment; and (4) other pathologies, including cysts or tumors of the third molars. The CBCT images were obtained, using a flat panel detector (FPD)-based CBCT system (NewTom VGi, QR srl, Italy). Each study was performed after adjusting the following parameters: current of 110 kVp; exposure time of 3.6 sec; and field of view of 8 cm × 8 cm.
To acquire the CBCT images, the subjects were positioned with the Frankfort plane parallel to the floor. The CBCT images were analyzed using NNT viewer software. The multi-planar reconstructed (MPR) images were studied in the third molar area with a slice thickness of 0.3 mm and an interslice gap of 0.3 mm. The CBCT images of the JAR group were evaluated in the corrected coronal and axial planes to determine the JAR location (i.e., lingual, buccal, inferior, or superior) relative to IAN. The relationship between JAR and IAN was characterized as separate or direct contact.
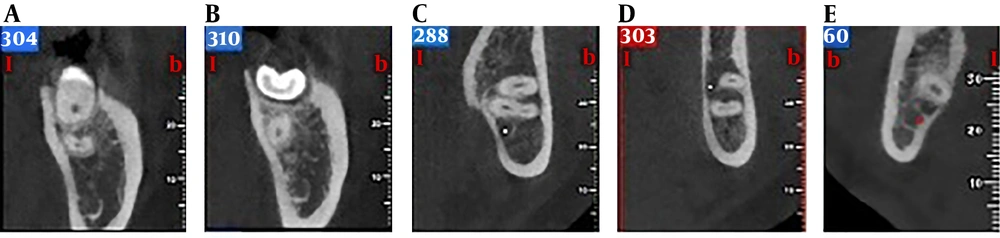
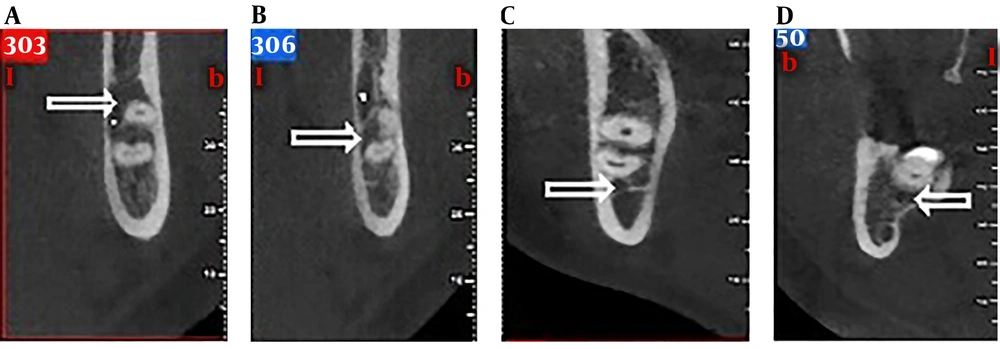
Moreover, the minimum thickness of the adjacent cortical plates was evaluated, based on a classification proposed by Kapila et al. (9). We also added two more types (J0 and J4) to their classification, which had not been considered (Table 1 and Figure 1). The CBCT images of the control group were also evaluated in the axial and corrected coronal planes to determine the third molar position relative to the mandibular canal (buccal, lingual, superior, and inferior) (Figure 2) and thinning of the cortical plates.
| Classification | Details |
|---|---|
| J0 | The cortical plate was not thinned. |
| J1 | The remaining cortical plate thickness was three-fourth of the maximum thickness. |
| J2 | The remaining cortical plate thickness was half of the maximum thickness. |
| J3 | The remaining cortical plate thickness was one-fourth of the maximum thickness. |
| J4 | The cortical plate was perforated. |
The analysis of data was performed in SPSS version 23 (SPSS Inc., Chicago, IL, USA). The results of case and control groups were compared, using descriptive tests and Chi-square test. The significance level was set at P < 0.05.
4. Results
The CBCT images of 40 patients, including 20 patients with JAR and 20 patients without JAR, were examined in this study. The case group included four males and 16 females, whereas the control group included seven males and 13 females. The mean age of the two groups was 25 years.
Evaluation of the JAR location relative to IAN showed that JAR was buccal to IAN in 55% of cases, lingual to IAN in 10% of cases, and superior to IAN in 35% of cases (Table 2). In the control group, the root apex was buccal to IAN in 15% of cases, lingual to IAN in 55% of cases, and superior to IAN in 30% of cases. There was a significant relationship between the location of JAR relative to IAN (P = 0.004). The association between JAR and IAN showed that in the majority of cases, JAR was in contact with IAN (P = 0.001). The lingual cortical plate was perforated in 75% of cases with JAR versus 45% of cases in the control group (P = 0.06) (Table 3).
| Position | JAR Group (%) | Control Group (%) | P Value |
|---|---|---|---|
| Buccal | 11 (55%) | 3 (15%) | 0.004 |
| Lingual | 2 (10%) | 11 (55%) | |
| Superior | 7 (35%) | 6 (30%) |
| Cortical Plate Thinning | J0 | J1 | J2 | J3 | J4 |
|---|---|---|---|---|---|
| JAR group | 0 | 2 (10%) | 1 (5%) | 2 (10%) | 15 (75%) |
| Control group | 2 (10%) | 2 (10%) | 4 (20%) | 3 (15%) | 9 (45%) |
| P value | 0.06 |
5. Discussion
The trigeminal nerve is the largest peripheral sensory nerve in the body. Damage to this nerve is considered the most challenging sequel of dental surgeries (8). Iatrogenic injuries to the third division of the trigeminal nerve, including IAN and the lingual nerve, remain complicated clinical problems. According to most previous studies, the incidence rate of injury ranges from 0.5% to 8%. However, these rates are attributed to nerve injury when the third molars are extracted with different degrees of difficulty.
The incidence of nerve damage is speculated to reach as high as 23% - 35% when there is a close connection between the tooth and IAN (14-18). Therefore, a precise preoperative radiographic evaluation is considered indispensable before the extraction of the third molars (18). On the other hand, panoramic radiography provides 2D images and cannot provide reliable or sufficient information for predicting nerve injury. CBCT has overcome this limitation and can be used as a suitable alternative if there is a close relationship between the mandibular canal and the third molar roots (4, 19).
Besides radiological markers, which represent a close relationship between the third molars and IAN, JAR is also a new radiographic sign, associated with paresthesia after removing the mandibular third molars (10). JAR has been shown to be a key predictor of IAN damage following the removal of third molars. Recent studies have used CBCT to clarify the relationship of JAR with IAN. In this regard, Nascimento et al. found that in most patients, JAR was in contact with the IAN canal (4). Similarly, in the present study, evaluation of the anatomic relation between JAR and IAN showed that in many cases, JAR was in contact with the canal (P = 0.001). Conversely, in another study, the relationship of JAR with the mandibular canal was ruled out because of the dissociation of JAR from the canal (9).
Generally, knowledge of the cortical plate thickness is of crucial importance, as cortical plate thinning may be one of the factors, resulting in the increased occurrence of paresthesia. There is scarce information regarding the effect of JAR on the cortical plates (20). In the present study, the cortical plates were perforated in 75% of cases in the JAR group at a given resolution (0.3 mm). There was an almost statistically significant increase in the perforation of cortical plates in the JAR group, compared to the control group (P = 0.06). In contrast, only one case of lingual cortical puncturing was seen in the study by Nascimento et al. (4).
In a study by Kapila et al., none of the patients with JAR showed perforation of the cortical plate on CBCT images (9). In the present study, the cortical plate thinning was observed in 100% of cases in the JAR group. Nevertheless, cortical thinning associated with JAR was observed in 46.8% of cases in the study by Nascimento et al. (4). In their study, when the mandibular canal was situated lingual to the root of the third molars, patients were at a higher risk of IAN damage (4). The position of IAN was lingual to JAR in 55% of cases. This result contradicts previous studies, which demonstrated the presence of JAR in 30% of cases on the buccal side (9).
Several researchers have indicated that JAR may be a continuity of IAN lamella (9-11). However, Umar et al. reported that JAR originated from the cancellous bone space (12). The results of the present study revealed that JAR is not only a cancellous bone, because it affected the cortical plates, and more importantly, it was in contact with the IAN canal in most cases. Our findings were consistent with the results of previous studies and confirmed the hypothesis that considers JAR as a sign of increased IAN injury risk.
In conclusion, based on the present results, JAR was in contact with IAN in most cases. The cortical plates were thinned in all cases of JAR. Also, JAR was located lingual to IAN in 55% of cases. However, because of the limitations of the present study, we suggest further research to investigate the incidence of paresthesia following third molar surgery if JAR is present.