1. Background
Delirium is a common problem in elderly patients (1). Acute signs of delirium, caused by abnormalities in the brain cognitive processing, are marked by decreased ability to concentrate or change thoughts, confusions, or changes in the level of consciousness (2). Patients in intensive care units (ICU) are prone to developing delirium (3). According to previous studies, the incidence and prevalence of delirium vary extensively in different communities. Evidence shows that 10% - 30% of admitted patients in general hospitals develop delirium, and a prevalence rate of up to 60% has been reported in elderly patients (4).
In a study from Italy on hospital-admitted patients, the prevalence of delirium was estimated at 22.9% (5). Moreover, delirium developed in up to 50% of hospitalized elderly patients in the United States (6). In Iran, the prevalence of delirium ranges from 22% to 44.5% in ICU patients (7, 8). An incidence rate of 43% was reported in postoperative elderly patients (9). On the other hand, in another review study, the incidence of postoperative delirium ranged from 0% to 73.5% (10). This broad range is associated with the patient groups under investigation, differences in appraisal tools, repetition and duration of delirium assessment, evaluators’ skills, and type and dosage of used drugs (11).
Generally, patients with delirium have a poor prognosis (9). Nevertheless, our understanding of the etiology of delirium remains limited (12). Delirium is not the outcome of one single cause, but multiple factors, including aging, male gender, dementia, hearing and visual impairments, cognitive dysfunction, drug use, alcoholism, comorbidity, stroke, and depression, seem to be involved (13, 14). Evidence suggests that prevention or control of delirium is quite feasible. Some of the negative consequences of delirium include high morbidity and mortality, suffering of patients and families, and major burden on healthcare settings. Considering the consequences of delirium, it is necessary to take effective measures.
The aim of this study was to evaluate three-month mortality among delirium patients and to determine relevant risk factors for mortality in patients who were admitted to a general hospital due to different reasons. Most previous studies have investigated individual risk factors for delirium in patients with specific diseases (15) and clinical conditions (16), such as postoperative patients (17-20), patients admitted to critical care units (e.g., intensive care unit (20-22) and coronary care unit (15)), and acute patients admitted to internal medicine wards (18).
In recent years, the population pyramid of Iran has shown an ever-increasing trend in the elderly population. In fact, we are faced with major challenges related to population aging and its outcomes in Iran (23). In order to ensure a higher quality of life for the elderly and their families, we need to reduce the associated morbidity and mortality.
2. Objectives
The purpose of this study was to evaluate the presence of delirium and to identify the correlated risk factors in an Iranian sample of hospitalized elderly patients in North of Iran.
3. Methods
3.1. Study Design
This prospective, observational, cohort study was conducted at a university-affiliated, 340-bed hospital in Sari, Iran. The Research Ethics Committee approved the study. Eligible patients were selected via available sampling. The study sample included 100 delirious patients, who received psychiatric counseling in different wards of the hospital between January 2018 and October 2018. All consecutive patients (minimum age, 18 years), who were admitted to the hospital with a Glasgow Coma Scale (GCS) score of at least 10, were recruited in the study. Intubation was not performed during analyses. All participants were able to communicate with the researchers. Informed consents were collected from the participants or their relatives.
Upon enrollment and during the first week of hospitalization, the psychiatric resident screened eligible patients for delirium using Neecham Confusion Scale (NCS), which is a nine-item questionnaire evaluating orientation, memory, and concentration via interview. A trained research assistant, who was blind to the study, interviewed a family member and collected the data. NCS was completed in the following intervals: consulting day, three days after consultation, discharge day, one-month follow-up, and three-month follow-up. Date of death during the follow-up was confirmed by the research assistant via telephone calls. Moreover, laboratory and clinical data, as well as the patients’ characteristics (i.e., age, sex, and alcohol/substance use), were recorded in the baseline forms.
3.2. Delirium Assessment
The Persian version of NCS was used to screen the patients for delirium (17). Neelon et al. developed this scale to diagnose delirium in the elderly and to observe changes in its severity. It was first evaluated in non-intubated ICU patients, showing acceptable psychometric features (specificity, 82%; sensitivity, 97%) (24). Nine items are included in this scale, which are classified into three subscales: subscale I, information processing (score, 0 - 14) including cognitive status (e.g., alertness, verbal and motor responses, and memory); subscale II, behaviors (score, 0 - 10) including observed behaviors and performance ability (e.g., verbal responses, sensory-motor performance, and general appearance); and subscale III, performance (score, 0 - 16), including vital functions (e.g., oxygen saturation, vital signs, and urinary incontinence).
The total NCS score is the sum of scores of three subscales. The scores of these subscales are summed up to determine the total score of NCS, ranging from 0 (no response) to 30 (normal) (25). The following cut-off points have been established for delirium: scores 0 - 19, moderate to severe delirium and/or confusion; scores 20 - 24, early or mild delirium and/or confusion; scores 25 - 26, high risk of delirium and/or confusion; and scores 27 - 30, no confusion and/or delirium and normal cognition.
3.3. Assessment of Risk Factors
A complete history of health problems related to delirium risk factors was collected from the patients and their families upon admission, including polypharmacy, hypertension, diabetes, dementia, cancer, surgery, substance abuse, infection, cardiovascular and renal problems, metabolic and electrolyte disturbances, stroke, and speech, visual, and hearing impairments. In addition, laboratory exams, including complete blood cell count (CBC), platelet (PLT) count, blood urea nitrogen (BUN), creatinine, erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), liver function test (LFT), and sodium (Na), potassium (K), calcium (Ca), and glucose levels, were measured.
3.4. Statistical Analysis
For statistical analysis, SPSS V. 20.0 was used. Descriptive statistics (e.g., mean, percentage, standard deviation, and frequency) were measured for data analysis. The relationship between variables was examined using correlation analysis and Independent t-test. In addition, multivariate logistic regression analysis was carried out to evaluate the association of delirium with other dependent variables. Three-month mortality was determined based on Cox regression model for survival data with adjustments for covariates. Also, a logarithmic test was applied to compare survival between subgroups in a single-variable mode. The significance level was set at 0.05, and the statistician was blind to the study.
4. Results
Of 100 patients participating in this study, 76% were male and 24% were female. The mean age of the participants was 79.9 ± 15.1 years. With respect to gender, the mean age of men was 71.15 ± 4.4 years, and the mean age of women was 64.5 ± 14.4 years; however, the gender difference was not significant. With respect to comorbidities, 23% of patients had cancer, 17% had renal disorders, 16 had diabetes, 15% were hypertensive, and 15% were diagnosed with a pulmonary disease. Clinical characteristics of the study population are presented in Table 1.
| Characteristics | Values |
|---|---|
| Admittance service (%) | |
| Internal medicine | 48 |
| Surgery | 15 |
| Gastroenterology | 15 |
| Respiratory care unit (RCU) | 10 |
| Intensive care unit (ICU) | 6 |
| Oncology | 5 |
| Psychiatry | 1 |
| Outcomes of delirium (%) | |
| Full recovery | 48 |
| Relative recovery | 39 |
| No recovery | 13 |
| Underlying disorders (%) | |
| Multiple comorbidities | 25 |
| Cancer | 23 |
| Renal failure | 17 |
| Diabetes mellitus | 16 |
| Hypertension (HTN) | 15 |
| Pulmonary infections | 15 |
| Trauma | 12 |
| Cerebrovascular accident (CVA) | 8 |
| Chronic obstructive pulmonary disease (COPD) | 4 |
| Loss of consciousness (LOC) | 3 |
| Cirrhosis | 3 |
| Ischemic heart disease(IHD) | 3 |
| Dementia | 3 |
| Hypothyroidism | 2 |
| Sepsis | 2 |
| Gastrointestinal disease | 2 |
| Substance withdrawal | 2 |
| Unknown | 1 |
| Predisposing symptoms (%) | |
| Medical | 83 |
| Polypharmacy | 8 |
| Trauma | 6 |
| Unknown | 3 |
| Substance abuse (%) | |
| Non | 66 |
| Opium | 22 |
| Methadone | 6 |
| Methamphetamine | 2 |
| Nicotine | 1 |
| Alcohol | |
| Laboratory assessments (%) | |
| BUN ≥ 50 mg/dL | 33 |
| Cr ≥ 1.2 | 26 |
| Hb < 12 | 21 |
| Abnormal liver function tests (LFTs) | 11 |
| Electrolyte imbalances (Na, K) | 14 |
| Hyperglycemia | 13 |
| Abnormal ESR & CRP | 3 |
| Thrombocytopenia | 7 |
| Language and sensory dysfunction (%) | |
| Speech | 2 |
| Hearing | 4 |
| Vision | 2 |
Abbreviations: BUN, blood urea nitrogen; CRP, C-reactive protein; ESR, erythrocyte sedimentation rate; LFT, liver function test.
The mean NCS score of the participants was 18.15 ± 5. The scores of NCS are presented in Table 2. The mean score of NCS increased significantly over time, indicating the improvement of disease over time (Table 3). In this group, two patients died on the third day of delirium development, 10 patients on the day of discharge, 13 patients during the four-week follow-up, and 15 patients during the 12-week follow-up.
| Time | Not Confused (%) | Mild (%) | Moderate (%) | Severe (%) | Death (%) |
|---|---|---|---|---|---|
| Day 1 | 1 | 5 | 38 | 56 | 0 |
| Day 3 | 11 | 25 | 37 | 25 | 2 |
| Day of discharge | 32 | 28 | 20 | 8 | 10 |
| 4 week follow-up | 42 | 12 | 15 | 17 | 13 |
| 12 week follow-up | 36 | 8 | 12 | 4 | 15 |
| Time | Mean ± SD | F | P Value |
|---|---|---|---|
| Day 1 | 18.5 ± 15.02 | 28.95 | < 0.001 |
| Day 3 | 21.5 ± 5.6 | ||
| Day of discharge | 24.4 ± 7.02 | ||
| 4 week follow-up | 5 ± 25.6 | ||
| 12 week follow-up | 25.6 ± 22.6 |
The rate of delirium development was significantly associated with underlying factors, including cancer, hypertension (HTN), cerebrovascular accident (CVA), cirrhosis, dementia, and substance abuse. The laboratory results showed BUN ≥ 50 mg/dL in 33% of patients with delirium, which had a significant association with NSC score (P < 0.05). Among other laboratory variables, higher ESR/CRP ratio was significantly associated with delirium (P < 0.05). The related risk factors in delirious patients are shown in Table 4.
| P Value | |||||
|---|---|---|---|---|---|
| Risk factors | First Day | Third Day | Discharge Day | 4 Week Follow-Up | 12 Week Follow-Up |
| Mean age | 0.5 | 0.37 | 0.03a | 0.06 | 0.16 |
| Gender | 0.48 | 0.4 | 0.9 | 0.6 | 0.55 |
| Admittance service | 0.06 | 0.9 | 0.07 | 0.38 | 0.17 |
| Outcomes of deliriumb | 0.73 | 0.01a | 0.04a | 0.001a | 0.03a |
| Cancer | 0.3 | 0.9 | 0.01a | 0.5 | 0.16 |
| Renal failure | 0.4 | 0.6 | 0.6 | 0.07 | 0.2 |
| Diabetes mellitus | 0.37 | 0.1 | 0.4 | 0.8 | 0.13 |
| HTN | 0.9 | 0.4 | 0.03a | 0.4 | 0.41 |
| Pulmonary infections | 0.4 | 0.9 | 0.25 | 0.21 | 0.66 |
| Trauma | 0.9 | 0.8 | 0.4 | 0.9 | 0.4 |
| CVA | 0.6 | 0.2 | 0.03a | 0.4 | 0.16 |
| COPD | 0.3 | 0.5 | 0.6 | 0.3 | 0.18 |
| LOC | 0.4 | 0.5 | 0.3 | 0.6 | 0.7 |
| Cirrhosis | 0.4 | 0.03a | 0.27 | 0.34 | 0.39 |
| IHD | 0.9 | 0.96 | 0.25 | 0.3 | 0.4 |
| Dementia | 0.9 | 0.5 | 0.2 | 0.03a | 0.08 |
| Hypothyroidism | 0.9 | 0.1 | 0.8 | 0.7 | 0.4 |
| Sepsis | 0.3 | 0.8 | 0.6 | 0.1 | 0.4 |
| Gastrointestinal disease | 0.3 | 0.8 | 0.6 | 0.1 | 0.4 |
| Substance abuse | 0.04a | 0.3 | 0.1 | 0.18 | 0.28 |
| BUN ≥ 50mg/dL | 0.03a | 0.2 | 0.7 | 0.4 | 0.8 |
| Cr ≥ 1.2 | 0.8 | 0.6 | 0.68 | 0.4 | 0.7 |
| Hb < 12 | 0.5 | 0.9 | 0.3 | 0.06 | 0.9 |
| Abnormal LFTs | 0.03a | 0.2 | 0.7 | 0.1 | 0.5 |
| Electrolyte imbalances (Na, K) | 0.9 | 0.4 | 0.9 | 0.2 | 0.4 |
| Hyperglycemia | 0.5 | 0.4 | 0.7 | 0.8 | 0.7 |
| Abnormal ESR & CRP | 0.7 | 0.03a | 0.2 | 0.3 | 0.2 |
| Thrombocytopenia | 0.6 | 0.7 | 0.3 | 0.3 | 0.33 |
| Speech impairment | 0.6 | 0.8 | 0.1 | 0.3 | 0.4 |
| Hearing impairment | 0.4 | 0.7 | 0.8 | 0.02a | 0.8 |
| Vision impairment | 0.9 | 0.1 | 0.3 | 0.6 | 0.69 |
Abbreviations: BUN, blood urea nitrogen; COPD, chronic obstructive pulmonary disease; CRP, C-reactive protein; CVA, cerebrovascular accident; ESR, erythrocyte sedimentation rate; HTN, hypertension; LOC, loss of consciousness.
aSignificant (P < 0.05).
bOutcomes of delirium: full recovery, relative recovery, and no recovery.
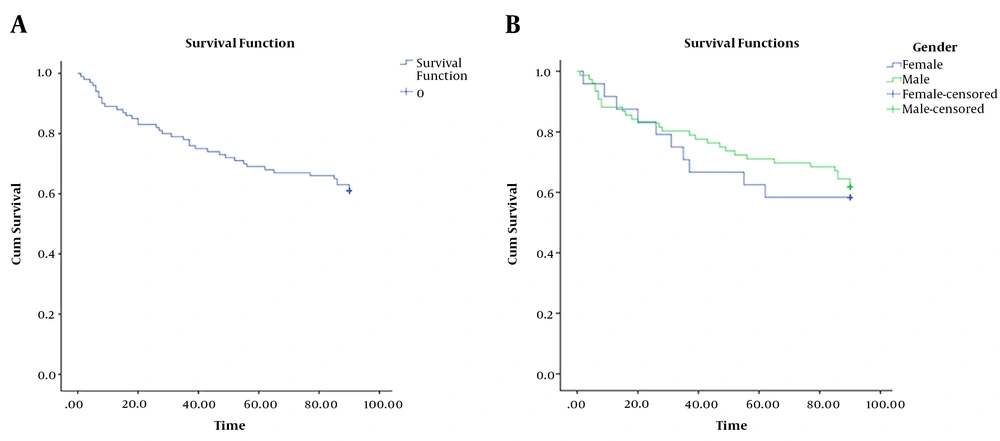
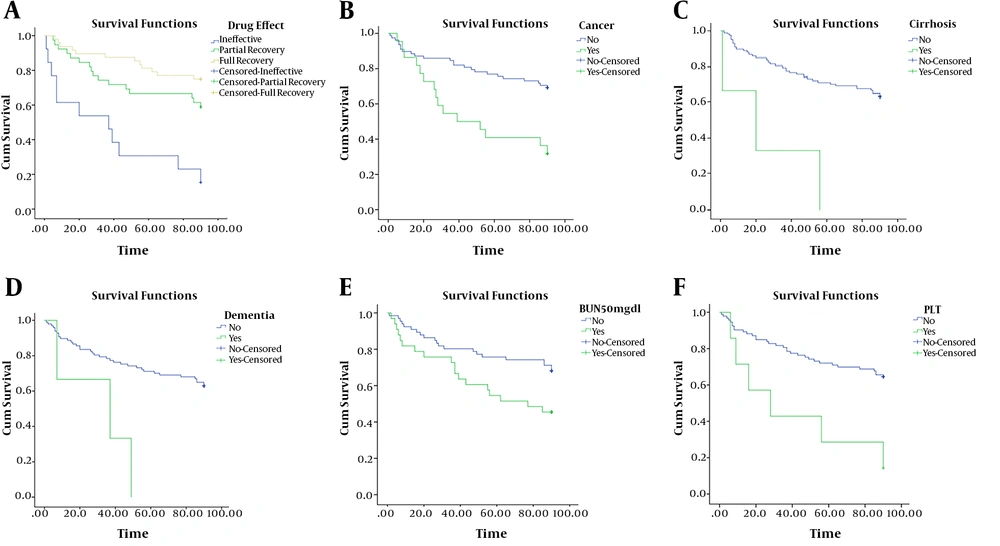
The probability of one-month survival of patients, based on Kaplan-Meier test, was 70%. The mean survival was 68.5 ± 3.23 days with a confidence interval of 62.2 - 74.9 (Figure 1A). Twenty days after hospitalization, the survival rate of women in hospitals was higher than that of men, although the difference was not significant (Figure 1B). Kaplan-Meier survival curves for effective factors, such as drug effect (P = 0.01), cancer (P < 0.001), cirrhosis (P = 0.001), dementia (P = 0.004), and BUN (P = 0.02) showed significant differences (Figure 2). The results of semi-parametric Cox regression model for survival data are shown in Table 5.
| Variable | HR | SE | Chi-Square | Sig. Level | 95% CI | |
|---|---|---|---|---|---|---|
| Upper Limit | Lower Limit | |||||
| Drug effect | ||||||
| Full recovery | 2.3 | 0.42 | 4.9 | 0.04 | 1.01 | 5.3 |
| Relative recovery | 4.6 | 0.45 | 11.4 | 0.001 | 1.9 | 11.1 |
| No recovery | - | - | - | - | - | - |
| Cancer | ||||||
| Yes | 4.1 | 0.37 | 13.8 | < 0.001 | 1.9 | 8.5 |
| No | - | - | - | - | - | - |
| Cirrhosis | ||||||
| Yes | 11.3 | 0.65 | 13.7 | < 0.001 | 3.1 | 41.1 |
| No | - | - | - | - | - | - |
| Dementia | ||||||
| Yes | 5.2 | 0.67 | 6.1 | 0.01 | 1.4 | 19.2 |
| No | - | - | - | - | - | - |
| BUN | ||||||
| Normal | - | - | - | - | - | - |
| Abnormal | 2.3 | 0.4 | 0.4 | 0.04 | 1.1 | 4.8 |
Abbreviation: BUN, blood urea nitrogen.
5. Discussion
This study aimed to determine the risk factors for delirium in a sample of elderly patients, admitted to a hospital in Sari, North of Iran. The risk factors for the development of delirium in our study sample were older age, use of multiple medications, cancer, HTN, CVA, dementia, cirrhosis, hearing impairment, and substance abuse. Almost all studies have reported a significant relationship between aging and delirium incidence (26). However, regarding gender, various studies have reported different results, showing that some women and men are more prone to delirium (27-29).
Most commonly, delirium is reported among patients with cancer, renal failure, diabetes mellitus, HTN, and pulmonary infections. Visual and hearing impairments have been confirmed as risk factors for delirium in other studies, as well (30). Cancer is considered a major risk factor for delirium (31). CVA was found in a small number of patients with delirium in our study, as it was recognized as a risk factor in the regression model. Based on a study by McManus et al., stroke is a major risk factor for delirium. Additionally, stroke, lesion volume, lesion place, reduced perfusion, and brain edema are associated with delirium (32). Therefore, both onset of stroke treatment and recovery can help prevent delirium after stroke.
Polypharmacy is another risk factor for delirium, as shown in the current study. Nevertheless, this association needs to be investigated more precisely in terms of type and amount of used drugs. Patients using multiple medications due to comorbidities need to be controlled closely for the signs of delirium (33). In the present study, substance abuse was significantly associated with poor outcomes (34), which is in line with some previous research. Careful evaluation of the patient’s history of substance abuse is also necessary. In fact, withdrawal from alcohol or other illicit substances requires special treatments.
Several medical conditions influence the development of delirium. Increase of BUN was significantly associated with the higher incidence of delirium in our patients, which is consistent with the findings of other studies (35). In the current study, patients with delirium had significantly increased levels of CRP and ESR. Evaluation of ESR and CRP showed infection or inflammation in delirium patients (8). This finding is in line with previous studies, which introduced infection as the cause of delirium. Moreover, our results indicated a significant correlation between abnormal LFT and development of delirium, similar to previous studies (36).
Kawaguchi et al. found that low hemoglobin level is associated with a higher incidence of delirium (37), probably due to inadequate oxygen supply; this finding is not in agreement with the results of the present study. On the other hand, our results are in line with earlier studies, which showed that delirium is correlated with mortality in the first three months after admission (38). Investigation of risk factors for delirium enables physicians to determine interventions focused on reducing the incidence of delirium in elderly patients. Private nursing at home or nursing home placement (33) within 1 - 3 months, in addition to the assessment of delirium risk factors, is important for the optimal care of elderly patients after hospitalization.
This study has some limitations. First, there is no information on some risk factors, such as poor social support and impaired functional status after hospitalization. Second, re-hospitalization was not evaluated in this study. On the other hand, the significance of this study is that it was conducted in a general hospital with a system in which physiatrists participate in the management of patients when needed. Another important strength of this study is delirium monitoring of patients for three months, as delirium tends to fluctuate over time. Accordingly, NCS was completed three times in the hospital setting on the consulting day, three days after the consulting day, and on the day of discharge.
Our sample was followed-up for one and three months. Generally, follow-up of patients is important as it has multiple implications for nurses in practice, education, and research.
Further prospective research can better identify the success of interventions in reducing specific causes of mortality. Also, future research may indicate the effectiveness of interventions in reducing the development of delirium in hospitals. Risk factors associated with delirium are potentially modifiable by changing the number of medications and procedures. Continued research is needed to evaluate the best available approaches for delirium management.
5.1. Conclusions
In conclusion, delirium is a serious and common complication in people over 60 years who are admitted to hospitals. In this study, we identified delirium risk factors in older patients who were admitted to the hospital for different reasons. Identification of these risk factors can provide more suitable management approaches for delirium. Additionally, continuous guidance and education can encourage nurses in hospitals to consider cognitive evaluation and sensitivity to risk factors of delirium. Private nursing care at home or nursing home placement, besides the assessment of delirium risk factors, is important for optimal care of elderly patients after hospitalization.