1. Background
Despite huge advances in science, technology, and medical equipment, numerous concerns grow over healthcare workers (HCWs) since they are exposed to a wide range of chemical, biological, mechanical, physical, and psychological hazards due to the nature of their work. The presence of different hazards in hospitals is repeatedly mentioned in many studies; for example, electric shock due to increased use of diagnostic and therapeutic equipment such as electrocardiogram and electric suction devices (1), chemical hazards observed after being exposed to disinfectants, cleaning compounds, drugs, mercury, and anesthetic gases (2, 3), fire and explosion caused by increasing fire risks with the development of vertical buildings (4), as well as the use of pressure devices and heaters (5, 6), slips and falls due to unsafe surfaces (7), exposure to radiation following the use of radiant and radioactive materials for diagnostic and therapeutic purposes (7), hospital waste produced by microorganisms (8, 9), injury with needles and sharp objects accompanied by contamination with pathogens including hepatitis B, C, and human immunodeficiency viruses (10), respiratory disorders and lung function impairments due to exposure to chemical and bioaerosols (11), musculoskeletal disorders as one of the most common causes of absenteeism and injury among HCWs particularly females (12, 13), and psychological risks such as job stress (14), shiftwork (15), and violence in the workplace (16).
Since health-related hazards and challenges in hospitals are considered as unique risks, HCWs and nurses are at risk of experiencing different kinds of health problems as well as some accidents and natural disasters. In 2013, 19% of all recorded occupational diseases in the United States occurred among HCWs (3). In 2011, 253,700 work-related diseases and injuries were reported in hospitals in the United States, which was approximately twice higher than the rate for industrial workers (17). In a study performed on health risks in hospitals, 50% of the participants reported experiences with a work-related health hazard. The highest rate of complaints (39.5%) was attributed to biological hazards such as needle sticks, cuts, direct contacts with bio-contaminants, and airborne or infectious pathogens (18). Among non-biological hazards, 21.5% of HCWs reported job stress. Slips, trips, falls, and fractures had similarly a rate of 21%, musculoskeletal injuries constituted 10.5% of complaints, and others such as physical hazards or burns were 10% (6). Tabatabee et al., analyzed occupational hazards among HCWs in a teaching hospital in Qazvin, Iran, and reported that the majority of work-related hazards leading to absenteeism were due to slips, trips, and falls. In their study, the prevalence of traumatic back pain caused by handling was reported at a high rate (19).
It is noteworthy that poor occupational safety and health (OSH) not only affects health and safety among HCWs, but it may also influence their efficiency and productivity in terms of providing health services to patients. Thus, establishing an OSH management system (OSHMS) is assumed as the most effective strategy to reduce incidents and likely to increase profitability (20). An OSHMS can accordingly aid organizations to consistently identify, assess, and control their OHS risks to better comply with rules and regulations and improve performance (21, 22).
All OSHMSs require hazard identification and risk assessment (HIRA) as a primary essential measure in controlling safety and health risks that also allow organizations to identify, assess, and prioritize their risks. Besides, it involves a critical appraisal of all activities (i e, routine and non-routine operations) in taking account of hazards to workers, patients, and other people affected by organizations’ activities (22). There is even a wide range of HIRA techniques and indices; a very limited number of them, such as hospital safety index (HIS) are specific to hospital and healthcare services (23), but not for OHS purposes.
2. Objectives
The current study aimed at developing and validating a particular index for OSH to improve the safety of healthcare systems more effectively.
3. Methods
The current cross-sectional study was conducted in two phases.
3.1. Development and Validation of the Hospital OSH Risk Assessment Index
3.1.1. Preparing Hazard Identification Checklists
In order to develop and validate an index applicable to healthcare centers, firstly, effective items on these fields had to be identified and categorized. In the present study, the research team referred to the selected hospitals at certain times. Prior to visiting the given hospitals, coordination was made with hospital authorities, and necessary permissions were also obtained. A package of the HAZID checklists were then provided considering five occupational hazard categories including physical (electrical, fire/explosion, fall/slip, and radiation), chemical (exposure to acids and bases, alcohol, ether, ester, formaldehyde, and detergents), biological (needle stick and sharp objects, hospital waste, and bloodborne pathogens), ergonomic (musculoskeletal disorders and environmental parameters), and psychological hazards (violence in the workplace, shiftwork, and job stress). The items included in the checklists were extracted from the national OSH regulations and standards for each category as well as national guidelines. A total of 10 OSH experts with at least five years of experience in healthcare settings were then interviewed and asked to study the items and provide comments on them. Afterward, the comments were applied to the considered items. Table 1 indicates a summary of the items selected for each hazard category.
| Hazard Category | Main Investigated Item |
|---|---|
| Electrical shock | HCW safety training, use of personal protective equipment, periodic inspections of electrical installations, electrical equipment earth system, earth wire resistance measurement, electrical equipment locking and tagging during maintenance, use of insulation and antistatic flooring, use of capacity electrical sockets, electrical equipment protective switches, separate energized and de-energized wires |
| Fire and explosion | Safety maintenance principles of chemicals, separation of pressurized gas cylinders, periodic inspections of compressed gas cylinder fitting, labeling and warning the danger of ignition of flammable materials, use of non-sparking equipment in the vicinity of flammable gases, rapid clearance of spilled fuel on floors, developing emergency response plans, training, firefighting team, fire resistance of building materials, fire detection and control equipment, emergency exit signs, testing and annual recharge devices of fire safety, safe disposal of flammable materials |
| Fall and slip | Frictional resistance of foam materials, presence of warning signs, standard slopes, fast drying of wet surfaces, slip-resistant HCW footwear, adequate lighting for hallways, stairs and landing of stairs, periodic inspection of elevators, elevators equipped with bumpers and automatic braking systems |
| Radiation | Radiation hazard warning signs, use of radiation HCW protection equipment, surface contamination tests, radiation room safety, training of HCW involved in radiation, safety principles of radioactive waste |
| Chemical | General and local ventilation, use of personal protective equipment, training of HCWs working with chemicals, warning signs of contact with chemicals, maintenance and use of chemical safety principles, the existence of emergency shower and eyewash in high-risk places |
| Biological | Training HCWs in safe injection, principles of waste separation, checking size and number of safety boxes, HCW vaccination against infectious diseases, warning signs, use of personal protective equipment, HCW periodic examinations, tests for assessment of biological system sterilization, separation of clean and dirty parts of central sterilization room, the existence of a quarantine room for patients |
| Ergonomic | Ambient temperature conditions, adequate lighting, use of measures to reduce glare, implementation of measures to reduce ambient noise, the height of desks, appropriate desk space, ergonomic chairs, body postures, ergonomics training, use of mechanical devices for manual handling |
| Psychological | Stress reduction programs, clarified duties of staff, friendly supervisor-employee relationships, job promotion, encouragement and appreciation system, presence of kindergarten, amenities, floating shifts, diet programs for shift workers, scheduled work and rest HCWs, trained security forces, the existence of glass barriers and protective equipment such as closed-circuit television, training on how to deal with violence in the workplace |
3.1.2. Validity and Reliability of HAZID Checklists
To assess the face validity of the HAZID checklists, the first version of the prepared checklists were examined by OSH experts in terms of relevance, clarity, and simplicity. Moreover, they were asked to leave comments on the items and also add any other items they thought were required for the HAZID checklists in hospital settings.
The content validity ratio (CVR) was also calculated for each item of the checklists, according to Lawshe’s formula (24, 25) (Equation 1). In this respect, a panel of experts was created, and they were asked to rate each item based on a three-point Likert scale as 0 (not essential), 1 (useful, but not essential), and 2 (essential).
CVR: Content validity ratio (to analyze the validity of items)
ne: Number of panelists essential to each item of the HAZID checklists
N: Total number of panelists
According to Lawshe (24), a CVR of 0.62 is required to retain the item when there are 10 panelists. Content validity index (CVI) of each HAZID checklist was correspondingly computed using Equation 2, and their acceptability was assessed based on the following criteria: acceptable (scores > 0.79), requiring modification (scores 0.70 - 0.79), and unacceptable (26).
Inter-rater reliability of the given checklists was further tested via the intra-class correlation coefficient (ICC). For this purpose, five public and private hospitals were rated by eight OSH experts. A coefficient value of ≥ 0.7 was considered as acceptable inter-rater reliability (27). Cronbach’s alpha coefficient was used to assess the internal consistency of the checklists for hazard categories, which was ≤ 0.7, indicating good internal consistency (28).
3.1.3. Determining Importance Coefficient of Items
To weigh the importance of each item in the HAZID checklists, a coefficient scored 1 (minimum importance) to 3 (maximum importance) was allocated to each item. This coefficient was determined based on the judgments of a panel of experts consisting of 10 OSH experts in hospitals.
To determine the IC, the mean score of panelists’ scores for each item was interpreted as 1 - 1.5 (IC = 1), 1.6 - 2.5 (IC = 2), and 2.6 - 3 (IC = 3).
3.1.4. Weighing Hazard Categories Using Analytical Hierarchy Process
In the current study, the weight of different hazards in hospital settings was calculated through AHP. This method was developed by Saaty (29) to support multi-criteria decisions when the problem could be broken down into its constitutive elements through which decision-making would be possible based on paired comparisons, and various options could also be prioritized based on specified criteria (30). Both of the two phases of the AHP technique, including hierarchy tree definition and numerical evaluation of tree, were completed in the current study. The hierarchy tree definition, therefore, started from the determination of the proposed goal, and then the criteria (i e, severity, and likelihood of hazards) were defined using the expert’s experience. For this purpose, all five categories and four subcategories of hospital hazards were included in paired comparison questionnaires and submitted to the 10 OSH experts experienced in hospital settings. They were subsequently asked to weigh the severity and probability of each pair of hazards using the Saaty scale. Therefore, the alternatives (i e, different hazard categories) were prioritized in the evaluation phase of the AHP technique based on paired comparisons (31, 32).
This process was performed to obtain values that weigh criteria and define a ranking for alternatives. The evaluation was also bottom-up in a way that the decision-making process started by comparing the alternatives with the criteria of the last level. The evaluation continued up to the criteria of the 1st level, which were then compared with the goal.
The scheme proposed by Saaty (i e, equal 1, barely better 2, weakly better 3, moderately better 4, definitely better 5, strongly better 6, very strongly better 7, critically better 8, absolutely better 9) was further used to translate linguistic judgments into numbers (33, 34). Finally, the geometric mean of the responses was calculated, and the weight (i e, risk) of each hazard was provided using the Super Decisions software.
3.1.5. Completion of Checklists and Scoring
In this phase, all the 36 teaching hospitals affiliated to Shiraz University of Medical Sciences were evaluated by five trained observers using the developed index. For this purpose, 10 random workstations were considered to be observed in each hospital. Each item of the HAZID checklists was comprised of two columns in front, including safe and unsafe. Each item was also scored based on the number of checkmarks in the safe column as follows: 2 (complete safety) for more than seven checkmarks, 1 (incomplete safety) for 4 - 7 checkmarks, and 0 (unsafe) for 1 - 3 checkmarks in the safe column in front of each item. The score for each checklist (i e, hazard category/subcategory) was calculated using Equation 3 (35):
N: Score of each checklist (i e, hazard category/subcategory)
ni: IC of the item
xi: Calculated score for each item
Finally, the HOSHRA index was computed using Equation 4:
Nc: Calculated score for physical, chemical, biological, ergonomic, and psychological hazard categories
Wc: Inter-category AHP weighted coefficient
For the physical hazard category consisting of four subcategories, first, the final score was calculated via Equation 5:
NPHH: Physical hazard final score
NPsc: Calculated score for each subcategory of the physical hazard including electrical, fire and explosion, fall and slip, and radiation hazards
WPsc: Intra-category AHP weighted coefficient
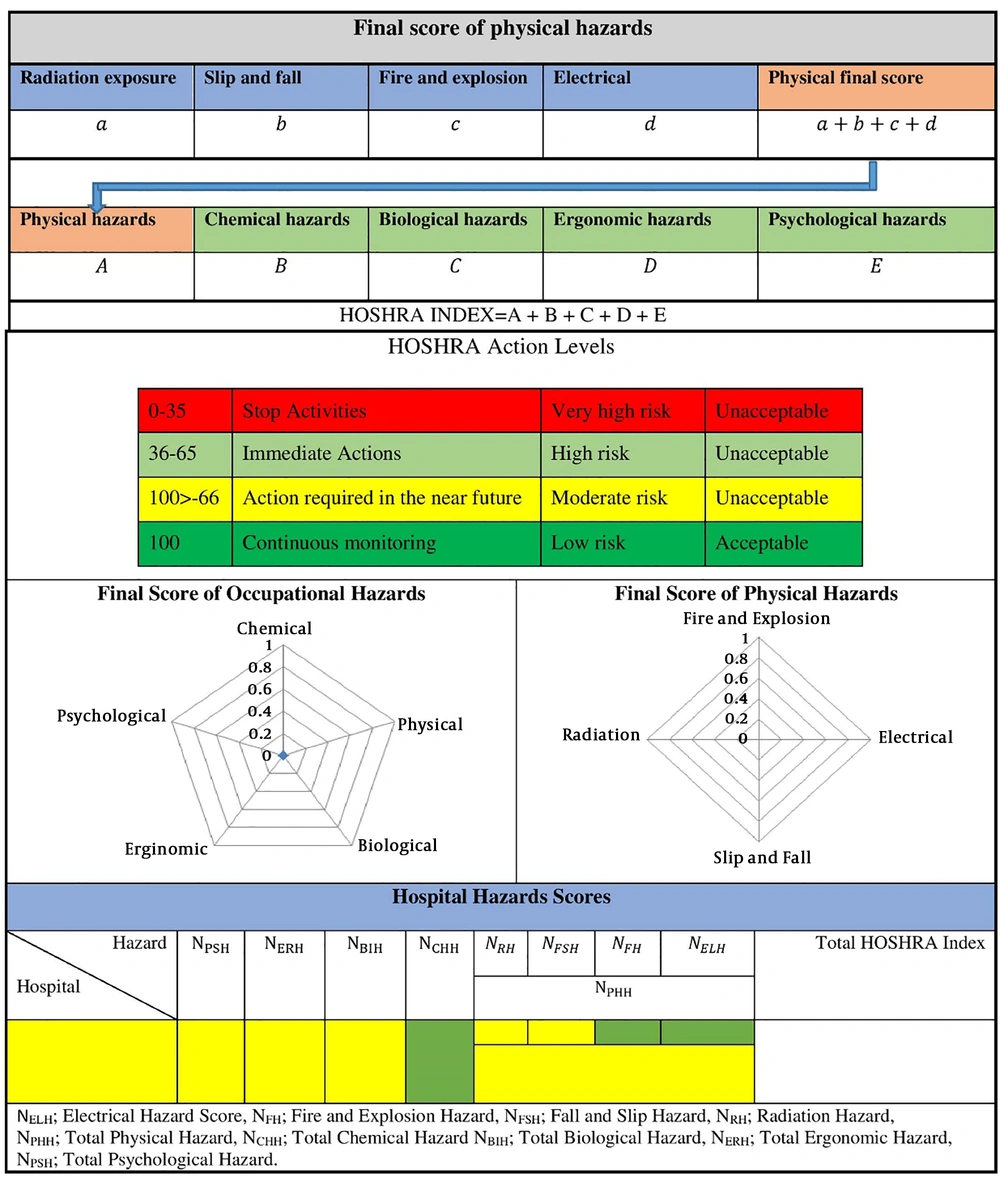
The HOSHRA index scores were then categorized into four levels as very high risk (the HOSHRA index < 36), high risk (36 ≤ the HOSHRA index ≤ 65), moderate risk (66 ≤ the HOSHRA index ≤ 95), and low risk (96 ≤ the HOSHRA index ≤ 100) (35). The summary of the HOSHRA index is shown in Figure 1.
4. Results
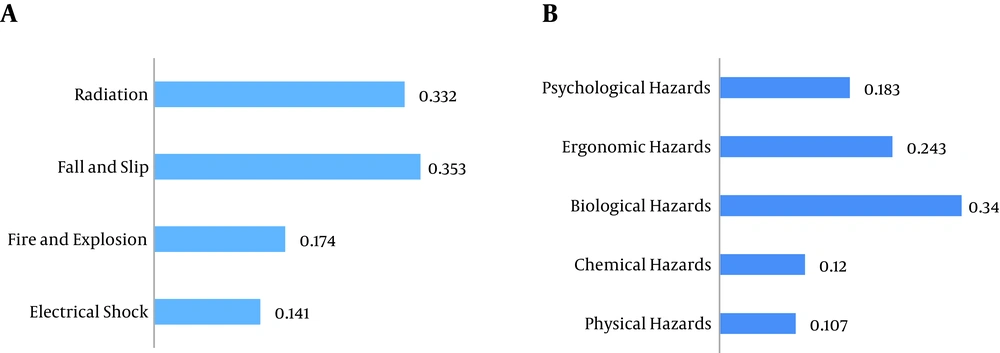
The calculated CVI, ICC, and Cronbach’s alpha coefficient indicated an acceptable content validity, inter-rater reliability, and internal consistency for hazard categories (Table 2). Figure 2 illustrates the intra-category AHP weighted coefficient for physical hazard subcategories and hazard categories. As shown, based on the panelists’ point of view, fall and slip had the highest weighted coefficient, followed by radiation hazard among the physical hazards (Figure 2A). Furthermore, among the main hazard categories, the highest values of the AHP weighted coefficient were assigned to biological hazards (Figure 2B).
| Hazard Category | Number of Items | Cronbach’s Alpha Coefficient | CVI | ICC |
|---|---|---|---|---|
| Physical | ||||
| Electrical shock | 17 | 0.83 | 0.91 | 0.97 |
| Fire and explosion | 27 | 0.74 | 0.73 | 0.99 |
| Fall and slip | 21 | 0.89 | 0.93 | 0.97 |
| Radiation | 17 | 0.76 | 0.76 | 0.95 |
| Chemical | 20 | 0.71 | 0.84 | 0.97 |
| Biological | 29 | 0.73 | 0.92 | 0.99 |
| Ergonomic | 26 | 0.81 | 0.89 | 0.99 |
| Psychological | 26 | 0.72 | 0.83 | 0.98 |
| Total (HOSHRA) | 183 | 0.77 | 0.85 | 0.99 |
Table 3 represents the mean scores of the HOSHRA index for hazard categories in the studied hospitals. As reported, ergonomic hazards had the lowest value in the HOSHRA index, indicating the highest level of OSH risk among the hazard categories. According to the HOSHRA action levels, the level of OSH risk for ergonomic hazards was high, but it was moderate for physical, chemical, ergonomic, and psychological ones. In the physical hazard subcategories, the risk of electrical shock along with fire and explosion hazards was high, but it was moderate for fall and slip, and radiation.
| Category | The HOSHRA Index | ||
|---|---|---|---|
| Mean ± SD | Maximum | Minimum | |
| Physical hazards | |||
| Electrical shock | 60.6 ± 11.16 | 75 | 40 |
| Fire and explosion | 63.2 ± 10.04 | 80 | 43 |
| Fall and slip | 77.9 ± 6.88 | 88 | 71 |
| Radiation | 79.5 ± 6.85 | 90 | 70 |
| Total | 74.39 ± 5.53 | 80.4 | 66.5 |
| Chemical hazards | 69.87 ± 6.07 | 80 | 62.5 |
| Biological hazards | 75.48 ± 5.66 | 85.8 | 68.3 |
| Ergonomic hazards | 65.86 ± 8.28 | 78.6 | 51.7 |
| Psychological hazards | 70.81 ± 10.97 | 87.2 | 54.5 |
5. Discussion
The current study mainly aimed at assessing OSH risks among hospitals in Shiraz, Iran. To this end, an observation-based method, named the HOSHRA index, was developed. The index consisted of a package of eight HAZID checklists in five categories of physical, chemical, biological, ergonomic, and psychological hazards. The developed HOSHRA index showed acceptable validity and reliability. The mean score of the HOSHRA index among the selected hospitals was 71.53 ± 5.93, indicating that the risk of OSH was at a moderate level. The highest and the lowest risk levels, according to the developed HOSHRA index, were 65.86 ± 8.28 and 75.48 ± 5.66 for ergonomic and biological hazards, respectively.
The AHP results also revealed that based on the panelists’ point of view, the maximum and minimum weighted coefficients for different hazard categories in hospitals belonged to biological and physical hazards, respectively. It is noteworthy that the most important items in the biological hazard checklist contributing to these findings were mainly related to the use of automatic injection syringes, access to biological hazard warning signs, regular monitor of biological hoods, and use of a sterile gauze when breaking ampule headings. In a study by Melisa et al., on hazards in healthcare sectors, the most important reason to be at risk of biological hazards, such as bloodborne pathogens, was performing the tasks involving sharp devices and their unsafe disposal (2). Moreover, the World Health Organization emphasizes guidelines developed to protect HCWs against biological hazards, including universal or standard precautions that warrant a system of work practices and behaviors minimizing biological exposures (36).
Interestingly, the AHP weight for ergonomic and psychological hazards was higher than that of chemical and physical ones. The items of the checklists contributing to such results were mainly associated with the lack of access to adjustable tables, being involved in static tasks such as long-term standing jobs, and distractive noises for ergonomic hazards. Lack of kindergartens, limited break time, and shift work were also considered as psychological hazards. In a study on occupational hazards in the Thai healthcare sector, it was similarly revealed that after biological hazards, musculoskeletal and psychological problems were the most prevalent problems among HCWs. Other factors, such as long shift work and lack of required HCWs were also taken into account as the reasons for such findings (3).
The highest value of the AHP weighted coefficient among the main hazard categories belonged to biological ones (w = 0.34), denoting that the experts believed that biological hazards among hazard categories were more likely to make occupational problems for HCWs. In a study performed in Greece, both HCWs and experts assigned high and moderate risks to biological hazards (37).
Among hazard categories in the HOSHRA index, the minimum value of the HOSHRA index (i e, the highest level of OSH risk) belonged to ergonomic hazards (65.86 ± 8.28), suggesting a high level of OSH risk in the studied hospitals. The main reasons regarding such findings were related to a lack of adequate knowledge among HCWs of work postures and patient handling and mobility. Similarly, the perception of occupational hazards in Greek HCWs was examined, and a risk assessment matrix was developed after preparing general questionnaires and completing them by experts and HCWs in hospitals, through which the perception of experts and personnel in different hazard categories were compared. The perceptions were found different when assessing management and ergonomic categories, as the experts believed that the risk of these categories was high, but HCWs perceived them as a moderate risk. Such discrepancies in concepts happen as experts might have more information about appropriate postures and patient handling and mobility compared with general HCWs (37).
In the category of physical hazards, the maximum AHP weighted coefficient was associated with fall and slip. However, the risk of fall and slip in the selected hospitals were categorized at a high level. These findings were in accordance with those of the studies by Bell et al., and Raeissi et al., in which the percentage of HCWs encountering falls and slips were one of the highest ones in a selected Iranian hospital (38). Moreover, according to the United States Bureau of Labor Statistics in 2007, the incidence of slipping and falling injuries in hospitals was 35 per 10,000 HCWs (39). These findings indicated the necessity of a preventative program to manage the fall and slip risks in healthcare centers (2).
The risk of the electrical hazard was categorized as a high-level one. In other words, electrical hazard had the highest value in the HOSHRA index in all categories and subcategories. The main reasons for the items in the checklist were related to lack of building wiring map, absence of protective switches, and lack of using protective equipment against electrical hazards by HCWs involved in this hazard category.
In the studied hospitals, the lowest OSH risk level in the physical subcategory belonged to the radiation hazard since there was a strict rule by law enforcement agencies, including the Atomic Energy Agency concerning radiation protection. Furthermore, health physicists could oversee the proper observance of radiation protection rules and regulations in hospitals. HCWs had a good risk perception about radiation, and they took it seriously. In a study performed in a hospital in Iran, random exposure to radiation was also reported by nearly half of HCWs (38). Greek HCWs in a study by Tziaferi et al., ranked radiation hazard as a high-risk agent in the studied hospitals, although the experts believed that it could be grouped in the moderate risk category (37).
Totally, according to the mean score of the HOSHRA index in the selected hospitals, all of these hospitals were categorized at a moderate level. One of the reasons for a low standard deviation (SD) in the current study was probably because all the studied hospitals were affiliated to the same university, and they followed a similar OSH policy. In addition, the developed index was applied only in 36 teaching hospitals in a cross-sectional study. On the other hand, there was no significant correlation between the HOSHRA index and occupational injuries and diseases, since not all the required data were documented appropriately in the studied hospitals and the number of hospitals was inadequate for this purpose. Therefore, more longitudinal studies with larger sample sizes in various periods should be included to find out whether the developed index would be correlated in all subcategories with data on accidents and occupational diseases.
5.1. Conclusion
The developed observation-based method showed an acceptable content validity and reliability for OSH risk assessment of hospitals. The HOSHRA index could also be applied to hospitals as an applicable measure to improve their OSH. In general, the risk of OSH among the studied hospitals was evaluated as moderate.