1. Background
Cytomegalovirus (CMV) belongs to the family of Herpesviridae and the subfamily of Betaherpesvirinae. Infection with CMV is highly frequent during pregnancy in human beings, which leads to preterm birth in 34% of the cases. The incidence of CMV seropositivity ranges from 40% to 100% worldwide. Approximately 50% of the population in the developed countries is seropositive for CMV by the age of 50. The primary maternal CMV infection during pregnancy carries a 40% risk to transmit the infection to a fetus, but congenital CMV infection is less likely due to its recurrence (1%) (1).
The prevalence of the primary infection with CMV in Iranian pregnant women and the risk of congenital CMV infection in infants is unknown (2). Congenital infections may occur after primary or frequent infections in pregnant women and are the main cause of hearing impairment, vision impairment, mental retardation, and seizure in children. After the primary infection, the virus is spread from the body through different ways in the following weeks or even years and then remains latent. Repeated episodes of infection may be a sign of the latent virus reactivation or reinfection with a different type of CMV with different antigenicity. Apart from the infection phase, most infection episodes of CMV are asymptomatic in a host with a normal immune system and usually do not cause any serious problem. However, maternal CMV infection during pregnancy can pose severe and permanent problems for the fetus (3, 4).
Since maternal CMV infection during pregnancy poses severe consequences for the fetus, screening for this virus during pregnancy could be very helpful as it provides a way to search for any related infection in the fetus and a case of positive results, the birth of a child with physical and mental defects can be prevented utilizing selective abortion. Laboratory tests are the best and only way to diagnose the disease. Despite its advantages, amniocentesis is an invasive procedure that increases the risk of abortion; therefore, serological and molecular methods are of great importance in the timely diagnosis of CMV infection (5, 6).
2. Objectives
The present study aimed at preventing and controlling CMV infection in pregnant women by determining and comparing their frequency in some parts of Golestan Province, Northern Iran, using serological and molecular methods and comparing the results.
3. Methods
3.1. Study Population
In the current cross-sectional study conducted from October 2017 to August 2018, blood samples were collected from 315 pregnant women (age range = 17 - 44 years, mean age = 23 ± 8.2) admitted to eight laboratories in Central and Western parts of Golestan Province after obtaining written consent. Moreover, all the personal data such as name and address of the patients kept confidential, and samples were identified merely based on the given codes. The women were in the first six months of pregnancy in which the risk of abortion as a result of infection is very high. The variables investigated in the study included age, ethnicity, occupational status, the month of pregnancy, smoking habits, and history of abortion. Patients’ information was recorded in a questionnaire, and their blood samples were kept based on assigned codes until testing.
3.2. Determination of CMV Infection
The screening test was conducted using the ELISA (the enzyme-linked immunosorbent assay) technique to detect CMV-IgG, followed by CMV-IgM and CMV-IgG avidity tests to determine the seropositivity prevalence of CMV. In the serologic study, the ELISA kits of anti-CMV IgG and anti-CMV IgM (Euroimmun Company; Germany) were used, and the results were interpreted according to the manufacturer’s instructions. Then, molecular tests using the PCR technique were also carried out on serum samples to gain more precise and reliable results.
3.3. Evaluation of the Quality and Quantity of the Extracted DNAs
A commercial kit (ROCHE Co., Switzerland) was used to extract the genomic DNA. To determine the DNA purity, the 260/280 nm absorbance ratio in the sample was used; values ≥ 1.8 were considered as the standard pure DNA. Lower ratios indicated protein impurity in the samples.
3.4. PCR Assay
The molecular analysis was performed using the PCR technique. According to the instructions for ROCHE kit (CMV Gene Proof), serum samples were prepared to extract nucleic acid, and the 254-base-pair fragments of the UL55 gene were proliferated after identification by the following specific primers (7):
(R) CGGCAATCGGTTTGTTGTAAA and (F) GGTCTTCAAGGAACTCAGCAAGA.
The PCR amplification was carried out in a 25-µL solution containing 1 µL of the DNA sample, 1 µL of each forward and reverse primers, 0.5 µL of dNTP, 2.5 µL of PCR buffer, 1.5 µL of magnesium chloride, 0.2 µL of Taq polymerase enzyme (5 U/µL), and 18.05 µL of distilled water. Initial denaturation was done at 94°C for 90 seconds, followed by 40 cycles of final denaturation at 94°C for 50 seconds. The annealing phase was carried out at 64°C for 50 seconds, and the extension was performed at 72°C for 50 seconds. The final extension was also performed at 72°C for 10 minutes. The PCR product was then run on a 1.5% agarose gel and stained in ethidium bromide for visualization under ultraviolet light. The standard kit was used as the positive control and distilled water as a negative control.
3.5. Data Analysis
The Kolmogorov-Smirnov test was employed to ensure the normality of data distribution, and then all the data were entered into the SPSS software version 23.0; chi-squared test was applied to evaluate the qualitative data.
4. Results
4.1. Demographic Characteristics
Typically, 25% of women with primary CMV infection were negative for IgM, and the key indicator was a four-fold increase in anti-CMV IgG serum titer after 2 - 4 weeks. Avidity tests were used to complete ELISA testing. Avidity index (AI) below 30% indicates infection in the last three months and AI 30% - 50% recent infection. Analysis of serological findings showed that the IgG- and IgM-positive cases with low IgG avidity were considered to have a primary infection and the IgG- and IgM-positive cases with high IgG avidity were considered to have a secondary infection. Merely IgG-positive cases were considered to have a history of infection (8). The results of the serological test showed that 201 pregnant women were only IgG-positive, of which 20.9% were IgG- and IgM-positive with low IgG avidity and 6.5% were IgG- and IgM-positive with high IgG avidity. However, only 21 women were positive for CMV after molecular analyses, of which 13 (62%) had a history of abortion (Table 1).
| Antibody Titer | Fars Ethnicity | Turkmen Ethnicity | P Value |
|---|---|---|---|
| Primary infection | 27 (64.3) | 15 (35.7) | 0.01 |
| Secondary infection | 2 (15.4) | 11 (84.6) | 0.01 |
| Previous infection | 0 | 3 (100) | 0.036 |
| No infection | 85 (59.4) | 58 (40.6) | 0.04 |
aValues are expressed No. (%).
4.2. Analysis of the Results after DNA Proliferation
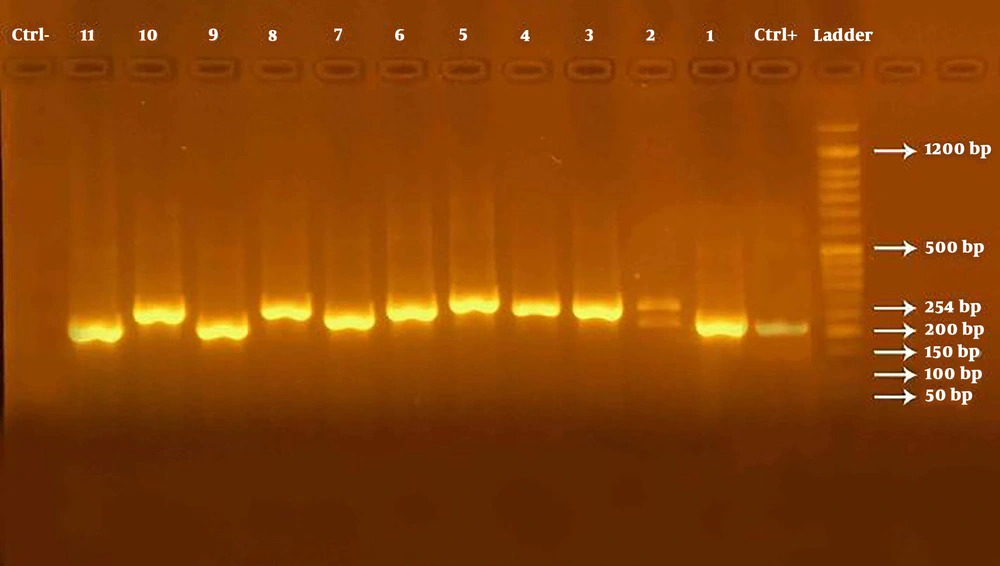
In the current study, bands visualized at 254 bp were considered positive after the electrophoresis of the PCR products for the UL55 gene (Figure 1).
The results of the molecular analysis showed that of the total 256 seropositive samples studied in terms of infection with CMV, 21 (8.2%) were positive, and 235 (91.8%) negative. Out of the studied women, 81.2% were positive for CMV-IgG and CMV-IgM, but only 8.2% had positive results in the molecular detection of CMV, out of which 61.9% had a history of abortion. However, no significant statistical relationship was found between the incidence of abortion and higher serum titers of CMV-IgG.
Analysis of the role of ethnicity in infection with CMV noted that 66.7% of positive samples belonged to Fars ethnic group. Evaluation of the relationship between ethnicity and occupational status showed that 85% of Fars and 29% of Turkmen housewives were CMV-positive. The relationship between ethnicity and age revealed that 35% of Fars and 42% of Turkmen pregnant women were older than 30. The relationship between ethnicity and the month of pregnancy indicated that 71% of Fars and 43% of Turkmen pregnant women were infected with CMV during the 4th to 6th months of pregnancy. Considering all these correlations, a significant relationship was observed only between age and infection with CMV (Table 2). Regarding the smoking habits, the variable was excluded from the final analysis as none of the subjects smoked.
| Variable | Fars Ethnicity, % | Turkmen Ethnicity, % | P Value |
|---|---|---|---|
| Age, y | 0.045a | ||
| > 30 | 65 | 58 | |
| < 30 | 35 | 42 | |
| Trimester of Pregnancy | 0.14 | ||
| First | 29 | 58 | |
| Second | 71 | 42 | |
| Occupational status | 0.07 | ||
| Housewife | 85 | 29 | |
| Employed | 15 | 71 | |
| History of abortion | 0.36 | ||
| Yes | 21 | 41 | |
| No | 79 | 59 |
aThe significant difference between the study groups was determined based on the chi-Squared test results.
5. Discussion
The present study aimed at investigating the frequency of CMV-positive cases among pregnant women in Golestan Province, Northern Iran. For this purpose, investigations were performed based on demographic characteristics using questionnaires or the remarks made by doctors. The study was conducted on 315 pregnant women admitted to hospitals in Central and Western parts of Golestan Province, and major variables including ethnicity (Fars and Turkmen), age, the month of pregnancy, and occupational status were considered for comparative purposes.
The majority of pregnant women in the current study (65%) were from Fars ethnic group (any entity other than Turkmen), and the rest were Turkmen (35%). The population of Turkmens in Golestan Province is more than 500,000; approximately ≥ 33% of the total population of the province. These statistics highly match the data gained from the current study in which the subjects were randomly selected. Besides, the frequency of the Turkmen group in the current study population was relatively similar to that of the Turkmen people in the total population of Golestan Province. Thus, the same ratio was set between Fars and Turkmen ethnic groups to more precisely evaluate the frequency of CMV infection in pregnant women of the province.
Another variable investigated in the study was the age range from 17 to 44 years. Because of the age range limitations in the study, two groups were defined, and the higher rate of pregnancy was observed in the group over 30 years. The important point concerning age in the study was the fewer number of pregnancies in some age groups, and the increased risk of pregnancy at older ages.
In a study on high-risk pregnancy and some contributing factors in pregnant women admitted to hospitals in Yasouj, Western Iran, the frequency of pregnancy was 2.1% and 5.1% at younger (below 18) and older ages, respectively, which indicates increased awareness of women about pregnancy in particular age ranges and reduced risk of pregnancy at high-risk ages (9).
Researchers reported that infection with CMV is more common in women, and the risk increases with age (10). However, most cases of infection with CMV in pregnant women (60% - 66%) occur under 30 years, and the associated risk factors depend on economic and social status (4).
In the present study, more than 40% of positive cases were older than 30 years. Less than 53% of positive cases were under the age of 30. Therefore, positive results for both age groups would be about 50%, which did not match the reports (4). Additionally, the majority of the pregnant women in the current study (76.19%) were housewives, and a few of them were employed or students.
The month of pregnancy was another variable investigated in the study groups; the results indicated that 61.9% of CMV-positive cases were in the second trimester of pregnancy (the 4th to 6th months), and the rest were in the first trimester.
According to a study, CMV infection generally poses severe complications to the fetus if it occurs at the early stages of pregnancy since infections during the first trimester disrupt organogenesis; infections during the second or third trimester also cause neurologic or developmental complications (11).
of the total 315 pregnant women under study, 81.27% had higher serum titers of IgG- and IgM-CMV, which were considered positive for this viral infection. Among the subjects who were CMV-positive based on serological findings, 34 had a history of abortion as reported by themselves or their doctors.
Screening tests are the most important clinical assessments concerning infertility treatment performed to determine any history of contact with CMV. In pregnant women suspected of an active infection, other diagnostic tests for proving an active infection, as well as amniocentesis and the PCR assay on amniotic fluid, can be helpful, especially during the 21st to 23rd weeks of pregnancy to check whether the fetus is also infected (12).
According to the findings of a study, despite its advantages, amniocentesis is an invasive procedure that increases the risk of abortion (13). The seroprevalence of CMV depends on various epidemiologic factors and usually varies from 80% to 90% (14).
A study showed that the seroprevalence of total antibodies against CMV in pregnant women was 97.3% (15), which was higher than the results of the present study (81.27%). In another study by the same authors on the frequency of CMV, the seroprevalence of total antibodies against CMV in pregnant women was reported 98% (16).
Diagnosis of a primary infection utilizing these two indicators can strongly predict the risk of infection in the fetus and abortion (2). According to the results of the present study, the risk of abortion in pregnant women with active CMV infection was 29%, which was in agreement with the results of another study reporting a 30% frequency for the congenital infection of the fetus transmitted through the pregnant mothers with active CMV infection (17).
Researchers measured serum titer of CMV-IgG in 537 pregnant women and reported the seropositivity prevalence of 77% (18), which was close to the results of the present study. They also reported that the seroprevalence of CMV-IgG gradually increases with the increase of age, which was also similar to the results of the present study.
In the current study, the frequency of CMV-positive pregnant women from Fars ethnic group (66.7%) was twice the number of Turkmen ones (33.3%). However, investigation of positive viral cases separately in each ethnic group showed that the frequency of active CMV in both populations was similar to 6.83% and 6.36% in Fars and Turkmen groups, respectively (P value < 0.5).
Given various etiologies attributed to unintentional abortion, it is believed that about 5% of the cases take place due to infection. Among the microbial factors contributing to such abortions, viruses play an important role in causing recurrent abortions due to developing chronic or recurrent infections in the reproductive system of women. Here, CMV is of paramount significance since the infection of the newborns with this virus is confirmed in 0.2% - 2.2% of the live births. The virus is also likely to be transmitted to the fetus through the mother exposed to CMV for the first time (19, 20).
5.1. Conclusions
According to the results of the current study, the frequency of CMV-IgG and CMV-IgM was high in serum samples collected from pregnant women and varied by ethnicity and age. The high prevalence of infection with CMV in Golestan Province was in line with the results obtained by other studies performed in Iran and other countries, particularly the developing countries.
The results of the present study showed that the frequency of CMV infection is increasing in Golestan Province. Yet, molecular analyses in the current study showed that seropositivity and even higher titers of CMV-IgG and CMV-IgM have no predictive values for CMV infection. Considering the importance of rapid and definitive diagnosis of the disease before the emergence of manifestations, the molecular techniques could be of great help as they are effective in the diagnosis of the infection with smaller amounts of the pathogenic genome. Therefore, adherence to hygiene principles and paying more attention to prenatal care as effective factors in prevention from CMV infection and its complications are recommended. Besides, amniocentesis and cordocentesis are invasive procedures that can lead to abortion and do not provide a definitive prognosis. Provision of facilities for molecular testing in other cities of Iran and utilizing low-risk, combination diagnostic methods are also recommended.