1. Background
Disasters impose numerous physical and psychological harms on affected populations (1). Iran has experienced about 20 earthquakes with magnitudes > 7 on the Richter scale (R) during the last 90 years (2). After disasters, the population would rush toward relief centers. Treatment of injured patients within the first 24-h would increase the chances of survival (3-6).
Disaster medical centers fall into five categories, the third of which includes emergency field hospitals (EFH), which are considered the best equipped and most comprehensive medical centers on-site. The EFHs comprise different medical wards with a variety of clinical and paraclinical facilities (7). Numerous studies have investigated the methods for providing relief services following earthquakes, as well as establishing EFHs (8-11).
On November 12th, 2017, at 21:48 local time, an earthquake with a magnitude of 7.3R was taken place in western Iran (2), which was estimated to lead around 600 - 700 deaths and over 10,000 injuries (12). One of the cities receiving a significant amount of damage was Sarpol-e-Zahab, the capital of Sarpol-e-Zahab County, located in Kermanshah Province, near the western border of Iran (Figure 1), which had 85,342 populations. Kermanshah is the largest Kurdish and the most important city in the Central West Region in Iran (13). Following this earthquake, numerous governmental and community teams were dispatched with various objectives, which Shiraz University of Medical Sciences (SUMS) medical team was one of them.
Considering the significance of the actions taken within a few days after an earthquake, it is imperative to use relative experiences to improve the crisis management in the case of next disasters; however, the sharing of such experiences has been previously overlooked in Iran.
2. Objectives
Thereby, in the present study, the experience of SUMS’s medical team was described. This type of study has a special significance, as it shares the experiences, which would help to identify the existing barriers and be more prepared for crisis management in future disasters.
3. Methods
This record-based cross-sectional study was carried out to focus on established EFH in Sarpol-e-Zahab and the actions taken by SUMS’s team (November 16th–23rd) following Kermanshah earthquake using data collected by this team.
The post-earthquake condition of the local hospital, then, the actions’ details taken by SUMS’s team, and the existing problems were described in this cross-sectional study using the data collected by SUMS’s team. Also, the visited patients in the EFH during this team stay were assessed, and the local medical staff’s satisfaction with SUMS’s team performance was analyzed in a comparison between before and after their arrival, using a data collection form, which was distributed among them on the last day of the team's stay. Convenience sampling method was used, and only individuals who were willing to fill out the forms and sign a written informed consent were included. The exclusion criterion consisted of not fully completing the questionnaire. This form contained two parts: demographics section (age, gender, occupation), and 13 before/after questions based on a 5-point Likert scale. Scores 1 and 5 indicated the lowest and highest levels, respectively. Then, the scores were added (minimum of 13 and maximum of 65) and compared.
All data, which could be analyzed statistically, were entered into SPSS version 22.0 and analyzed by descriptive and analytical tests, including Independent sample t-test, paired-sample, and chi-square tests. Two-tailed P value < 0.05 and confidence interval (CI) of 95% were considered to be statistically significant.
4. Results
The results of this study fall into 5 categories, as follows:
4.1. Post-earthquake Conditions
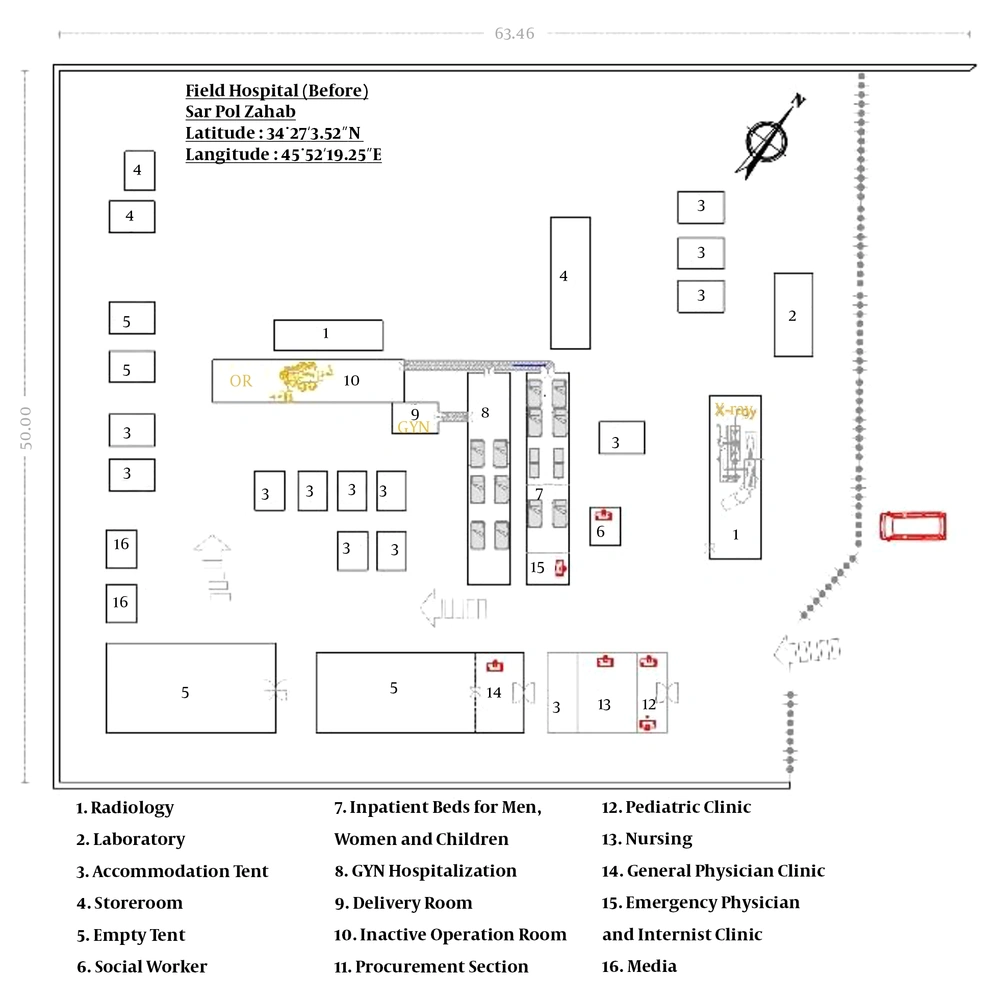
Following the earthquake, the only hospital in Sarpol-e-Zahab (Shohada hospital) with 54 beds and 180 personnel was demolished, and it had become semi-open owing to the numerous aftershocks and only could provide outpatient examinations and relief services. Upon arrival SUMS’s team, it was observed that Kurdistan University of Medical Sciences (KUMS)’ team had established an EFH in an area, located in the hospital parking lot, which included one examination room for patients’ screening, a maternity ward with one labor bed, two separate temporary inpatient wards for adults with eight beds, and four maternity beds (Figure 2). Three physicians, including one general practitioner (GP), one internist, and one emergency medicine (EM) specialist, visited the patients.
The majority of tents were supplied by the Red Crescent Society. For the aforementioned wards, as well as accommodations for the medical staff and media, Intex tents donated by KUMS were used. Staff accommodations were provided within the hospital’s designated area, in contrast to the establishment of EFHs principles. The field of the operating room with one operating table and a recovery bed were inactive. Laboratory and radiology units were built with Conex boxes. The radiology unit was only capable of taking X-rays, and patients who need CT scans were transported to Kermanshah or Eslamshahr hospitals. A 24-h pharmacy was located in the CT scan ward in the main hospital building, which was more stable due to being recently built and had not taken any damages. It is noticeable that two established EFHs by the Islamic Republic of Iran Army and Islamic Revolutionary Guard Corps (IRGC) were providing services at the hospital entrance. Also, response teams from other countries established small medical camps in different areas of the hospital in the form of non-governmental organizations.
4.2. Actions that Were Taken by SUMS’ Medical Team
The SUMS’s team improved the quality of services by maximum employing of equipment, facilities, and supplies existing in the area, communicating with governmental and military units, utilizing public donations, and establishing coherent collaboration between units working inside and outside the hospital. This team of 32 individuals (24 men and 8 women), including GPs, EM specialists, orthopedics, general surgeons, cardiologists, pediatrician, obstetricians, EM residents, internal medicine residents, radiology resident, obstetrics resident, and radiology specialist, were entered Sarpol-e-Zahab four days after the earthquake and stayed for eight days. They arrived at 1 AM and started to visit the patient at 12 PM. (Table 1).
| Hour | Measures that Were Taken |
|---|---|
| 1 AM | Arrival of the dispatched team at the quake-affected region |
| 8 AM | Commencing the establishment of the field hospital |
| 1 PM | Finishing the establishment of the field hospital |
| 2 PM | Starting to visit and treat inpatients and outpatients |
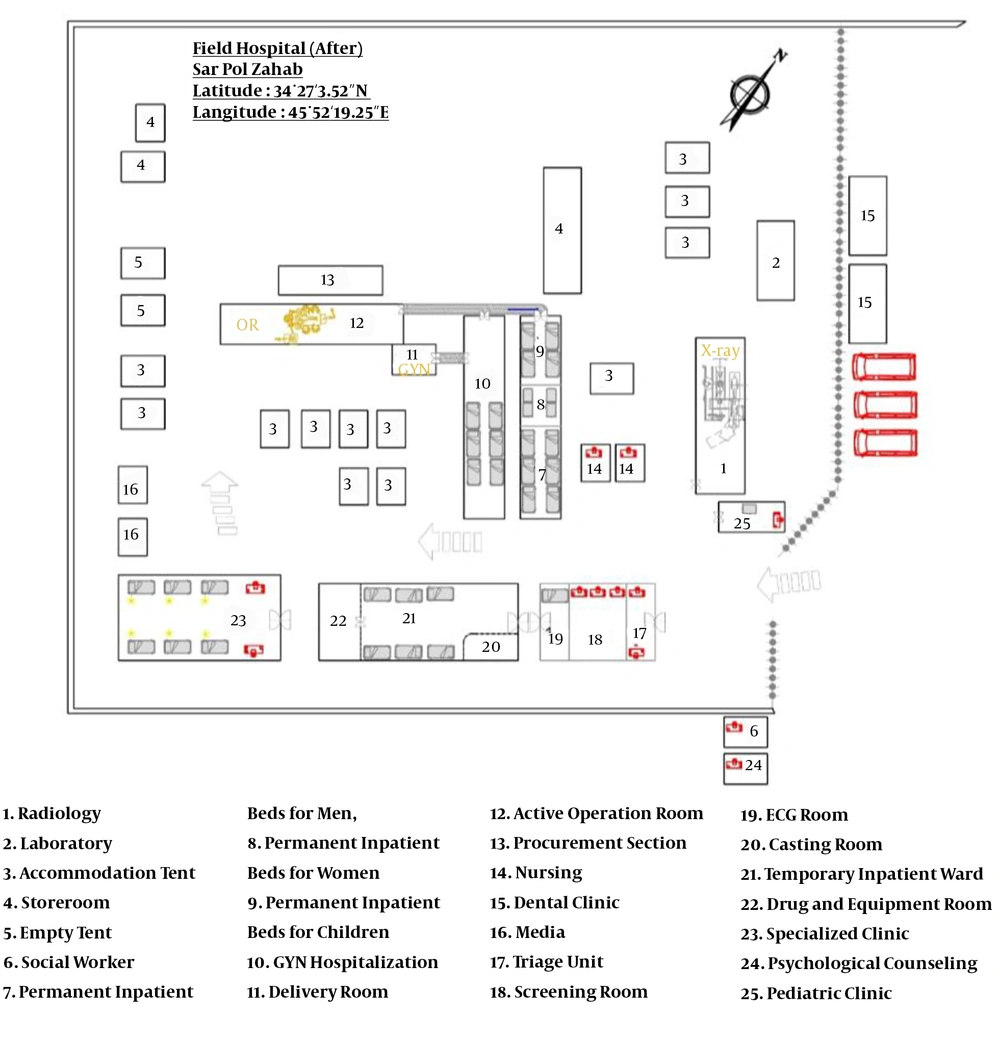
They made certain changes to the previously established EFH, in accordance with scientific principles (14). In this regard, the triage unit was moved to the hospital entrance before the screening unit. In the screening unit, an area was designated for electrocardiography along with an orthopedic casting room, with two beds for injections. Then, another area with six beds was considered for temporary inpatient. Behind this tent, a 12-h specialized clinic was established, and the specialists started visiting patients, who were also on call during closed hours. One pediatrician visited the children around the clock in a separate clinic, which was set up next to the radiology Conex box. One obstetrician was present in the clinic and obstetrics operating room for 24-h.
The previous screening room and temporary inpatient ward were turned into permanent inpatient ward with 10 - 12 beds for adults and four beds for children. No alterations were made to the maternity ward, operating room, laboratory, and radiology, but the operating room became active. Also, two Conex with dental services were provided by KUMS in the next days (Figure 3) (furthermore, see the Appendixes 1 and 2 in Supplementary File).
In order to make the aforementioned alterations, the existing equipment and supplies were used, e.g., the ultrasound machine was placed inside a Conex box, and was handled by this team. Also, this team assisted the local staff and volunteers. The EFH was fixed and temporary, as it had been decided to transfer the services to the city’s old hospital building until the construction of a new hospital. Additionally, since there was no Intensive Care Unit (ICU), critically ill patients and patients in need of long-term hospitalization were transferred to Kermanshah. Transportations were done via an interurban ambulance accompanied by one driver and one nurse. Sometimes, multiple patients would be transported by one ambulance. The decision to transport the patients were made based on the physicians’ decision and patients’ specific needs. Patients were discharged based on clinical conditions evaluation. Commands were done from Kermanshah.
4.3. Existing Problems
There was not a sufficient amount of manpower, which forced SUMS’s team to divide the working hours into three shifts (one shift work and one shift rest). Some units had to be present on-site around the clock without rest. The number of ambulances was not adequate; until the arrival of ambulances deployed from other Kermanshah’s regions.
Support was poor, especially in the first days. The dispatched team was not well-accommodated upon arrival, and the accommodation problems and the lack of basic supplies such as blankets, heating devices, and drinking water led to the lack of concentration and ordered activity. However, this problem was solved in the next days. Furthermore, there was not enough coherence between the supplies and public donation distribution and the service-providing units. The personnel’s meals were supplied from public donations throughout the city. Also, there was no access to adequate amounts of medications and equipment (Table 2). Some drugs were taken out of hospital storage, and other medication-related requests were supplied from Kermanshah.
| Medication | Diagnostic Equipment | Provisions |
|---|---|---|
| Hydralazine vials | Manometers | Pillows |
| Labetalol vials | Flashlights | Towels |
| Magnesium Sulfate vials | Pulse oximeters | Blankets |
| Heparin vials | Glucometer kits | Heating equipment |
| Ondansetron vials | Speculums | Drinking water |
| Clindamycin vials | Disposable suturing sets | |
| APOTEL vials | Tongue depressors | |
| Bisacodyl suppositories | Umbilical cord claps | |
| MOM suspensions | Fiberglass or cast along with casting tape | |
| Dimethicone pills | Cast saws | |
| Flexible bandages | ||
| Colostomy bags | ||
| Compression stockings |
Despite physical security provided by Shiraz and Alborz universities, and police force deployed from Tehran, the hospital’s equipment and supplies were stolen. Communications were carried out only via cell phone since there were no other means to communicate. Another problem was that most of the native villagers only spoke Kurdish, and due to cultural differences, it was difficult to connect with patients, therefore, the local personnel were used.
4.4. Visited Patients
During eight days, a total of 9,214 visits were done, but the data of 5,402 visits were recorded, of which 55.1% were men (P < 0.0001). The mean ± SD of age was 31.6 ± 18.65 years (range, 0 - 99), which was not different in both genders (P = 0.189) (Table 3). Chief complaints were recorded in 5,058 patients, that the most frequent were the signs of the flu and respiratory infections (38.1%), various types of trauma (20.5%), and gastrointestinal problems (11%) (Table 4).
| Day | Values | P Value | Age | P Value | 95% CI |
|---|---|---|---|---|---|
| 1st day | < 0.0001b | 0.884 | -2.65, 2.28 | ||
| Male | 505 (58.9) | 32.38 ± 17.30 | |||
| Female | 353 (41.1) | 32.56 ± 18.84 | |||
| Total | 858 (15.9) | 32.45 ± 17.94 | |||
| 2nd day | < 0.0001b | 0.491 | -3.52, 1.69 | ||
| Male | 590 (58.1) | 30.38 ± 19.41 | |||
| Female | 425 (41.9) | 31.29 ± 19.53 | |||
| Total | 1,015 (18.8) | 30.76 ± 19.45 | |||
| 3rd day | < 0.0001b | 0.189 | -1.72, 0.34 | ||
| Male | 744 (54.9) | 31.28 ± 18.65 | |||
| Female | 610 (45.1) | 31.97 ± 18.79 | |||
| Total | 1,354 (25.1) | 32.17 ± 18.18 | |||
| 4th day | < 0.0001b | 0.888 | -3.19, 2.76 | ||
| Male | 391 (55.8) | 30.68 ± 19.95 | |||
| Female | 310 (44.2) | 30.90 ± 19.76 | |||
| Total | 701 (13.0) | 0.13 | 30.78 ± 19.86 | ||
| 5th day | 0.729 | -2.3, 3.29 | |||
| Male | 341 (52.1) | 31.57 ± 18.83 | |||
| Female | 314 (47.9) | 31.07 ± 17.50 | |||
| Total | 655 (12.1) | 31.33 ± 18.20 | |||
| 6th day | 0.86 | 0.185 | -5.87, 1.14 | ||
| Male | 220 (49.7) | 28.55 ± 19.85 | |||
| Female | 223 (50.3) | 30.92 ± 17.57 | |||
| Total | 443 (8.2) | 29.75 ± 18.73 | |||
| 7th day | 0.48 | 0.513 | -2.55, 5.10 | ||
| Male | 183 (48.7) | 34.43 ± 19.00 | |||
| Female | 193 (51.3) | 33.16 ± 18.68 | |||
| Total | 376 (7.0) | 33.85 ± 18.84 | |||
| Total | < 0.0001b | 0.189 | -1.72, 0.339 | ||
| Male | 2,974 (55.1) | 31.28 ± 18.65 | |||
| Female | 2,428 (44.9) | 31.97 ± 18.79 | |||
| Total | 5,402 | 31.6 ± 18.71 |
Abbreviation: CI, confidence interval.
aValues are expressed as mean ± SD or No. (%).
bStatistically significant
| Chief Complains | Values |
|---|---|
| Flu and respiratory infections | 1,929 (38.1) |
| Various types of trauma | 1,038 (20.5) |
| Gastrointestinal problems | 556 (11.0) |
| Chronic diseases (diabetes, cardiovascular diseases, asthma, COPD, hyperlipidemia, hypoglycemia, etc.) | 291 (5.8) |
| Drug request | 289 (5.7) |
| All types of headache | 178 (3.5) |
| Neurological problems | 134 (2.7) |
| Radiography request | 134 (2.6) |
| Hypertension or hypotension | 115 (2.3) |
| Kidney system problems | 94 (1.9) |
| Bite | 86 (1.7) |
| Skin problems | 63 (1.2) |
| Musculoskeletal pains | 61 (1.2) |
| Drug, poisoning, suicide | 51 (1.0) |
| Genitourinary problems | 23 (0.5) |
| ENT and eye problems | 16 (0.3) |
| Others | 840 (16.6) |
| Total | 5,058 (100) |
aValues are expressed as No. (%).
4.5. Local staff’s Satisfaction
Satisfaction forms were distributed among 45 local staff (100% return rate), but 41 individuals (91.1%) had responded to over 90% of the questions. The mean ± SD of age was 32.03 (7.61) years [33.55 ± 8.3 in men, and 28.75 ± 5.75 in women (P = 0.064, 95%CI: -0.292 - 9.89)], and most of them were men (63.6%, P = 0.014), and nurses (68.4%). Results revealed that the local staff was more satisfied with the services provided by SUMS’s team (P < 0.0001) (Table 5).
| Items | Before | After | P Value |
|---|---|---|---|
| Level of satisfaction with physical arrangement of parts | 2.83 ± 1.40 | 3.85 ± 0.96 | < 0.0001b, c |
| Level of satisfaction with the professional performance of emergency medical services | 3.22 ± 1.26 | 4.22 ± 0.73 | |
| Level of satisfaction with the management of emergency medical services | 3.0 ± 1.38 | 4.1 ± 1.09 | |
| Level of satisfaction with the professional performance of internal medical services | 3.20 ± 1.29 | 4.07 ± 1.01 | |
| Level of satisfaction with the professional performance of cardiology services | 3.20 ± 1.31 | 3.98 ± 1.21 | |
| Level of satisfaction with the professional performance of surgical services | 3.22 ± 1.29 | 4.24 ± 0.70 | |
| Level of satisfaction with the professional performance of orthopedic services | 2.73 ± 1.5 | 3.98 ± 1.06 | |
| Level of satisfaction with the professional performance of maternity services | 3.32 ± 1.13 | 4.0 ± 1.0 | |
| Level of satisfaction with the professional performance of pediatric services | 3.05 ± 1.45 | 3.88 ± 1.29 | |
| Level of satisfaction with the professional performance of radiology services | 3.0 ± 1.38 | 3.73 ± 1.32 | |
| Level of satisfaction with the professional performance of general practitioners | 3.71 ± 1.31 | 4.0 ± 1.20 | |
| Level of satisfaction with the professional performance of radiology experts | 3.59 ± 1.36 | 4.0 ± 1.07 | |
| Total satisfaction level | 30.05 ± 12.34 | 48.05 ± 7.84 |
Abbreviation: SD, standard deviation.
aValues are expressed as mean ± SD.
b95% CI: -13.61, -6.39.
cStatistically significant.
5. Discussion
A hospital should have six vital components in the management of potential injury-creating events: physical plant, personnel, equipment and supplies, communication, transportation, and supervisory managerial support (15). EFH refers to a comprehensive hospital with different clinical, clerical, administrative, and maintenance departments in which emergency procedures, urgent care services, and surgeries are carried out. The clinical section consisted of a triage unit, emergency room, inpatient and maternity wards, an operating room, a specialized clinic, and staff accommodations (14). Before SUMS’s team arrival, these sections did not fully exist. After the rearrangement of EFH and more help provided by SUMS’s team, it was found that the local staff was more satisfied. Also, in EFH’s establishment, the distances covered by service providers and patients should be in a way that would minimize the motion (16), which was taken into account in Sarpol-e-Zahab’s EFH.
During the Iran-Iraq war, 29 EFHs were established, and all of them were fixed. The first operating rooms were established by placing a number of containers next to each other (16). Sarpol-e-Zahab’s EFH was fixed but temporary, as it had been decided to transfer the services to the city’s old hospital building until the construction of a new hospital.
In choosing EFH’s location, it should be considered the access to the road network. Also, the location must have enough space to separate the wards so that patient transfer will be convenient. The EFH should not be next to non-passable rivers and must be close to a water resource and an electrical grid. Moreover, there must be a suitable area for ambulance arrivals and helicopter landings (6). Sarpol-e-Zahab’s EFH was established in the location of the demolished hospital, which was close to the West Terminal and accessed the road, far away from any rivers, and had sufficient space.
In crisis management, standard tents resistant against storm, rain, and fire must be used. In addition, the tents should be multi-level, so in conditions that a part of the tent is perforated, the rest of it can be utilized (17). In Sarpol-e-Zahab’s EFH, Intex tents and tents donated by the Red Crescent Society were used, as well as Conex boxes for laboratory, radiology, and operating room, which was a suitable strategy.
During Haiti earthquake, Israel Defense Forces (IDF) was entered the affected region after 48h with 121 medical staff along with 220 physicians, and established EFH 8h following the equipment arrival (4). Bar-Dayan et al. showed that IDF with 102 staff had established EFH in Adapazari, four days after the Turkish earthquake (9). Military Medical Department of IRGC was present in Bam earthquake area after 2h and started to establish EFH, 30 minutes after arrival, within 24h. Overall, they established 2 EFHs, 33 fields of emergency units, and 13 disaster-relief, also dispatched 185 relief teams, including 1,286 individuals, and sent over 49 tons of medication and healthcare equipment (11). The SUMS’ human workforce team was not sufficient, and the staff had to cover a compressed shift schedule and full time, without any rest in some units. In crisis times, a substitution is needed for each individual so that service provision can be carried out coherently (17). Owing to cultural and linguistic differences, it would help to use local forces for communication.
The IDF’s EFH in the Haiti earthquake had 60 outpatient beds, four ICU beds, and an operating room with one table. Owing to the inefficiency of the medical equipment, they had to increase their admission capacity to 72 patients and add another operating room (4). After changing the arrangement in Sarpol-e-Zahab’s EFH, the number of beds was increased, and the operating room became active.
During 10-day following Adapazari earthquake, 1,205 patients were treated and 35 patients were hospitalized (9). Merin et al. (4) reported that 1,100 patients were visited in 10-day of their activity following Haiti earthquake. Meanwhile, SUMS’s team triaged over 9,000 patients for eight days, but because of manual and incomplete data recording, only the data related to 5,402 patients were recorded in detail. Owing to incoherence between units, there was no accurate data on inpatient and outpatient wards, the operating room, and the patients undergoing electrocardiography and casting.
It was found that the majority of patients referring to Sarpol-e-Zahab’s EFH suffered from signs of the flu and respiratory infections, various types of trauma, and gastrointestinal problems, which might be due to cold season, accidents caused by earthquakes, unhealthy drinking water, and contaminated food. Along with the previous studies, we found that men included a greater percentage of the patients, totally. However, there was not any difference in their age. Horton reported that women are more vulnerable to disasters (18). Bar-Dayan et al. reported that the most prevalent complaints in Adapazari’s Hospital were internal medicine and pediatric diseases (8). Bozkurt et al. (10) concluded that the medical needs in quake-affected areas were dynamic and changed rapidly; therefore, EFH must be prepared to change its activities in accordance with any changes in needs.
Since Sarpol-e-Zahab’s EFH lacked an ICU, critically-ill patients and patients in need of long-term hospitalization were transported to Kermanshah. Merin et al. (4) expressed that due to the impossibility of providing care for all patients, they decided to treat the most urgent cases, which made up for the best expenditure of resources. Their policy was based on early discharge, which allowed them to treat 100 patients/day with 72 beds.
In this EFH, despite physical security, the hospital’s equipment and supplies were stolen. Thus, it is necessary to hold appropriate training courses and employ more powerful individuals in order to achieve better security in crisis times (17). As the support was also weak, especially in the first days, it is better that assistance teams do not impose any extra costs on recipients of assistance. It is recommended that dispatched teams bring along the necessary provisions, such as lightweight camping tents, a sufficient number of sleeping bags, heating equipment, and food for a few days.
Manual data recording, lack of full access to data due to the retrospectively of the study, especially data from before the arrival of the dispatched team and after their departure, and not recording certain data such as final disease diagnoses, administered medications, and treatment plans were the limitations of this study. Furthermore, the data were not fully differentiated based on wards and procedures; therefore, those data were not statistically analyzed. Also, the patients’ data were not recorded according to national ID; therefore, a patient might be visited several times without being specified.
It can be concluded that the rearrangement of EFH based on scientific principles can increase the EFH’s capacity and quality of health services. Despite the desirable performance of SUMS’s team, the data are not sufficient to explore all aspects, and further evidence is required to determine the problems and barriers in the establishment of EFHs and patients’ treatment. This shows the necessity of developing a registry system for crisis times to improve healthcare management, which can be used to inspire the necessary advocacies. Moreover, it is recommended to evaluate hospitals’ preparedness for crisis times, thereby detecting and resolving the problems and weaknesses. It also seems necessary to provide adequate training on crisis management and the methods to deal with disasters.