1. Background
Infertility of women with endometriosis is today's challenge in women’s fertility. According to a global estimation, about 25% - 35% of women with infertility have endometriosis, and up to 50% with endometriosis are infertile. Additionally, about 8% of women candidates for assisted reproductive technology (ART) are diagnosed with endometriosis (1). More than two-thirds of women with endometriosis who underwent controlled ovarian hyper-stimulation require higher total doses of ovulation-stimulation drugs to increase the likelihood of conception; however, the rate of clinical pregnancy, particularly in severe cases, remains considerably low (2, 3). Various reasons raised for the high infertility rate among women with endometriosis such as distorted pelvic structure, endocrine-related ovulatory abnormalities, activated inflammatory cascades, altered peritoneal environment, abnormal uterine bleeding (AUB), and impaired uterine implantation (4-6). Apart from a low conception rate in the background of endometriosis due to its detrimental impact on ovarian responsiveness to hyper-stimulation, its adverse effects on the outcome of pregnancy are noteworthy. Endometriosis can increase the risk of ectopic pregnancy by 30% - 40% (7). The increased risk of preterm labor, small for gestational age, hemorrhagic complications, spontaneous rupture or perforation of utero-ovarian vessels during pregnancy, and also miscarriages are also proposed (8-10). The consequences of ART in women with endometriosis are different from those of the ones without it. Endometriosis is accompanied by a lower number of retrieved oocytes as well as a higher rate of cycle cancellation (11). However, there is a fundamental question about the association between ovulation induction and the risk of endometriosis progression and recurrence. The controlled ovarian hyper-stimulation may increase the risk of endometriosis recurrence due to increased estradiol concentration (12); however, some authors contrarily noted no increased risk of a new endometrioma following the controlled ovarian hyper-stimulation (13). Because of the close relationship between endometriosis and infertility, as well as the adverse impact of endometriosis on fertility after different fertility treatments, the incidence of endometriosis decreases following fertility treatment.
2. Objectives
The present study aimed at assessing the recurrence of endometriosis and its main determinants following fertility treatment with surgery or ART.
3. Methods
The current historical cohort study was performed on all consecutive women with endometriosis undergoing fertility treatments, including laparoscopic surgery or ART in two large hospitals in Tehran in 10 years from 2006 to 2016. All patients with complete hospital records, including demographic characteristics, clinical history, characteristics of endometriosis, and outcomes of ovulation induction, were eligible for the present study. Women with the following features were excluded: onset of pain immediately after delivery, spontaneous pregnancy, symptoms caused by other clinical conditions, and evidence of myoma or other abdominopelvic masses. By reviewing the hospital records, study variables including demographic and socioeconomic characteristics, number of parity and history of abortion, grade, and symptoms of endometriosis, and anthropometric indices were extracted and transferred to the checklist. The patients in the two groups were followed up for five years through both physical examination (to assess the change in clinical manifestations) and sonography assessment to assess endometriosis recurrence. Recurrence of endometriosis was defined as the recurrence of pelvic pain (severity equal or greater than pre-intervention) with palpated pelvic masses or nodulations on pelvic examination and/or presence of ovarian cysts with the typical sonographic findings of endometriomas larger than 20 mm in diameter. In this regard, the recurrence-free survival rate was compared between the two groups, matched by baseline variables. For statistical analysis, IBM SPSS version 21.0 was employed (IBM Corp. 2012. Armonk, NY: IBM Corp.). Baseline characteristics between the two groups were compared using the student or the Mann-Whitney test whenever the data did not appear to have a normal distribution or when the assumption of equal variances was violated across the study groups. Categorical variables were compared using the chi-squared test. Results were expressed as numbers and percentages for categorical variables or mean ± standard deviation (SD) for quantitative variables. Cox proportional hazard analysis was used to determine the difference in recurrence of endometriosis between the methods of fertilization including ART and surgery in the presence of baseline variables including age, body mass index (BMI), education level, occupational status, stage of endometriosis, number of parity, and history of abortion, and the results were presented as hazard ratio (HR) and 95% confidence interval for HR. P values less than 0.05 were considered statistically significant.
4. Results
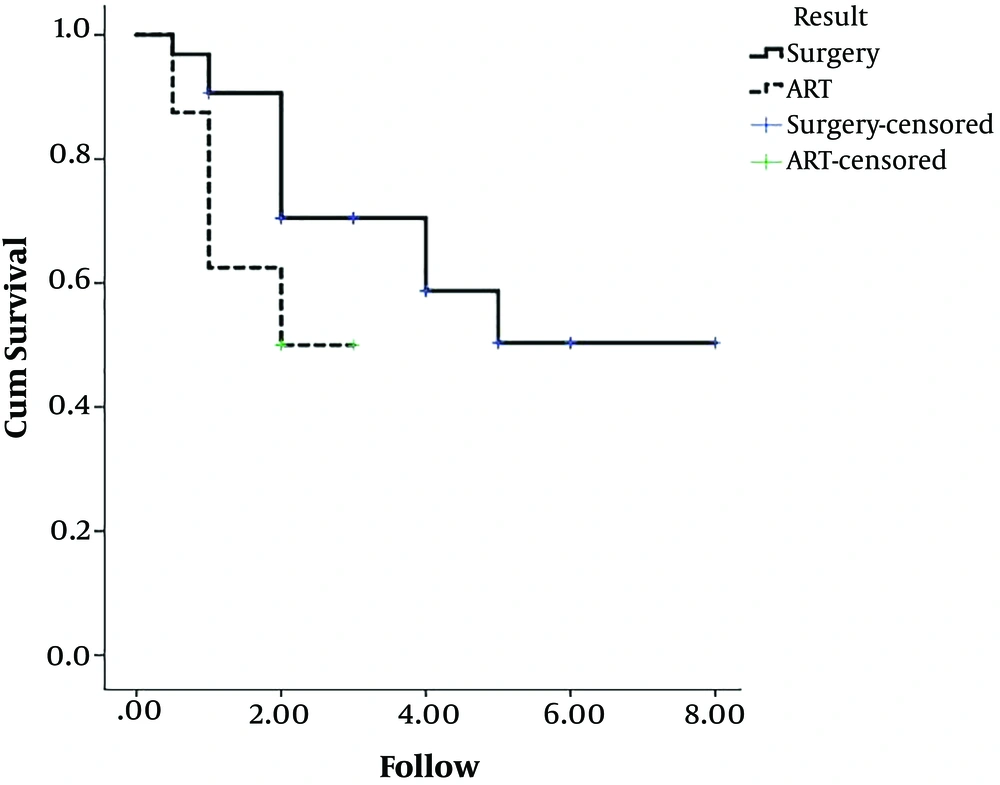
The two study groups included patients undergoing ART (n = 9) or surgery (n = 42). As summarized in Table 1, there was no significant difference in baseline variables including mean BMI, education level, occupational status, number of parity or abortion, history of ectopic pregnancy, and number of children between the two groups; however, the candidates for ART were significantly younger than the ones undergoing surgery. Regarding the stage of endometriosis, stage I was found in 19.1% and 22.2%, stage II in 26.2% and 22.2%, stage III in 9.6% and 11.1%, and stage IV in 45.2% and 44.4% of the ART and surgery groups, respectively with no significant difference (P = 0.991). Within the follow-up time, the rate of endometriosis recurrence was 28.6% and 44.4% in the surgery and ART groups, respectively, indicating no significant difference between the groups (P = 0.436). In this regard, the 1-, 2-, and 3-year recurrence-free rate was 87.5%, 50.0%, and 50.0% in the ART group, and 96.9%, 90.6%, and 70.5% in the surgery group, respectively (Figure 1). The mean time of recurrence in the ART and surgery groups was 1.1 ± 0.6 and 2.3 ± 1.3 years, respectively, indicating no significant difference between the groups (P = 0.108). As shown in Table 2, there was no significant difference in symptoms of endometriosis recurrence, including chronic pelvic pain, dyspareunia, dysuria, dichasia, catheter-related pain, dysmenorrhea, and AUB between the groups. Using the Cox proportional hazard modeling (Table 3) and baseline variables including age, BMI, education level, occupational status, stage of endometriosis, number of parity, and history of abortion, the method of fertilization (ART or surgery) could not affect the long-term recurrence rate of endometriosis (OR = 1.428, 95%CI: 0.177 - 9.900, P = 0.784).
| Item | ART Group (N = 9) | Surgery Group (N = 42) | P Value |
|---|---|---|---|
| Mean age, y | 25.50 ± 3.89 | 32.56 ± 4.50 | 0.010 |
| Mean BMI, kg/m2 | 25.50 ± 3.30 | 23.80 ± 3.81 | 0.242 |
| Education level, % | 0.891 | ||
| Illiterate | 0.0 | 0.0 | |
| Primary school | 11.1 | 15.8 | |
| Diploma | 44.4 | 36.8 | |
| Academic education | 44.4 | 47.7 | |
| Occupational status, % | 0.243 | ||
| Employed | 0.0 | 23.7 | |
| Self-employed | 11.1 | 5.3 | |
| Housewife | 88.9 | 71.1 | |
| Number of gravida, % | 0.063 | ||
| 1 | 66.7 | 35.7 | |
| 2 | 11.1 | 35.7 | |
| 3 | 0.0 | 21.4 | |
| 4 | 0.0 | 4.8 | |
| 5 | 22.2 | 2.4 | |
| Number of parity, % | 0.505 | ||
| 1 | 55.6 | 47.6 | |
| 2 | 33.3 | 42.9 | |
| 3 | 0.0 | 7.1 | |
| 4 | 11.1 | 2.4 | |
| Number of abortion, % | 0.161 | ||
| 0 | 77.8 | 78.6 | |
| 1 | 11.0 | 19.0 | |
| 2 | 0.0 | 2.4 | |
| 3 | 11.1 | 0.0 | |
| History of ectopic pregnancy, % | 0.0 | 2.4 | 0.999 |
| Stage of endometriosis, % | 0.991 | ||
| I | 22.2 | 19.1 | |
| II | 22.2 | 26.2 | |
| III | 11.1 | 9.6 | |
| IV | 44.5 | 45.2 |
aValues are expressed as mean ± SD.
| Item | ART Group (N = 9) | Surgery Group (N = 42) | P Value |
|---|---|---|---|
| Chronic pelvic pain, % | 33.3 | 21.4 | 0.424 |
| Dyspareunia, % | 33.3 | 11.9 | 0.137 |
| Dysuria, % | 22.2 | 4.8 | 0.139 |
| Dichasia, % | 22.2 | 2.4 | 0.077 |
| Catheter-related pain, % | 0.0 | 7.1 | 0.999 |
| Dysmenorrhea, % | 33.3 | 16.7 | 0.353 |
| Abnormal uterine bleeding, % | 11.1 | 0.0 | 0.176 |
| Variable | P Value | HR | 5% for HR |
|---|---|---|---|
| Method of fertilization | |||
| ART (ref) | 1.000 | ||
| Surgery | 0.784 | 1.428 | 0.177 - 9.900 |
| Age, y | 0.645 | 1.043 | 0.873 - 1.245 |
| BMI, kg/m2 | 0.999 | 1.000 | 0.814 - 1.228 |
| Education level | |||
| Illiterate (ref) | 1.000 | ||
| Primary school | 0.445 | 1.618 | 0.471 - 5.560 |
| Diploma | 0.326 | 1.457 | 0.647 - 6.098 |
| Academic education | 0.227 | 1.789 | 0.459 - 5.123 |
| occupational status | |||
| Employed (ref) | 1.000 | ||
| Self-employed | 0.398 | 1.546 | 0.135 - 2.216 |
| Housewife | 0.228 | 1.478 | 0.122 - 3.120 |
| Stage of endometriosis | |||
| I (ref) | 1.000 | ||
| II | 0.448 | 1.277 | 0.680 - 2.398 |
| III | 0.328 | 1.358 | 0.328 - 3.457 |
| IV | 0.656 | 1.478 | 0.560 - 3.895 |
| Number of parity | |||
| 1 (ref) | 1.000 | ||
| 2 | 0.394 | 1.593 | 0.546 - 4.650 |
| 3 | 0.452 | 1.785 | 0.458 - 3.898 |
| 4 | 0.392 | 1.329 | 0.224 - 3.863 |
| History of abortion | |||
| No (ref) | 1.000 | ||
| Yes | 0.389 | 0.589 | 0.176 - 1.967 |
5. Discussion
The subfertility caused by endometriosis is a condition identified several years ago; however, its pathogenesis remains uncertain. In this regard, a high rate of subfertility is reported in women with endometriosis, and about half of subfertile women have endometriosis. The evolution of fertility treatment methods such as laparoscopic surgery and ART increased the chance of conception in women with endometriosis. Another point in such a population is the increased risk of recurrent endometriosis following fertility treatment that can lead to re-experiencing infertility and increased risk of ovarian malignancy. However, it is still not clear which process of ovulation induction is more likely to result in endometriosis recurrence. In the present study, there was no significant difference in the recurrence of endometriosis between surgery and ART as fertility treatments. In other words, the endometriosis recurrence-free survival rate was similar in both fertility treatment techniques. This result could be obtained even after adjusting probable confounders such as the grade of endometriosis, parity, and history of miscarriage. Therefore, it seems that the main criteria for selecting the best fertility treatment considering the risk of recurrent endometriosis are the cost-efficacy, successful ovulation, and patient’s satisfaction. In some recent trials, both fertility treatment methods were accompanied by a low recurrence rate of endometriosis. In a Cochrane review, four randomized clinical trials showed that excisional surgery of ovarian endometrioma led to a favorable outcome considering the recurrence of endometriosis symptoms and subsequent spontaneous pregnancy in women who previously were infertile (14-17); however, there was no consensus on the best surgical techniques to improve the success rate of fertility treatment. In this regard, some studies emphasize the superiority of excision/stripping surgery over the vaporization/coagulation technique due to a lower rate of endometriosis recurrence (18), but some other authors indicate ovarian cystectomy as the surgical choice versus ablation (19). Another point is that the secondary surgery can increase the risk of endometriosis recurrence compared with the primary surgery, and thus, there is a direct relationship between the number of surgeries and the rate of endometriosis recurrence. Vercellini et al. (20), showed that a lower conception rate is expected in patients undergoing a second surgery for recurrent endometriosis compared with the ones who had a primary surgery (22% versus 40%). In this regard, some authors recommend in-vitro fertilization instead of a secondary surgery that can preserve the chance of conception (21).
Compared with surgical techniques, the impact of applying ART for fertilization in women with endometriosis on disease recurrence remains questioned. Similar to surgical interventions, selecting different ART regimens results in different rates of endometriosis recurrence. A study showed that preoperative hormonal treatment did not reduce endometriosis-related pain and recurrence (22), while in another study, the long-term adjuvant hormonal treatment led to the reduction of recurrence rate (23). To the best of authors’ knowledge, the current study was the first that compared the recurrence rate of endometriosis in women undergoing surgery and ART for fertility treatment and could show a similar recurrence rate in both approaches. However, more studies on different ART regimens and repeated surgical procedures are required.
In the current study, the rate of endometriosis recurrence was 28.6% and 44.4% in patients undergoing surgery and ART, respectively, indicating no significant difference between the groups (P = 0.436). A wide range of recurrence rates is reported in various studies from 6% to 67% (24, 25) that might be due to different definitions for endometriosis recurrence, follow-up time, and severity of primary endometriosis (26-28). As indicated in the current study, none of the baseline variables, including the method of fertilization (ART or surgery), patients' age or BMI, stage of endometriosis, and the number of parity or history of abortion could predict disease recurrence. Reviewing the literature showed that history of endometriosis surgery, bilateral pelvic involvement of endometriotic lesions, ovarian endometrioma, tenderness, younger age, history of medication, and advanced-stage disease could predict endometriosis recurrence after fertility treatment (24, 29). Authors believe that to obtain the main indicators for the recurrence of endometriosis following ovulation induction, providing a uniform definition for recurrence, and performing studies with larger sample sizes and higher statistical power, especially for the adjustment of confounders, seems essential.
5.1. Conclusions
The present study showed that the method of fertilization, surgery, or ART, may not affect the rate of endometriosis recurrence in women with subfertility caused by endometriosis. In other words, each of these fertilization methods may be selected to minimize the endometriosis recurrence rate. However, other advantages and disadvantages of these methods should be considered to obtain more conclusive results.