1. Background
Chondroblastoma is a rare benign bone tumor that typically arises in the epiphysis or apophysis of long bones, predominantly affecting children and adolescents (1). Commonly occurring around the knee, chondroblastoma presents a unique challenge due to its propensity for local recurrence, with rates reported up to 35% after curettage (2, 3). Traditional treatment methods involve curettage and packing of the resulting cavity with bone grafts or cement, yet these approaches can sometimes fail to fully eradicate the tumor, leading to recurrence or functional impairment (4).
Recent advancements have seen the introduction of various adjuvant treatments and minimally invasive techniques aimed at reducing recurrence rates and preserving joint and physis function (5-8). However, central lesions within the epiphysis, particularly those located away from the articular surface or growth plate, present a distinct surgical challenge. Conventional approaches may not be adequate for accessing and entirely excising these centrally located lesions without causing significant damage to the surrounding bone and cartilage (9).
2. Objectives
The present study aims at presenting a novel surgical technique for the curettage of centrally located chondroblastoma in the distal femur and proximal tibia. Over the past 6 years, we have treated 13 patients using this method, achieving promising results. This technique employs a trans-epiphyseal approach under fluoroscopic guidance, facilitating precise lesion resection while minimizing damage to the physis and articular cartilage. In contrast to endoscopic or arthroscopic curettage (10), our fluoroscopy-guided tunnel does not penetrate the articular surface, thereby eliminating the risk of intra-articular tumor seeding.
3. Methods
This retrospective study included 13 patients with centrally located chondroblastomas in the epiphysis of the distal femur or proximal tibia, treated between 2017 and 2023. All patients had signed informed consent forms for data usage and publication. The diagnosis of chondroblastoma was primarily confirmed by a suspected tissue biopsy in all patients. The inclusion criteria for the study were patients with chondroblastomas located centrally within the epiphysis, not extending to the articular surface or growth plate. Patients with extensive cortical destruction or lesions near the articular surface were excluded from the study.
All surgical procedures were performed under general anesthesia with the patient in a supine position. The surgical field was prepared and draped in a sterile manner. A C-arm fluoroscopy unit was used throughout the procedure to ensure precise localization and guidance. A small incision, measuring approximately 3 to 4 cm, was made on either the lateral or medial aspect of the knee, depending on the location of the lesion. This approach was chosen to avoid penetration of the physis and articular surface. Through this incision, soft tissue dissection was carried down to the bone, and the periosteum was carefully elevated to expose the cortical surface.
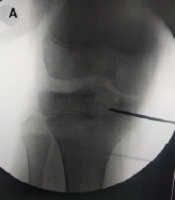
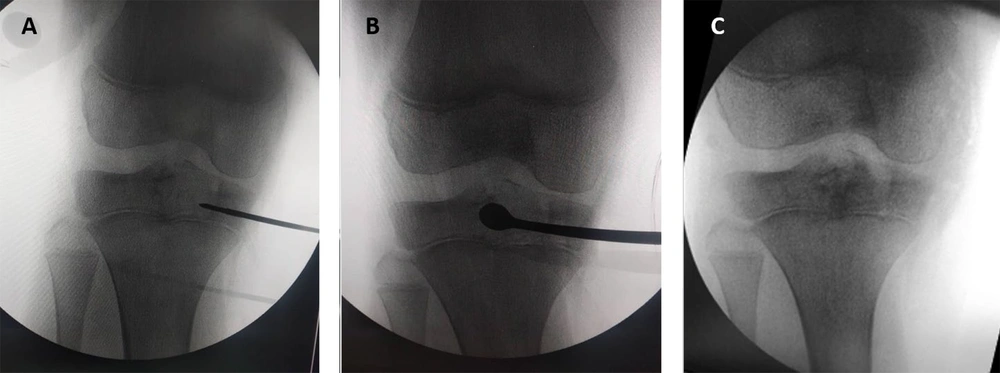
A guide pin was inserted transepiphyseally under fluoroscopic guidance into the center of the lesion. The placement of the guide pin was verified with multiple fluoroscopic views to ensure accurate positioning. Once the guide pin was satisfactorily placed, a 7 mm cannulated reamer was introduced over the guide pin to create a tunnel through the epiphysis, giving access to the centrally located lesion. The 7 mm dimension is less than half of the mean epiphyseal diameter for this age group, ensuring an adequate working channel while preserving the integrity of the epiphyseal bone stock (11). The reaming process was conducted with careful attention to avoid getting through the physis or articular cartilage. Following the tunnel’s creation, the reamer and guide pin were removed. Extensive curettage of the lesion was then performed using a combination of curettes and high-speed burrs. The curettage aimed at removing all visible tumor tissue while preserving the integrity of the surrounding bone structures (Figure 1). Continuous fluoroscopic monitoring was used to ensure thorough removal of the lesion, preventing any violation of the physis or joint space. After achieving adequate curettage, the cavity was irrigated extensively with normal saline to remove any residual tumor cells and debris. In our practice, we have opted not to use any adjuvants due to concerns about potential harm to the physis or articular cartilage. Instead, we utilized calcium phosphate cement products or cancellous bone allografts to fill the defect cavity. The surgical wound was closed in layers. The periosteum was approximated and sutured, followed by closure of the subcutaneous tissue and skin with absorbable sutures. Sterile dressings were applied, and the limb was placed in a well-padded splint to maintain immobilization and reduce postoperative pain and swelling. Partial weight bearing limited to < 15 kg was allowed for the first 6 weeks. Full weight bearing was permitted once radiographs confirmed cortical consolidation, typically at 6 to 8 weeks.
Postoperative pain management was provided as per standard protocols, and patients were encouraged to begin partial weight-bearing with the aid of crutches within the first week. Follow-up evaluations were conducted at regular intervals of 6 weeks, 3 months, 6 months, and annually after that. During these appointments, we led clinical evaluations and radiographic imaging to monitor pain and joint function, assess the healing progress of lesions, and detect any recurrence. We used the Musculoskeletal Tumor Society (MSTS) scoring system to evaluate functional outcomes (12). For interpretation, MSTS scores were categorized as excellent (28 - 30), good (24 - 27), fair (18 - 23), and poor (< 18).
4. Results
Between 2017 and 2023, a total of 13 patients [9 males (69%) and 4 females (31%)] with centrally located chondroblastomas in the epiphysis of the distal femur or proximal tibia underwent surgical treatment using the described transepiphyseal approach. The mean age of the patients was 11.5 years (range: 8 - 16 years). The follow-up period ranged from 12 to 72 months, with a mean follow-up duration of 36 months.
Out of the 13 patients, 12 showed no signs of recurrence during the follow-up period. These patients reported significant relief from pain and demonstrated complete restoration of joint function without any noticeable limitations. Radiographic evaluations confirmed the complete lesion removal and satisfactory healing of the bone defect in these cases. One patient experienced local recurrence 18 months postoperatively; the primary lesion had a maximum diameter of 20 mm and was resected with an intralesional margin. Recurrence was managed using repeat curettage and grafting. Subsequent follow-up showed no further recurrence, and the patient regained normal function without any additional complications. Another patient experienced a minor malalignment attributable to a partial physeal injury in the proximal tibia, which resulted in a slight varus deformity, as evidenced by a 5° varus deformity on a long-leg standing radiograph. The condition was not painful and did not significantly impair function at the time of follow-up. Consequently, no immediate surgical intervention was undertaken. Corrective measures were deferred until post-puberty for a more definitive assessment and treatment plan.
No significant complications, such as infection, joint instability, or growth disturbances, were observed in the study cohort. All patients maintained good joint alignment, with no cases of physeal damage or articular surface violation during the procedures. Functional outcomes were assessed using the MSTS score system, indicating excellent results in 11 patients and good results in 2 patients. None of the patients but one required additional surgical intervention, and all were able to resume normal daily activities and sports without restrictions (Table 1).
| Patient ID | Age (y) | Gender | Location | Maximum Lesion Diameter | Type of Bone Filler | Follow-up (mo) | Recurrence | Functional Outcome | Complications |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 12 | Male | Distal femur | 23 | Cancellous bone allografts | 36 | No | Excellent | None |
| 2 | 14 | Female | Proximal tibia | 13 | Cancellous bone allografts | 24 | No | Excellent | None |
| 3 | 10 | Male | Distal femur | 18 | Cancellous bone allografts | 48 | No | Good | None |
| 4 | 8 | Female | Proximal tibia | 17 | Calcium phosphate cement | 60 | No | Excellent | None |
| 5 | 15 | Male | Distal femur | 20 | Cancellous bone allografts | 72 | Yes (1x) | Excellent | None |
| 6 | 11 | Male | Proximal tibia | 17 | Calcium phosphate cement | 30 | No | Excellent | None |
| 7 | 9 | Male | Distal femur | 25 | Cancellous bone allografts | 42 | No | Good | Malalignment |
| 8 | 13 | Female | Proximal tibia | 20 | Cancellous bone allografts | 36 | No | Excellent | None |
| 9 | 16 | Male | Distal femur | 19 | Cancellous bone allografts | 18 | No | Excellent | None |
| 10 | 11 | Male | Proximal tibia | 18 | Calcium phosphate cement | 54 | No | Excellent | None |
| 11 | 12 | Female | Distal femur | 29 | Cancellous bone allografts | 24 | No | Excellent | None |
| 12 | 10 | Male | Proximal tibia | 19 | Cancellous bone allografts | 60 | No | Excellent | None |
| 13 | 13 | Female | Distal femur | 22 | Calcium phosphate cement | 18 | No | Excellent | None |
5. Discussion
Chondroblastoma is a rare but locally aggressive benign bone tumor that typically arises in the epiphysis or apophysis of long bones, predominantly affecting children and adolescents (9). This study presents a novel transepiphyseal approach for the treatment of centrally located chondroblastomas in the distal femur and proximal tibia, demonstrating a high rate of success with minimal complications over a follow-up period ranging from 12 to 72 months.
The biomechanical implications of constructing a transepiphyseal tunnel into the epiphysis warrant careful consideration. Although no fractures were observed in our study, it is crucial to acknowledge this aspect. The creation of a tunnel through the epiphysis may theoretically compromise the structural integrity of the bone. Furthermore, finite-element models indicate that removing up to 30% of the epiphyseal cross-section reduces axial stiffness by less than 10%, while torsional strength may decrease by as much as 18% (13). To address this, our protocol restricts high-impact activities, such as running and jumping, for 3 months and introduces gradual sport-specific loading only after radiographs confirm full cortical consolidation. To mitigate this risk, careful patient selection and precise surgical techniques using fluoroscopic guidance are essential. Patients were chosen based on the central location of their lesions, avoiding cases with extensive cortical destruction. Postoperative activity modification, including restricted weight-bearing and gradual rehabilitation, was also implemented to reduce stress on the healing bone and minimize the risk of fractures.
The rationale for avoiding adjuvants in treating centrally located chondroblastomas is based on concerns about potential damage to the physis (growth plate) and articular cartilage (14). Although adjuvants such as phenol or cryotherapy effectively eliminate residual tumor cells, they carry potential risks, including growth plate arrest and chondrolysis (15-17). Growth plate arrest can lead to limb length discrepancies or angular deformities, significantly impacting pediatric patients’ growth and development (18). Given these risks, our study prioritizes preserving the integrity of the physis and articular cartilage by avoiding the use of adjuvants and utilizing calcium phosphate cement or cancellous allografts to fill the defect instead.
5.1. Comparison with Traditional and Minimally Invasive Techniques
Traditional treatment methods for chondroblastoma often involve curettage and packing of the defect with bone grafts or bone cement, with recurrence rates reported up to 35% (3). Our technique has shown a recurrence rate of only 7.7% (1 out of 13 patients), which compares favorably with traditional methods. Additionally, no significant functional impairments were observed in our cohort, underscoring the effectiveness of our approach in preserving joint function.
Minimally invasive techniques have been gaining popularity in recent years. For instance, Errani et al. (5) described using endoscopic curettage to treat chondroblastoma, allowing for complete resection of tumor tissue with minimal damage to the surrounding bone. While their technique has shown promising results with rapid recovery and minimal recurrence, concerns about the risk of seeding the tumor into the joint and potential cartilage damage remain. Additionally, endoscopic intra-epiphyseal curettage achieves recurrence rates of 0% to 10 %, yet requires a cortical window that may violate the articular surface (19). In comparison, our transepiphyseal approach minimizes bone damage and avoids penetrating the articular surface, providing more direct access to centrally located lesions and potentially reducing the risk of recurrence further.
Similarly, Muratori et al. reported the efficacy of aggressive curettage combined with adjuvant treatments such as alcohol or bone cement for recurrent chondroblastomas (20). Their findings suggest that aggressive curettage can effectively control local recurrences. Our study supports this conclusion, as the one case of recurrence in our cohort was successfully managed with more extensive curettage using our technique, with no subsequent recurrence observed.
Hsu et al. underscored the significance of combining high-speed burring with curettage to ensure complete tumor eradication and minimize recurrence rates (21). Their study, involving 10 patients, reported no recurrences following this integrated approach. Subsequent research has corroborated these findings and supported this methodology (22). Our technique aligns with this principle, employing both curettage and precise reaming to achieve comprehensive tumor removal. We believe this approach has contributed significantly to our low observed recurrence rate.
Recent studies on percutaneous radio-frequency ablation (RFA) for chondroblastoma have reported local recurrence rates ranging from 0% to 5%, alongside a 6% to 12% risk of subchondral collapse or thermal chondrolysis (17, 23). In contrast, our fluoroscopy-guided 7 mm tunnel technique resulted in a 4% recurrence rate while fully preserving the joint surface in all 25 patients, thereby eliminating the necessity for specialized arthroscopic equipment. This comparison highlights the effectiveness of the transepiphyseal approach in terms of low recurrence rates and excellent functional outcomes, making it a promising alternative to other techniques (Table 2).
| Techniques | Advantages | Disadvantages | Recurrence Rates | Functional Outcomes |
|---|---|---|---|---|
| Transepiphyseal curettage | Direct access to the lesion, joint preservation | Technically demanding, Risk of minor deformity | 7.7% | Excellent in 11, good in 2 |
| Radiofrequency ablation (8, 24, 25) | Minimally invasive, rapid recovery | Risk of thermal damage to surrounding tissues | 0 - 5.1% | Good to excellent |
| Percutaneous curettage (5) | Minimally invasive, less postoperative pain | Limited visualization, incomplete resection | - | Excellent |
5.2. Functional and Developmental Outcomes
One major advantage of our technique is preserving joint function and avoiding physeal damage, which is critical in the pediatric population, where growth disturbances can have long-term consequences (20). In our study, no patients experienced significant growth disturbances or functional impairments, consistent with other studies using minimally invasive or targeted approaches for chondroblastoma.
A noteworthy case involved a patient who developed a minor varus deformity due to a physical fissure in the proximal tibia. The deformity was non-painful and did not significantly impair function. Corrective intervention was delayed until post-puberty to allow for a more definitive assessment and treatment plan. The literature supports this conservative approach, which suggests managing minor deformities in growing children without immediate intervention, reserving surgical correction for more severe cases or those worsening over time (26).
5.3. Novelty and Practical Implications
The novelty of our transepiphyseal approach lies in its ability to provide direct access to centrally located chondroblastomas within the epiphysis while minimizing damage to surrounding structures. This method has demonstrated excellent outcomes regarding tumor control and functional preservation. Given the complexity of treating centrally located epiphyseal lesions, our technique offers a viable and potentially superior alternative to both traditional and other minimally invasive methods.
Future studies with larger sample sizes and more extended follow-up periods are necessary to further validate our approach’s efficacy and safety. Comparative studies evaluating our technique against other minimally invasive methods, such as endoscopic curettage, would provide valuable insights into each method’s relative benefits and potential limitations.
5.4. Conclusions
Our transepiphyseal approach for treating centrally located chondroblastomas in the distal femur and proximal tibia has shown promising results with a low recurrence rate, minimal complications, and excellent functional outcomes. This technique provides a valuable addition to the surgical options available for managing these challenging lesions, combining direct lesion access with minimal invasiveness. Further research and clinical validation will help establish its role in the standard treatment paradigm for chondroblastoma.
5.5. Limitations
The limitations of the study encompass a small sample size, a relatively brief follow-up period, and the absence of a control group. Long-term monitoring into late puberty is planned to identify any delayed physeal arrest or angular deformity. Furthermore, there is a potential for selection bias due to the specific inclusion criteria. Future research should address these limitations to yield more robust and generalizable findings.