1. Background
Bladder cancer (BC), the ninth most common cancer in the world, caused more than 614,000 new cases in 2022 (1). The age-standardized incidence rates (ASRs) in men and women were 9.3 and 2.4 per 100,000 population, respectively (1). The occurrence of BC rises in the sixth decade of life and beyond, primarily affecting the elderly. It is notably more common in men, who are 3 - 4 times more likely to develop the disease than women (2). This cancer is more prevalent in regions such as North America, Southern and Western Europe, parts of the Mediterranean, and specific areas of North Africa (3).
In Iran, BC is ranked seventh in common types of cancer, with 6400 new cases annually (1). GLOBOCAN 2022 estimates the ASR at 7.1 per 100,000, with higher rates in men (12.1) compared to women (2.0), and also predicts over 8,000 new cases (ASR = 8.5) by 2025 (1, 4). Historical data show rising trends: From 14.3 (men) and 3.0 (women) in 2014 to 16.2 and 3.5 in 2016 (5, 6). The prevalence of BC in Iran varies by region, with the central provinces exhibiting higher rates (6). Among men, the highest ASR of BC was observed in Kerman 27.3, while the lowest rate was reported in Ilam (6.5); for women, Kohgiluyeh and Boyer-Ahmad is the highest (5.4) and Qom the lowest (1.2) (6, 7). Local studies have reported ASRs in Semnan (12.2 men, 3.0 women) and Shahroud-Meyami (9.4 men, 3.2 women) (7, 8).
Recent findings indicated that opium is a significant risk factor for BC, with an odds ratio of 5.0 (3.8 to 6.7) (9). Another significant risk factor is Schistosoma haematobium infection, which plays a major role in BC cases across many regions of Africa (10). Opium consumption is prevalent in the Iranian population (11). In Iran, individuals exposed to both smoking and opium face a 6.2 times higher risk (2.04 - 18.7) of developing BC (12). Other contributing risk factors include frequent consumption of red meat (more than four times per week), intake of animal fat, and occupational exposures such as aromatic amines and paint components (12, 13).
Cancer registries are essential for collecting and analyzing data, which helps identify trends, guide research, and inform prevention and control strategies (14). Given the lack of BC data in Iran since 2016, updated information is needed.
2. Objectives
This study analyzed BC incidence and trends over 13 years across all ages and both genders to provide insights for improving cancer prevention and management.
3. Methods
This descriptive time series study was conducted based on data from the population-based cancer registry system at Shahroud University of Medical Sciences. Patients included were new cases with BC registered from 2010 to 2022 in Shahroud and Meyami districts of northwest Iran. According to the International Classification of Diseases (ICD-10), using code C67 for defining BC.
Population estimates for 18 age groups were obtained by interpolating data between the 2011 and 2016 census periods. Both crude rate and ASR (per 100,000 population) were calculated, with ASR estimated using the direct standardization method. In this study, age and sex were considered potential confounding factors and were controlled by calculating ASRs and presenting them separately across age and sex groups. To compare findings with previous studies, the old standard population (Segi) was applied (15) while the new World Health Organization (WHO) standard population was used for a more precise estimation of the ASR (16). The 95% confidence intervals were calculated for the ASR. The ASR for BC was measured across different age and sex groups. The annual percentage change (APC) and the average annual percentage change (AAPC) were calculated using Joinpoint 5.0.0.1 software. This study was approved by the Ethics Committee of Shahroud University of Medical Sciences (ethics code: IR.SHMU.REC.1401.150).
4. Results
A total of 298 BC patients were registered in Shahroud and Meyami districts between 2010 and 2022. Men comprised the majority of patients compared to women (80.9% vs 19.1). The mean age for men and women was 64.5 ± 14.5 and 64.9 ± 14.7, respectively.
Table 1 displays the incidence rates, both crude and ASR, stratified by sex according to the WHO’s updated population and SEI standard. Over the 13 years, the ASR was 8.9 [95% confidence interval (CI): 7.9 - 10.0] per 100,000 population, with 14.1 (95% CI: 12.4 - 16.1) among men and 3.4 (95% CI: 2.6 - 4.5) among women. The ASR was lowest in 2010 (4.9, 95% CI: 2.0 - 7.8) and highest in 2018 (13.7, 95% CI: 8.9 - 18.4). The highest ASR was observed in women in 2011, at 6.8 (95% CI: 1.7 - 11.8), while the highest ASR among men was recorded in 2022, at 23 (95% CI: 14.5 - 31.6).
| Year and Sex | Population | CIR | Old ASR (95% CI) | New ASR (95% CI) |
|---|---|---|---|---|
| 2010 | ||||
| Women | 115,719 | 1.7 | 1.4 (0.0 - 3.3) | 1.8 (0.0 - 4.3) |
| Men | 119,333 | 7.5 | 6.6 (2.2 - 11.0) | 7.9 (2.7 - 13.1) |
| Both | 235,052 | 4.7 | 4.0 (1.6 - 6.4) | 4.9 (2.0 - 7.8) |
| 2011 | ||||
| Women | 118,623 | 5.9 | 6.0 (1.4 - 10.6) | 6.8 (1.7 - 11.8) |
| Men | 120,207 | 7.5 | 6.8 (2.0 - 11.6) | 8.1 (2.6 - 13.5) |
| Both | 238,830 | 6.7 | 6.4 (3.1 - 9.7) | 7.4 (3.7 - 11.1) |
| 2012 | ||||
| Women | 120,408 | 2.5 | 1.8 (0.0 - 4.0) | 2.1 (0.0 - 4.7) |
| Men | 122,015 | 13.9 | 15.9 (8.2 - 23.7) | 17.7 (9.3 - 26.1) |
| Both | 242,423 | 8.3 | 8.9 (4.8 - 12.9) | 9.9 (5.5 - 14.3) |
| 2013 | ||||
| Women | 122,221 | 5.7 | 4.8 (1.0 - 8.6) | 6.6 (1.7 - 11.5) |
| Men | 123,852 | 9.7 | 10.6 (4.4 - 16.8) | 11.6 (5.0 - 18.3) |
| Both | 246,073 | 7.7 | 7.7 (4.1 - 11.3) | 9.1 (5.0 - 13.3) |
| 2014 | ||||
| Women | 124,062 | 1.6 | 1.4 (0.0 - 3.4) | 1.7 (0.0 - 4.0) |
| Men | 125,716 | 14.3 | 13.2 (6.6 - 19.9) | 15.4 (8.0 - 22.8) |
| Both | 249,778 | 8.0 | 7.3 (3.8 - 10.8) | 8.5 (4.6 - 12.4) |
| 2015 | ||||
| Women | 125,925 | 0.0 | 0.0 | 0.0 |
| Men | 127,605 | 15.7 | 15.5 (8.2 - 22.8) | 18.0 (9.9 - 26.2) |
| Both | 253,530 | 7.9 | 7.8 (4.1 - 11.4) | 9.0 (4.9 - 13.1) |
| 2016 | ||||
| Women | 126,705 | 3.2 | 3.0 (0 - 6) | 3.1 (0.1 - 6.1) |
| Men | 130,641 | 16.8 | 17.8 (10.1 - 25.4) | 19.3 (11.1 - 27.4) |
| Both | 257,346 | 10.1 | 10.4 (6.3 - 14.5) | 11.2 (6.8 - 15.5) |
| 2017 | ||||
| Women | 128,612 | 5.4 | 4.6 (1.2 - 8.1) | 5.6 (1.5 - 9.8) |
| Men | 132,607 | 11.3 | 12.6 (6.1 - 19.1) | 13.1 (6.4 - 19.7) |
| Both | 261,219 | 8.4 | 8.6 (4.9 - 12.3) | 9.4 (5.4 - 13.3) |
| 2018 | ||||
| Women | 130,548 | 6.1 | 5.7 (1.7 - 9.7) | 6.5 (2 - 11) |
| Men | 134,602 | 17.8 | 18.3 (10.7 - 25.9) | 20.8 (12.4 - 29.2) |
| Both | 265,150 | 12.1 | 12.0 (7.7 - 16.3) | 13.7 (8.9 - 18.4) |
| 2019 | ||||
| Women | 132,510 | 3.0 | 2.5 (0.0 - 5.1) | 3.1 (0.1 - 6.0) |
| Men | 136,628 | 13.2 | 13.4 (7.1 - 19.7) | 14.7 (7.9 - 21.5) |
| Both | 269,138 | 8.2 | 8.0 (4.6 - 11.4) | 8.9 (5.1 - 12.6) |
| 2020 | ||||
| Women | 134,505 | 3.0 | 3.2 (0.1 - 6.4) | 3.2 (0.1 - 6.3) |
| Men | 138,684 | 15.9 | 16.3 (9.3 - 23.3) | 17.9 (10.4 - 25.4) |
| Both | 273,189 | 9.5 | 9.8 (5.9 - 13.6) | 10.5 (6.5 - 14.6) |
| 2021 | ||||
| Women | 136,528 | 5.1 | 5.0 (1.2 - 8.7) | 5.5 (1.4 - 9.6) |
| Men | 140,771 | 18.5 | 18.7 (11.2 - 26.1) | 20.5 (12.6 - 28.4) |
| Both | 277,299 | 11.9 | 11.8 (7.6 - 16) | 13.0 (8.5 - 17.5) |
| 2022 | ||||
| Women | 138,581 | 1.4 | 1.2 (0 - 2.9.0) | 1.4 (0.0 - 3.3) |
| Men | 142,887 | 19.6 | 21.4 (13.3 - 29.6) | 23.0 (14.5 - 31.6) |
| Both | 281,468 | 10.7 | 11.3 (7.2 - 15.5) | 12.2 (7.8 - 16.6) |
Abbreviations: ASR, age-standardized incidence rate; 95% CI, 95% confidence interval.
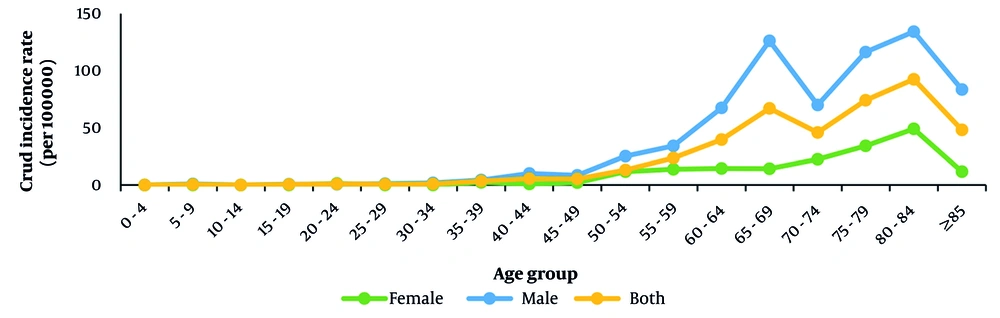
Figure 1 depicts the crude incidence rate by sex and age groups. In women, the incidence rate generally increased with age but decreased after age 84. In men, the incidence rate also increased with age; however, it declined slightly between the ages of 65 and 69, then rose again until age 84 before decreasing. Across all age groups, men had higher BC incidence rates than women.
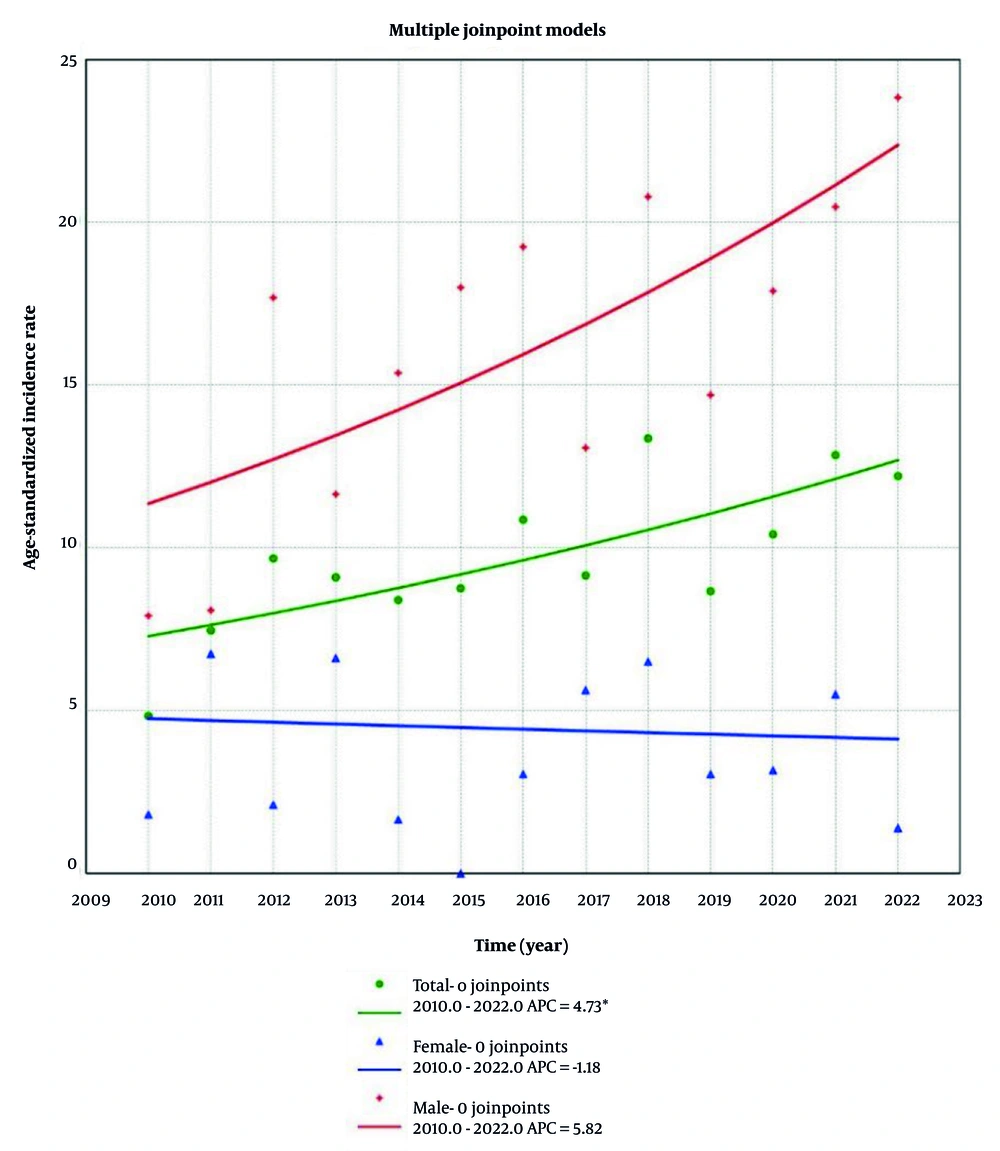
Between 2010 and 2022, the APC was 4.7% (95% CI: 1.3 - 9.0). It can be observed that APCs for men and women were 5.8% (95% CI: -0.6 - 14.0) and -1.2% (95% CI: -13.6 - 14.8), respectively (Figure 2). More details can be found in Figure 2 and Table 2.
Abbreviations: 95% CI, 95% confidence interval; APC, annual percentage change; AAPC, average annual percentage change.
a It belongs to AAPC.
b The APC and AAPC are significantly different from zero (P < 0.05).
5. Discussion
In this study, we shed light on how the incidence and trend of BC have changed during 13 years in Shahroud and Meyami districts. The results revealed that there was an increasing trend from 2010 to 2022 with an average annual increase of 4.7%. Throughout the study period, the ASR was 8.9 per 100,000 population.
By comparing the ASR of BC among men and women in this study with the national ASR reported in 2014, it is evident that the regional ASR is largely consistent with the country's ASR (6). Findings from a national study showed that in 2016, the ASR was 16.2 for men and 3.5 for women. Among men, the highest ASR was reported in Kerman and East Azarbayjan, while the lowest was observed in Sistan and Baluchistan and Zanjan. For women, Yazd and North Khorasan recorded the highest ASR, whereas Illam and Sistan and Baluchistan had the lowest rates (5). A study based on data from the cancer registry system during 2014 - 2016 revealed that the ASR in Iran was 13.7 for men and 2.9 for women. In Semnan, these rates were slightly different, with an ASR of 14.1 for men and 2.3 for women (4).
Several studies have reported ASRs of BC in various provinces of Iran, consistently indicating higher rates in men compared to women. A study conducted in Mazandaran province in 2014 reported ASRs of 8.2 per 100,000 population for men and 5.4 per 100,000 population for women (17). Similarly, research from East Azerbaijan province during 2015 - 2016 found that men had a significantly higher ASR than women, with rates of 19.8 versus 4.6 per 100,000 population, respectively (18). In Isfahan Province, data from 2015 - 2018 also demonstrated this pattern, with an ASR of 19.9 per 100,000 for men and 3.4 per 100,000 population for women (19). One of the main factors associated with this difference is smoking (20). Results of a study showed that the high incidence rates of BC among men in the United States and Spain reflect the high prevalence of male smokers in these countries, 30 to 40 years prior (3). Additionally, sex hormones and their receptors play a role in BC pathogenesis, with androgens promoting tumor growth through the androgen receptor (AR) located on the X chromosome. Genetic differences, including variations in sex chromosomes, further contribute to the observed disparities in BC incidence between men and women (21).
The results revealed an increase in both the incidence and pattern of BC over time. According to a 10-year study conducted in the Shahroud and Meyami districts, the ASR was 6.3, which was lower than the ASR reported in the following decade (8). This trend may reflect demographic changes, particularly population aging, as life expectancy in Iran has increased, and a larger proportion of the population is reaching ages at higher risk of BC (22). Additionally, improvements in diagnostic capacity and cancer registration systems, along with changes in exposure to risk factors such as tobacco smoking and occupational carcinogens, may contribute to the rising incidence (5, 7).
In this study, the increasing incidence trend of BC, both overall and among men, was consistent with findings from other studies in Iran and globally (4, 5, 23). In contrast, the incidence trend among women remained relatively stable, aligning with patterns observed in Northern European women (3). One possible explanation for this stability could be consistent changes in disease classification over time (24). The transition from ICD-9-CM to ICD-10-CM for BC involved consistent but more detailed classification changes. However, these changes did not significantly alter the overall incidence trends, because the fundamental definition of BC remained the same (25).
The ASR showed an increasing trend with age, peaking at 84 years, and subsequently declining. This pattern is consistent with findings reported in other studies (7, 26). This decrease in ASR among individuals aged 84 and older may be attributed to poorer overall health and higher rates of non-cancer-related mortality in this age group (27).
The main strength of this study was analyzing 13 years of BC incidence and trends, along with calculating ASR using both the old and new WHO standard populations. However, one limitation of this study was the lack of an analysis of risk factors. Due to this limitation, we were unable to examine potential risk factors that could help identify the causes of the increased incidence of this cancer. Additionally, while the findings are specific to the Shahroud and Meyami districts, they may offer insights applicable to similar populations in other regions with comparable demographic and environmental characteristics.
5.1. Conclusions
Between 2010 and 2022, the overall incidence of BC in Shahroud and Meyami increased among men but remained stable in women. Further research is needed to identify the underlying causes of these trends.