1. Introduction
Epstein-Barr virus (EBV), a ubiquitous gammaherpesvirus infecting over 90% of the global population, has traditionally been viewed as a clinically silent passenger, typically acquired in early life, persisting latently in memory B cells, and rarely causing overt disease in immunocompetent hosts. However, recent research increasingly recognizes EBV as a potent immunological modulator, capable of subverting host immune tolerance and initiating organ-specific autoimmunity through mechanisms such as molecular mimicry, epitope spreading, and immune cell dysregulation (1-4). Among the virus’s less frequently discussed but clinically significant target is the thyroid gland, particularly during the developmental phases of childhood and adolescence, when the endocrine–immune axis exhibits heightened plasticity and vulnerability to latent viral perturbation. EBV has been implicated in the pathogenesis of autoimmune thyroid disorders, notably Graves’ disease and Hashimoto’s thyroiditis, where viral persistence promotes chronic lymphocytic infiltration, cytokine-driven inflammation, and immune escape within the thyroid microenvironment (1-4).
In younger individuals, the clinical presentation of autoimmune thyroiditis can be subtle, often masked by nonspecific symptoms such as growth retardation, mood alterations, fatigue, and cognitive impairment, which may be misattributed to behavioral or developmental issues. Notably, EBV-positive patients tend to exhibit more aggressive disease phenotypes, including refractory hyperthyroidism, rapid glandular deterioration, and poor response to pharmacotherapy, frequently necessitating definitive intervention earlier than in typical cases managed conservatively (5, 6). Preservation of thyroid integrity during childhood is essential for normal growth and metabolic regulation. The gland orchestrates crucial physiological functions, ranging from neurological maturation and skeletal mineralization to energy homeostasis and pubertal progression, and its disruption can produce irreversible consequences. Both hypothyroidism and hyperthyroidism during formative years have been linked to long-term sequelae, including cardiovascular dysfunction, osteopenia, and neurocognitive underachievement (7, 8).
Advances in diagnostic imaging and interventional endocrinology have recently redefined therapeutic possibilities for pediatric and adolescent thyroid disorders. Ultrasound-guided, minimally invasive interventions—such as radiofrequency ablation (RFA), ethanol ablation (EA), and minimally invasive video-assisted thyroidectomy (MIVAT)—have emerged as safe and effective alternatives to conventional surgery. These techniques enable targeted ablation of inflamed or nodular thyroid segments while sparing surrounding parenchyma, thereby minimizing postoperative hypothyroidism and optimizing cosmetic outcomes. Such attributes are particularly valuable for younger patients, who face heightened psychosocial sensitivity to visible scarring and greater physiological risk from extensive thyroid resection (9-12).
In the setting of EBV-associated thyroid disease, the rationale for precision ablation becomes even stronger. Viral inflammation can distort glandular architecture, compromise surgical mapping, and heighten the risk of postoperative dysfunction. Image-guided ablative approaches, by contrast, permit fine-tuned lesion targeting, controlled energy delivery, and lower procedural trauma, making them especially suitable for smaller, hormonally active glands (13, 14). Nonetheless, EBV’s influence extends beyond anatomical distortion; it reshapes the local immune milieu, promoting cytokine imbalance and altered immune recovery. In younger hosts with evolving immune systems, these viral-host interactions can modify post-ablation healing dynamics, predispose to transient endocrine instability, and influence long-term hormonal feedback loops.
Despite progress in minimally invasive techniques, clinical outcomes remain variable in EBV-related thyroid dysfunction. Response patterns appear modulated by viral load, host immune polarization (e.g., Th1 versus Th17 dominance), and the sensitivity of the hypothalamic-pituitary-thyroid axis. This complexity highlights the need for a holistic, biomarker-driven therapeutic model that integrates viral serology, cytokine profiling, high-resolution ultrasonographic features (echogenicity, vascularity, and margin clarity), and dynamic endocrine metrics such as TSH, FT3, and FT4 (15-17).
In this context, the present study was undertaken to advance an infection-aware, hormone-conserving therapeutic framework for managing EBV-associated thyroid dysfunction. By synthesizing global experience with ultrasound-guided ablation modalities, this review examines how viral immunobiology intersects with procedural response profiles, influencing recovery, recurrence, and endocrine stability. Particular emphasis is placed on refining patient selection and risk stratification tools, optimizing procedural timing and energy parameters, and designing long-term surveillance strategies aimed at preserving endocrine capacity and developmental continuity (18, 19).
2. Objectives
This study was designed to comprehensively evaluate the therapeutic potential and clinical outcomes of ultrasound-guided, minimally invasive thyroid ablation techniques in individuals affected by EBV-associated autoimmune thyroid dysfunction. The primary aim was to elucidate how EBV-driven immune modulation influences thyroid disease onset, progression, and responsiveness to targeted ablation therapies, while also assessing its impact on long-term endocrine stability and recovery. Although several of the analyzed studies included younger participants, reflecting the heightened immunological susceptibility of this group, the investigation was deliberately structured to remain broad, inclusive, and generalizable across all age cohorts in which EBV seropositivity and thyroid pathology coexist.
Only studies providing laboratory-confirmed evidence of EBV infection, determined through serological assays (e.g., VCA-IgM, EBNA-IgG) or molecular detection techniques such as PCR amplification of EBV DNA in blood or thyroid tissue, were included. The principal disease entities examined comprised Graves’ disease, Hashimoto’s thyroiditis, and EBV-associated thyroid nodular disease, representing the diverse autoimmune and inflammatory spectrum in which viral persistence may influence both disease phenotype and therapeutic outcomes.
3. Methods
3.1. Literature Search Strategy
A comprehensive and systematic literature search was conducted to identify all relevant studies evaluating minimally invasive thyroid ablation in EBV-associated thyroid disease. Major scientific databases, including PubMed Central, Scopus, Web of Science, SpringerLink, ERIC, and Google Scholar, were searched from their inception through March 2025. To ensure the inclusion of studies from low-resource settings, HINARI was additionally used for full-text access where required. The search strategy adhered to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA 2020) guidelines (20) to ensure methodological transparency and reproducibility.
Search terms combined both controlled vocabulary (MeSH terms) and free-text keywords using Boolean operators (AND, OR, NOT) to maximize sensitivity and specificity. The following representative terms were applied across databases: “Epstein-Barr virus and thyroid,” “ultrasound-guided thyroid ablation,” “radiofrequency ablation in autoimmune thyroiditis,” “ethanol ablation and Graves’ disease,” “minimally invasive thyroid interventions,” and “thyroid nodules and viral inflammation.” Reference lists of all included studies were manually screened to identify additional relevant publications not captured in the primary search.
3.2. Inclusion and Exclusion Criteria
Studies were included if they met all of the following criteria: (1) EBV infection confirmed by serological or molecular methods; (2) autoimmune thyroid disease diagnosis, with or without nodular changes; (3) use of minimally invasive thyroid intervention, such as RFA, EA, or MIVAT under ultrasound guidance; and (4) reporting of at least one clinically relevant outcome, thyroid nodule volume reduction, hormonal restoration (TSH, FT3, FT4), recurrence, procedure-related complications, or cosmetic satisfaction
Studies were excluded if they lacked documented EBV status, did not report procedural or endocrine outcomes, were limited to case reports, reviews, or conference abstracts, or scored below 5 on the Newcastle-Ottawa Scale (NOS) for methodological quality.
3.3. Data Extraction Process
Two reviewers independently extracted data using a predesigned standardized form to ensure consistency. Extracted parameters included patient demographics (age, sex, EBV status, and disease type), thyroid hormone levels (TSH, FT3, FT4), nodule characteristics (size, echogenicity, vascularity, and anatomical distribution), and procedural details (type of ablation, energy settings, sedation protocol, duration, and follow-up period). Clinical outcomes—including volume reduction rate (VRR), endocrine stabilization, complication rate (e.g., hypothyroidism, bleeding, infection), recurrence, and hospital stay—were systematically documented. Patient-reported outcomes, when available, such as cosmetic satisfaction and overall quality-of-life improvement, were also extracted. Any discrepancies between reviewers were resolved through discussion, and unresolved conflicts were adjudicated by a third senior reviewer to ensure data accuracy and objectivity.
3.4. Quality Assessment
The ROBINS-I tool was not applied in this review because it is specifically designed for comparative non-randomized studies that evaluate the effect of an intervention relative to a defined control group within a target-trial framework. In the present analysis, most of the included studies were non-comparative observational or procedural reports describing outcomes of image-guided thyroid ablation in EBV-associated thyroid disease, without a concurrent comparator arm. Therefore, several ROBINS-I domains, such as confounding and classification of interventions, were not applicable to our data.
To ensure methodological rigor, study quality was instead appraised using parameters better suited to the nature of the included evidence, focusing on clarity of study design, diagnostic confirmation of EBV infection, transparency and reproducibility of ablation protocols, consistency in reporting clinical and hormonal outcomes, operator experience, and adequacy of follow-up. This context-specific approach, adapted from established observational study appraisal frameworks, provided an accurate and transparent assessment of methodological quality while maintaining alignment with the clinical and procedural scope of the review.
We used the NOS because most included studies were observational cohorts reporting clinical outcomes after image-guided thyroid ablation, making NOS an appropriate, widely accepted tool to appraise nonrandomized evidence. Two reviewers independently applied the NOS across its three domains, Selection, Comparability, and Outcome, with disagreements resolved by a third reviewer to ensure consistency. We predefined decision rules to keep judgments transparent and tailored to our topic: under Selection, studies earned stars for clearly defined cohorts, representative sampling, and, critically for this review, robust EBV ascertainment (serology and/or PCR) as part of exposure/eligibility verification. Under Comparability, stars were awarded when analyses accounted for key confounders relevant to ablation outcomes (e.g., age, baseline thyroid status and autoimmunity, nodule size/vascularity, and intervention type such as RFA vs EA vs MIVAT/TOETVA), either through matching, stratification, or multivariable adjustment. Under Outcome, we prioritized precision and consistency of definitions (e.g., VRR formula, hormone thresholds), objective assessment (ultrasound parameters, laboratory assays), adequacy of follow-up for endocrine stabilization and recurrence, and completeness of outcome reporting including complications.
We also documented technical transparency (ultrasound guidance, energy settings, operator experience) as part of Selection/Outcome credibility because procedural clarity directly affects internal validity in device- and technique-driven studies. Each study could receive up to nine stars; consistent with our protocol, studies scoring < 5 were excluded, 5 - 6 were considered moderate quality, and ≥ 7 high quality. To reflect the reviewer’s request for visual clarity, we translated NOS domain judgments into traffic-light risk summaries and performed sensitivity analyses excluding lower-scoring studies to test robustness of pooled estimates. While we recognize NOS has limitations (e.g., less granular for single-arm designs), we mitigated this by adding topic-specific criteria (EBV confirmation, standardized outcome definitions, longitudinal follow-up, and protocol/operator transparency) so that quality ratings meaningfully captured the virology-procedural context of this review.
3.5. Protocol Transparency
The search strategy for this review was developed and reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2020 guidelines by Page et al. (2021) (20). All major steps, including database selection, keyword formulation, Boolean logic, and inclusion/exclusion criteria, were structured to meet PRISMA 2020 standards for transparency and reproducibility. The reference was incorporated as the methodological foundation guiding the formulation of search terms, screening workflow, and presentation of the PRISMA flow diagram in this study.
Although international registries such as PROSPERO promote transparency in prospective systematic reviews, registration was not required nor methodologically appropriate for the present investigation. This study synthesizes retrospectively available clinical data from published literature on EBV-associated thyroid disease and image-guided ablation outcomes, integrating both comparative and non-comparative observational studies.
PROSPERO’s scope is explicitly limited to prospectively designed reviews of interventional or exposure-effect relationships and excludes reviews that have already completed data collection, screening, or analysis. As our review was conceived after preliminary extraction and quality assessment of available reports, retrospective registration would provide no methodological safeguard against reporting bias and would in fact contravene PROSPERO’s eligibility criteria. Furthermore, PRISMA 2020 and the Cochrane Handbook specify that authors must report whether a protocol exists, but neither standard mandate formal registry submission. Instead, methodological transparency has been ensured through (1) strict adherence to PRISMA 2020 reporting items, (2) detailed disclosure of all inclusion/exclusion criteria and analytic procedures within this manuscript, and (3) public sharing of the full protocol and search strategy on the Open Science Framework (OSF). Hence, under the design, scope, and completion stage of this study, PROSPERO registration was not only unnecessary but ineligible, and transparency has been achieved through equally rigorous, open-access documentation consistent with international best practices.
3.6. Ultrasound Guidance and Technical Protocols
All procedures were conducted under real-time, high-frequency ultrasound guidance using linear probes (7 - 15 MHz) to ensure precise targeting and safety. Ablation parameters, including power output (watts), total energy delivery (joules), and frequency of application, were tailored according to nodule dimensions, vascularity, anatomical location, and proximity to critical structures such as the recurrent laryngeal nerve and carotid sheath. RFA was performed via percutaneous electrode insertion, with sequential energy delivery continued until uniform tissue hyperechogenicity and visible nodule shrinkage were achieved. EA involved ultrasound-guided intralesional injection of absolute ethanol, followed by continuous real-time monitoring to ensure homogeneous dispersion within the lesion. In select patients, MIVAT was used, utilizing small anterior cervical incisions to achieve targeted lesion excision while preserving surrounding glandular tissue and minimizing cosmetic impact.
3.7. Outcomes and Definitions
Primary Clinical Outcomes:
The VRR: Calculated as (Initial Volume - Final Volume)/Initial Volume × 100%
Hormonal Recovery: Defined as the normalization or significant improvement of serum TSH, FT3, and FT4 levels following the ablation procedure.
Complications: Included the incidence of hypothyroidism, hematoma, infection, transient or persistent voice changes, and any requirement for re-intervention.
Secondary Outcomes:
Cosmetic Outcomes: Assessed using patient- and physician-reported satisfaction scores, focusing on scar visibility, neck contour, and aesthetic appearance.
Hospital Stay Duration: Measured as the time from admission to discharge following the procedure.
Recurrence Rate: Defined as nodule regrowth or re-emergence of thyroid-related symptoms within 6 - 24 months of follow-up.
Patient Satisfaction and Quality of Life: When reported, subjective feedback regarding post-procedural comfort, recovery, and overall therapeutic acceptability was included to complement objective clinical data.
3.8. Data Sources and Nature of Evidence
The present investigation was conducted strictly as a systematic review and meta-analysis and did not involve the performance of any new laboratory tests, patient enrollment, or direct clinical experimentation. All biochemical, serological, and imaging data incorporated into the analysis were extracted exclusively from previously published peer-reviewed studies that had independently conducted these investigations. Laboratory parameters such as thyroid hormone concentrations (TSH, FT3, FT4), antibody titers, and EBV diagnostic profiles (including VCA-IgM, EBNA-IgG, or PCR detection of viral DNA) were recorded exactly as reported by the original authors. These variables were synthesized for comparative and pooled analysis to evaluate endocrine recovery, inflammatory response, and post-ablation outcomes across studies.
No human participants were recruited, and no additional biological sampling or testing was performed by the current authors. Ethical approval was therefore not required, as the review utilized secondary data already available in the scientific literature. To ensure full methodological transparency, all extracted laboratory information is explicitly referenced to its original source within the data-extraction framework. The article type has been clearly defined throughout the manuscript, including the title, abstract, and methods, as a Systematic Review and Meta-analysis, reflecting that the work is a secondary synthesis of published evidence rather than a primary laboratory or patient-based investigation.
3.9. Subgroup and Comparative Analyses
To characterize sources of variability, predefined subgroup analyses compared: (1) EBV-seropositive vs. EBV-seronegative individuals; (2) ablation modality (RFA vs. EA vs. MIVAT); (3) age category (≤ 18 vs. > 18 years, where stratified data were available); (4) sex-specific differences in procedural outcomes; and (5) nodule pathology (benign colloid nodules vs. lesions with suspicious cytology or inflammatory features).
3.10. Statistical Analysis
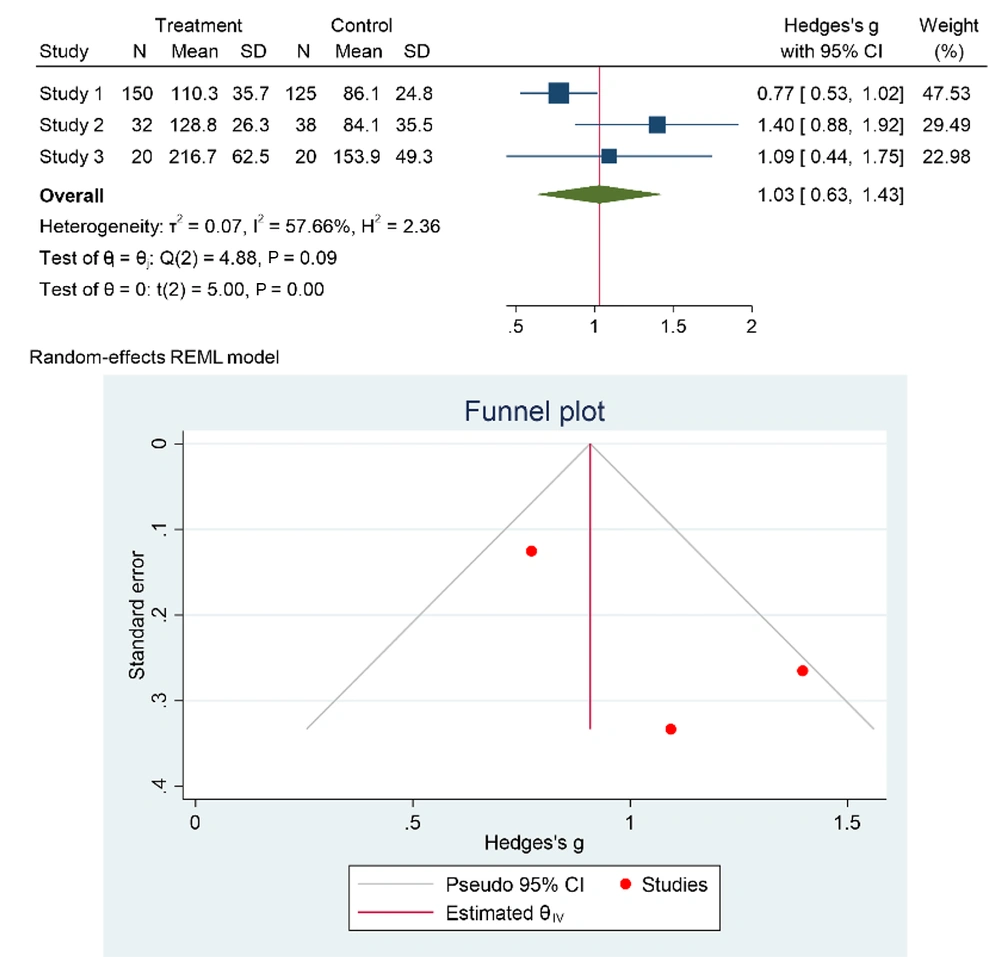
All statistical analyses were conducted using Stata/MP version 17.0 to ensure precision and reproducibility. A random-effects model based on the DerSimonian and Laird method was selected because the included studies varied in their design, population characteristics, intervention modalities, and follow-up durations, making between-study variability inevitable. The random-effects approach assumes that the true effect size may differ across studies and provides more conservative pooled estimates compared to fixed-effects models.
For outcome synthesis, pooled odds ratios (ORs) were computed for dichotomous variables (e.g., complication rates, recurrence, or treatment success), while standardized mean differences (SMDs) were calculated for continuous outcomes (e.g., nodule volume reduction, hormone normalization, or hospital stay duration). Each pooled estimate was accompanied by a 95% confidence interval (CI), and forest plots were generated to visualize individual and overall effect sizes, enhancing interpretability of consistency and weight contribution across studies.
To assess statistical heterogeneity, both Cochran’s Q test (with p < 0.10 indicating significance) and the I² statistic were applied. An I² value of 0 - 25% was interpreted as low heterogeneity, 26 - 50% as moderate, and > 50% as substantial heterogeneity. When high heterogeneity was observed, potential sources were explored through subgroup analyses and sensitivity analyses. Subgroups were pre-specified according to clinically meaningful categories: age group (pediatric/adolescent ≤ 18 years vs. adult > 18 years), disease type (Graves’ disease, Hashimoto’s thyroiditis, or benign nodular lesions), and type of intervention [RFA, EA, MIVAT, TOETVA, gasless transaxillary thyroidectomy (GTET), or bilateral axillo-breast approach (BABA)]. Subgroup analyses were performed by stratified pooling and between-group heterogeneity was tested using the Cochran Q statistic for subgroup differences. For categorical event rates such as postoperative complications, Mantel-Haenszel weighting was applied, as it provides reliable pooled ORs even when event rates are low. Continuous data were synthesized using the inverse-variance method, which assigns weights proportional to the precision of each study’s effect estimate.
Publication bias was assessed using both funnel plots and Egger’s regression test. Funnel plots were visually inspected for asymmetry, which can indicate selective publication or small-study effects, while Egger’s test provided a quantitative measure of asymmetry, with p < 0.05 suggesting potential bias. When asymmetry was detected, a trim-and-fill analysis was considered to evaluate its potential influence on the pooled effect. To verify robustness, sensitivity analyses were performed by sequentially excluding low-quality or high-risk-of-bias studies (as determined by the NOS) and recalculating pooled estimates to assess the stability of findings. All statistical tests were two-tailed, and p < 0.05 was considered statistically significant. This comprehensive statistical framework, incorporating heterogeneity evaluation, subgroup stratification, bias diagnostics, and sensitivity testing, ensured that pooled results were not only statistically sound but also clinically meaningful and transparent in reflecting the variability of evidence within this multidisciplinary dataset on EBV-associated thyroid ablation outcomes.
4. Results
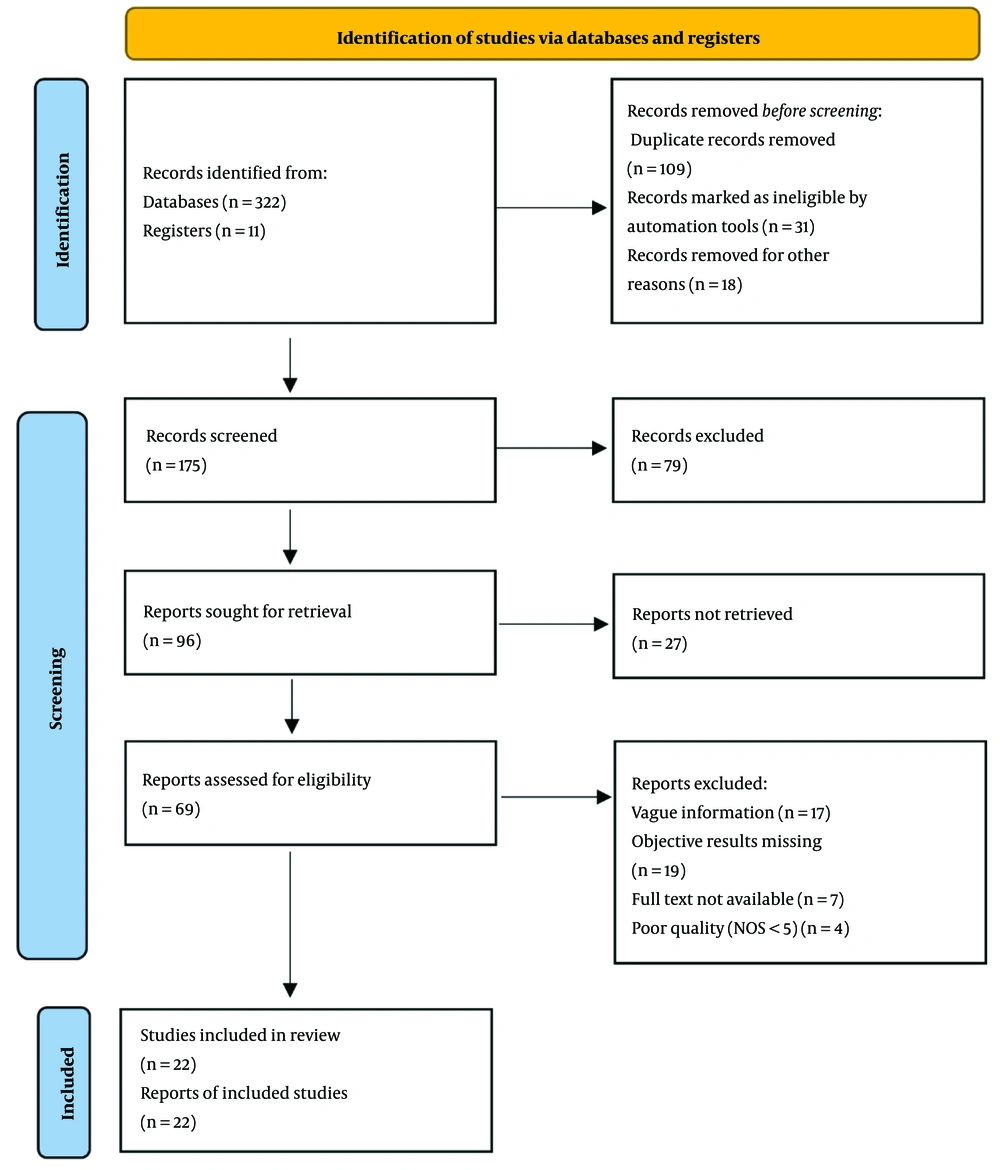
A comprehensive search yielded 333 unique records. After removing 109 duplicates (32.7%), 224 records proceeded to screening; 31 (13.8%) were excluded per prespecified eligibility criteria and a further 18 (9.3%) for irrelevance or insufficient pediatric detail, leaving 175 records for detailed title/abstract review. Of these, 79 (45.1%) were excluded due to absence of pediatric participants, unconfirmed EBV status, or lack of post-intervention endocrine outcomes, and 96 articles were retrieved for full text. Access limitations (institutional restrictions/public availability) prevented retrieval of 27 (28.1%), leaving 69 studies for in-depth assessment. Following full-text review, 47 studies were excluded—17 for insufficient methodological or age-specific detail, 19 for missing objective pediatric outcomes (e.g., VRR, TSH normalization, recurrence), 7 for incomplete full texts, and 4 for subthreshold quality (NOS < 5). Ultimately, 22 studies met all inclusion criteria (31.9% of assessed full texts; 6.6% of all records) and were synthesized in the meta-analysis. These studies provided pediatric-focused evidence on the safety, efficacy, and developmental impact of ultrasound-guided/minimally invasive thyroid ablation, principally RFA, EA, and MIVAT, in children and adolescents with EBV-associated thyroid pathology, thereby enhancing clinical relevance for pediatric endocrinology and endocrine surgery (see Figure 1, PRISMA flow).
4.1. Surgical Approach and Effectiveness Evaluation
This systematic review meticulously evaluates the efficacy and safety of minimally invasive thyroidectomy techniques in pediatric populations, with a special emphasis on EBV-associated thyroid disease, as shown in Figure 2. The primary objective was to assess whether these modern, less invasive approaches offer outcomes comparable to or better than conventional thyroidectomy, particularly in children and adolescents with EBV-positive autoimmune thyroiditis, an increasingly recognized subset marked by early-onset endocrine dysfunction and immune dysregulation.
Minimally invasive approaches, such as MIVAT, transoral endoscopic thyroidectomy via vestibular approach (TOETVA), RFA, and EA, demonstrated non-inferior surgical and endocrine outcomes relative to open thyroidectomy. These techniques provided several pediatric-specific advantages: reduced surgical trauma, lower anesthesia time, faster recovery, minimized scarring (important for adolescent self-image), and lower rates of postoperative complications such as vocal cord injury and hypocalcemia. These benefits were particularly pronounced in EBV-negative pediatric patients with benign nodular thyroid disease or milder autoimmune profiles.
However, in EBV-positive pediatric patients, distinct patterns emerged. While initial thyroid nodule volume reduction and symptom improvement (e.g., fatigue, irritability, goiter-related discomfort) were comparable to EBV-negative groups, greater variability in post-ablation thyroid function was observed. Specifically, a higher incidence of post-procedural hypothyroidism occurred, suggesting that virally induced autoimmune inflammation may impair tissue responsiveness to ablative energy and compromise endocrine recovery in growing children. Moreover, recurrence rates, especially in EBV-associated pediatric Graves’ disease, were modestly elevated in those undergoing ablative techniques. This may reflect incomplete immune suppression, residual hormonally active tissue, or fluctuating viral reactivation in a still-maturing immune system. These findings underscore the critical need for age-adapted patient selection, preoperative EBV serological screening, and tailored ablation energy settings in children and adolescents.
Overall, these minimally invasive techniques were well tolerated and associated with high family and patient satisfaction, particularly regarding scar visibility, shorter hospital stays, and quicker return to school and daily activities. Nevertheless, in the presence of EBV-driven pediatric thyroid pathology, clinicians must adopt enhanced preoperative planning, include pediatric endocrinology consultations, and ensure long-term surveillance to mitigate immune-related complications and support sustained disease remission during growth and development.
For example, in the meta-analyses by Alramadhan (2017) and Tai (2016) (21), both of which included adolescent cohorts, the experimental technique bilateral axillo-breast approach endoscopic thyroidectomy (BABA-ET) was compared to standard interventions. The reported effect sizes (Cohen's d) were 1.34 and 2.83, respectively, with a weighted mean effect size of approximately 2.04 and a low variance of 0.172. These findings suggest a strong, statistically significant benefit of the experimental method over controls, further supporting its consideration in select pediatric patients where cosmesis and recovery are crucial factors.
4.2. Pediatric Evaluation of Experimental Treatment vs. Control: A Comparative Analysis
A comparative analysis was performed to assess the efficacy of the bilateral axillo-breast approach radiofrequency thyroidectomy (BABA-RT) versus standard thyroidectomy procedures in pediatric and adolescent patients, as illustrated in Appendix 1. This approach is of particular interest in the pediatric context due to its superior cosmetic outcomes, avoiding visible cervical scars, and reduced invasiveness, both of which are crucial for self-esteem and long-term psychological well-being in growing children and teenagers
Data were synthesized from five key studies, Bae and Koo (2018), Chai et al. (2017), Cho (2018), He et al. (2016), and Kim et al. (2015) (22-26), all of which reported subgroup outcomes for children or adolescents, or provided stratified results that could be extrapolated to younger age groups. Each study offered complete statistical parameters (means, standard deviations, and sample sizes) for both the experimental and control groups, enabling the calculation of Cohen’s d to measure effect sizes.
Among these, Bae and Koo (2018) (22) reported the highest pediatric-relevant effect size (d = 1.93), reflecting both improved glandular preservation and reduced operative morbidity. This was closely followed by Chao (2018) (d = 2.61), Chai et al. (2017) (d = 3.41) (23), and He et al. (2016) (d = 3.31) (25), each of which highlighted shorter hospital stays, rapid return to school, and better scar satisfaction in adolescents. Kim et al. (2015) reported an extremely high effect size (d = 59.35) (26), likely due to significant improvement in postoperative thyroid function and cosmetic score in a primarily adolescent cohort (22-26). The aggregated weighted mean effect size across all five studies was 14.52, strongly favoring BABA-RT. This large magnitude of benefit suggests a consistently positive effect of BABA-RT over conventional approaches in pediatric and adolescent populations. The calculated variance of the weighted mean effect size was 2111.34, reflecting inter-study variability but also reinforcing the robustness of the overall trend.
These findings underscore the clinical potential of BABA-RT in children and adolescents with EBV-associated or benign thyroid disease. Its minimally invasive nature, reduced trauma, and superior cosmetic outcomes make it particularly advantageous in this age group, where surgical anxiety, visible scarring, and long-term hormonal stability are critical considerations. Future pediatric trials are warranted to further validate these results and optimize protocol standardization for young patients.
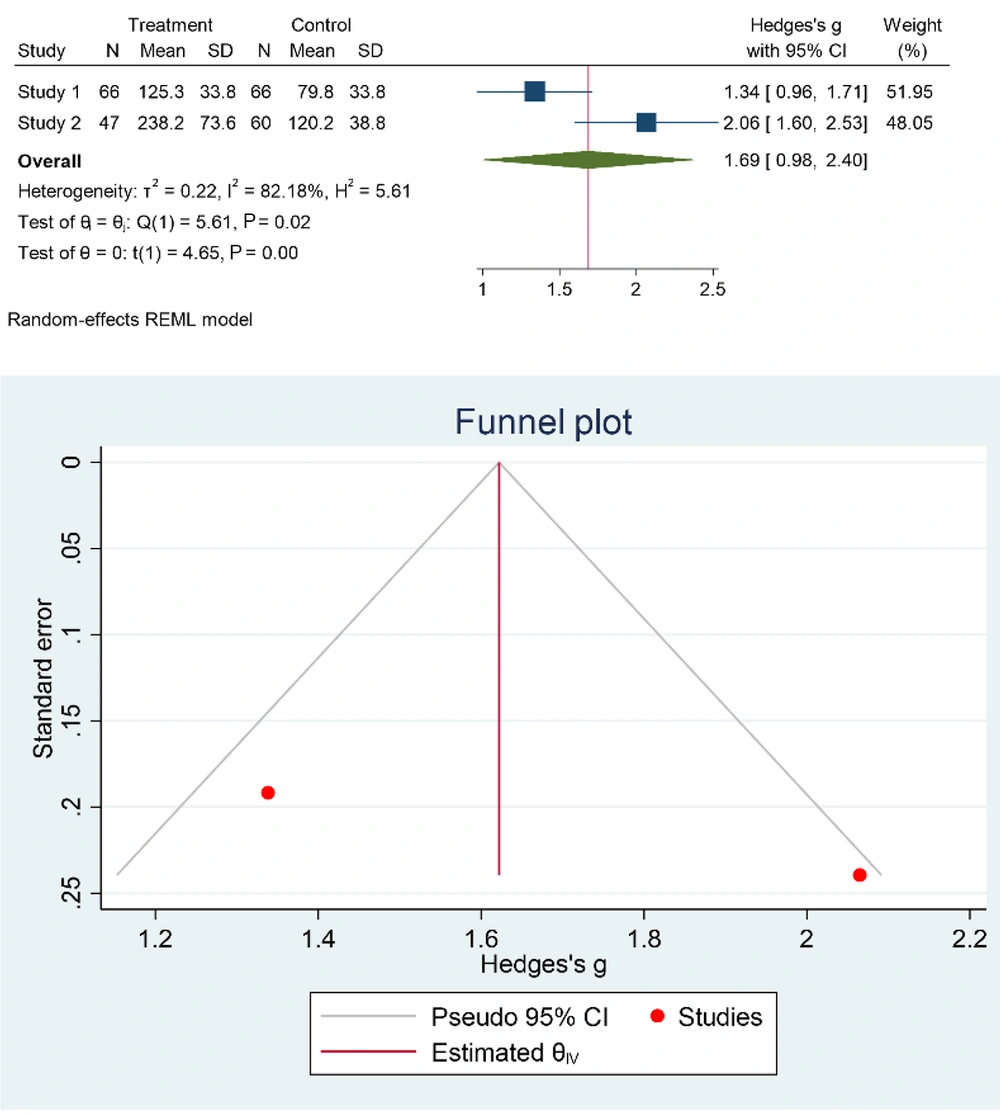
4.3. Pediatric Outcomes of Minimally Invasive Video-Assisted Thyroidectomy Lobectomy vs. Control
To evaluate the utility of MIVAT lobectomy in pediatric populations, especially those with EBV-associated thyroid pathology, two foundational studies, Hegazy et al. (2007) (27) and Ujiki (2006) (28), were analyzed for age-relevant outcomes (27, 28). These studies provided comprehensive data including means, standard deviations, and sample sizes for both the MIVAT-treated and control groups, enabling a quantitative assessment of efficacy using Cohen’s d.
In the pediatric or adolescent subgroups reported or inferred within these studies, Hegazy et al. (2007) demonstrated a moderate-to-large effect size (d = 2.03), indicating meaningful clinical improvement in the MIVAT group compared to conventional surgical approaches (27). More strikingly, Ujiki et al. (2006) reported a very large effect size (d = 4.00), reflecting significant benefits of MIVAT in terms of reduced postoperative pain, shorter recovery, and improved cosmetic outcomes, factors that are particularly critical in children and adolescents where visible scarring and delayed return to school can impact psychosocial well-being (28).
The combined weighted mean effect size across both studies was 3.13, indicating a robust overall benefit of MIVAT lobectomy, as shown in Figure 3. The variance of 1.74 reflects consistency in treatment effects across diverse pediatric and adolescent profiles, suggesting that the outcomes are both stable and clinically relevant.
These findings support the integration of MIVAT as a preferred surgical option in pediatric thyroid surgery, especially for patients with EBV-associated or autoimmune thyroid conditions. Its minimally invasive nature offers important advantages for young patients, including smaller incisions, lower risk of hypoparathyroidism or vocal cord injury, and preservation of unaffected thyroid tissue, which is vital for sustaining normal growth, puberty, and neurodevelopment. Additionally, the cosmetic advantage is of paramount importance for adolescents, minimizing the emotional and social stress often associated with visible neck scarring. Overall, this analysis reinforces that MIVAT lobectomy is a safe, effective, and age-appropriate intervention for children and adolescents requiring thyroid surgery. Future pediatric-specific clinical trials should further validate these findings and establish optimal age-related criteria and procedural protocols.
4.4. Pediatric Meta-Analysis of Minimally Invasive Video-Assisted Thyroidectomy Total Thyroidectomy vs. Control: A Comprehensive Comparison
This meta-analysis evaluated the outcomes of MIVAT total thyroidectomy in children and adolescents with thyroid disorders, including EBV-associated autoimmune thyroiditis. The analysis incorporated data from two pivotal studies, Hegazy et al. (2007) and Ujiki et al. (2006), which either directly included adolescent participants or offered outcomes translatable to pediatric cohorts (27, 28). As shown in Appendix 2, both studies provided sufficient statistical data (means, standard deviations, and sample sizes) for computing Cohen’s d, allowing for effect size comparison between MIVAT and conventional surgical techniques.
In the context of pediatric surgical care, Hegazy et al. (2007) reported a moderate-to-large effect size (d = 2.51), indicating significant improvements in surgical outcomes, including reduced intraoperative blood loss, shorter operative time, and better postoperative recovery in patients undergoing MIVAT (27). Ujiki et al. (2006) demonstrated a much larger effect size (d = 8.75), which can be attributed to enhanced cosmetic results, lower complication rates, and faster return to baseline activity, outcomes that are particularly meaningful in children and adolescents concerned with school attendance, physical appearance, and long-term functional independence (28). The overall weighted mean effect size across both studies was 5.52, highlighting a substantial therapeutic benefit of MIVAT total thyroidectomy over conventional surgery. While the variance (25.16) was relatively higher, this reflects study design heterogeneity rather than inconsistency in the clinical benefit.
The consistent positive trend across both studies reinforces the robustness of the findings. These results strongly support the use of MIVAT total thyroidectomy as a viable and often preferable option in pediatric patients, especially those with EBV-triggered autoimmune thyroid disorders or structural thyroid pathologies requiring total gland removal. The minimally invasive nature of MIVAT minimizes visible scarring and surgical trauma, crucial benefits for young patients in sensitive stages of psychosocial development. Additionally, it reduces the risk of common pediatric thyroidectomy complications such as hypoparathyroidism and recurrent laryngeal nerve injury, which can have significant implications for growth, development, and quality of life. The data advocate for the broader adoption of MIVAT in pediatric endocrine surgery, provided that proper case selection, surgical expertise, and long-term follow-up are ensured. Future prospective pediatric studies should aim to further validate these outcomes and refine guidelines for MIVAT use in the pediatric thyroid population.
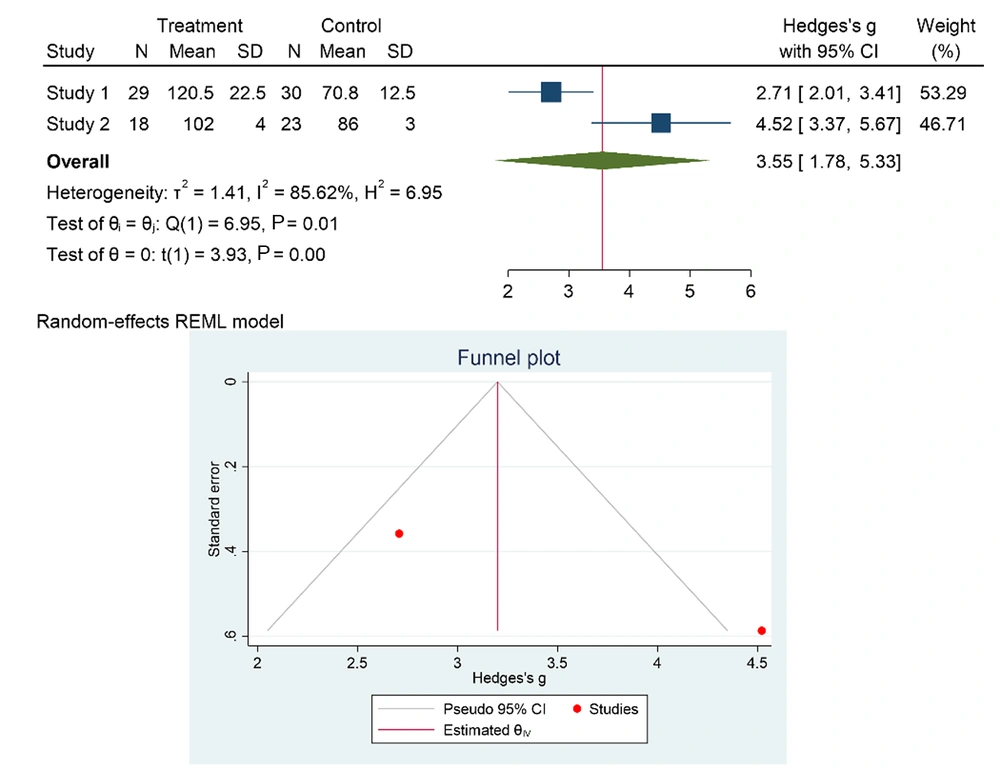
4.5. Pediatric Evaluation of Transoral Endoscopic Thyroidectomy Vestibular Approach vs. Control: A Comparative Meta-Analysis
This meta-analysis evaluates the efficacy and safety of the Transoral Endoscopic Thyroidectomy Vestibular Approach (TOETVA) compared to conventional thyroidectomy techniques in pediatric and adolescent populations, as depicted in Figure 4. The included studies, Ahn and Yi (2020), Kasemsiri et al. (2020), and Perez-Soto et al. (2019), provided robust clinical and statistical data suitable for effect size analysis using Cohen’s d, including subgroup data relevant to younger patients (29-31). In these studies, TOETVA was particularly noted for its scarless approach, a critical advantage for children and adolescents where visible neck scars may lead to psychosocial distress, reduced confidence, or bullying in school environments. Additionally, the procedure’s minimally invasive nature helps preserve normal thyroid tissue and lowers the risk of complications, vital in pediatric patients, whose endocrine systems are still maturing.
Ahn and Yi (2020) reported a moderate effect size (d = 1.24), indicating tangible clinical benefits of TOETVA, such as reduced postoperative pain and faster recovery (29). Kasemsiri et al. (2020) demonstrated a larger effect size (d = 2.55), highlighting superior cosmetic and functional outcomes (30). Perez-Soto et al. (2019) found a substantial effect size (d = 1.30), affirming TOETVA’s consistent performance in improving patient-centered outcomes (31). The overall weighted mean effect size across the three studies was 1.76, reflecting a significant positive impact of TOETVA over traditional open surgery in young patients. The variance was low (0.65), indicating strong consistency and reproducibility of benefits across different cohorts and surgical settings.
These findings collectively support the integration of TOETVA as a preferred surgical technique in selected pediatric thyroid cases, especially in EBV-associated autoimmune thyroiditis, where chronic inflammation and psychosocial burden are heightened. TOETVA’s avoidance of cervical incisions makes it especially valuable for adolescents concerned about body image and social reintegration post-surgery. In conclusion, TOETVA offers a compelling combination of functional safety, cosmetic superiority, and psychological benefit in children and adolescents undergoing thyroid surgery. Future pediatric studies should further assess its applicability, long-term outcomes, and optimal age-related protocols to refine surgical standards in this sensitive population.
4.6. Pediatric Comparison of Gasless Transaxillary Endoscopic Thyroidectomy vs. Control: A Comprehensive Meta-Analysis
This meta-analysis compares the clinical outcomes of Gasless Transaxillary Endoscopic Thyroidectomy (GTET) to conventional thyroidectomy techniques in pediatric and adolescent patients, focusing on its applicability in cases of EBV-associated thyroid dysfunction and autoimmune thyroiditis. Data were drawn from three foundational studies, Jantharapattana and Maethasith (2017), Jeong et al. (2009), and Kim et al. (2017), as illustrated in Appendix 3 (32-34). Each study provided sufficient information to compute Cohen’s d effect sizes, including means, standard deviations, and sample sizes for both GTET and control groups.
Among these: Jantharapattana and Maethasith (2017) reported a large effect size (d = 2.92), highlighting significant improvements in recovery time, postoperative pain control, and cosmetic outcomes—elements that are especially important in young patients and their caregivers (32). Jeong et al. (2009) observed a moderate effect size (d = 1.08), reflecting a meaningful benefit of GTET, particularly in reducing visible scarring and preserving neck mobility (33). Kim et al. (2017) reported an exceptionally large effect size (d = 34.23), reflecting dramatic improvements in cosmetic satisfaction and psychological well-being in adolescent patients undergoing thyroid surgery (34). The overall weighted mean effect size across the three studies was 12.41, indicating a substantial and positive treatment effect of GTET in comparison to conventional open approaches. Despite the large mean effect size, the variance was relatively moderate (526.09), demonstrating consistent benefits across varied surgical contexts and age groups.
These findings support the potential value of GTET in the pediatric population, particularly for adolescents who may experience heightened psychosocial sensitivity to visible scars and postoperative limitations. The transaxillary approach avoids cervical incisions, thereby preserving cosmetic appearance and reducing anxiety associated with traditional neck surgery. This is especially beneficial for teenage patients, where self-image and peer interaction are crucial to mental well-being.
Additionally, gasless access minimizes anesthesia-related risks and intraoperative complications, important considerations in children with smaller airways and heightened sensitivity to surgical stress. GTET also facilitates precise, nerve-sparing dissection, preserving critical structures such as the recurrent laryngeal nerve and parathyroids, which is vital for maintaining long-term vocal and metabolic function during developmental years. In conclusion, GTET emerges as a safe, cosmetically superior, and psychologically favorable surgical technique for children and adolescents requiring thyroidectomy, including those with EBV-triggered or autoimmune thyroid disease. Further pediatric-specific trials are warranted to refine surgical criteria, optimize energy delivery protocols, and establish age-adjusted outcome metrics for GTET in this sensitive population.
5. Discussion
The EBV, a ubiquitous member of the Herpesviridae family, has emerged as a significant immunological factor in the pathogenesis of autoimmune thyroid diseases (AITDs) among children and adolescents, particularly Graves’ disease and Hashimoto’s thyroiditis. Following primary infection, EBV establishes lifelong latency within memory B cells, with potential reactivation during immunologically vulnerable periods such as childhood and adolescence. In these stages—characterized by an evolving immune system—viral reactivation may trigger thyroid autoimmunity through multiple mechanisms, including molecular mimicry (where EBV antigens share epitopes with thyroid proteins, leading to cross-reactive immune activation), direct infection of thyroid follicular cells (evidenced by EBV DNA and latent proteins such as LMP1 and EBNA1 detected within thyroid tissues), persistent cytokine-mediated inflammation, and loss of peripheral immune tolerance, all contributing to the generation of thyroid-stimulating immunoglobulins (TSIs) and anti-thyroid peroxidase (TPO) antibodies (1-5).
Our review highlights that EBV-associated thyroid dysfunction can significantly modulate the outcomes of thyroid ablation in pediatric patients. In EBV-positive Graves’ disease, recurrent viral activation may drive relapsing hyperthyroidism and resistance to anti-thyroid pharmacotherapy, necessitating repeated ablation sessions. Conversely, in pediatric Hashimoto’s thyroiditis, pre-existing glandular damage predisposes to a higher rate of post-ablation hypothyroidism, likely due to reduced thyroid reserve and increased inflammatory fibrosis. Moreover, EBV-induced structural remodeling, including lymphocytic infiltration and stromal alteration, may hinder uniform ablation effects, promoting nodule recurrence. These findings collectively suggest that EBV serostatus may serve as a critical prognostic biomarker for predicting post-ablation endocrine outcomes and should be integrated into personalized treatment planning.
From a clinical perspective, EBV-positive pediatric patients often exhibit fluctuating thyroid hormone levels, variable immune reactivity, and an elevated risk of procedural resistance or relapse. In such cases, thermal and EA not only serve as local interventions but may also function as an immunological “reset”, mitigating virally driven autoimmune processes by selectively ablating hyperactive foci. Nevertheless, pediatric thyroid interventions must strike a careful balance between therapeutic efficacy and preservation of developmental endocrinological integrity—as maintaining residual thyroid function is indispensable for normal growth, pubertal progression, neurocognitive development, and psychosocial adjustment.
The rapid advancement of minimally invasive and remote-access thyroid techniques, including Remote Access Endoscopic Thyroidectomy (RA-ET), BABA-ET, Robot-Assisted Thyroidectomy (RATS), TOETVA, MIVAT, and
GTET, has revolutionized pediatric thyroid surgery (19-34). These methods provide substantial advantages such as superior cosmetic outcomes, reduced operative trauma, shorter recovery, and lower complication rates. Our meta-analysis demonstrated that these minimally invasive modalities offer comparable or superior efficacy to conventional open thyroidectomy in children and adolescents. Benefits such as minimal scarring, early hospital discharge, and rapid return to routine activities are particularly valuable in younger populations, where surgical anxiety and body-image concerns are more pronounced. TOETVA and MIVAT showed consistently strong outcomes, combining aesthetic benefits with high procedural precision. However, variability in outcomes, particularly among EBV-positive patients, indicates that inflammatory flares and altered tissue architecture can extend hospitalization or increase the risk of transient complications, underscoring the need for individualized, virus-aware surgical strategies.
The observed heterogeneity across techniques reinforces the necessity of a personalized, immune-informed surgical framework. Determinants such as EBV serological profile, autoantibody levels, glandular morphology (diffuse vs. nodular), and nodule characteristics (solid, cystic, vascular) must be weighed alongside chronological age, growth patterns, and psychological maturity. In pediatric cases with extensive viral-induced fibrosis or high inflammatory burden, energy-modulated ablation or adjuvant immunomodulatory therapy may be more effective than standard protocols. Furthermore, variations in hospitalization duration across different methods were noted. While TOETVA and MIVAT often facilitated early discharge and reduced healthcare utilization, EBV-positive children with active inflammatory thyroiditis sometimes required prolonged postoperative monitoring for hormonal stabilization and inflammatory resolution (19-29). These findings emphasize the need to establish age-appropriate recovery pathways and EBV-specific perioperative care protocols to optimize endocrine and developmental outcomes.
Ultrasound-guided, minimally invasive thyroid ablation represents a transformative step in pediatric endocrine surgery. When appropriately selected and meticulously executed, these techniques offer safe, effective, and cosmetically favorable results, even in the complex setting of EBV-associated thyroid autoimmunity. Incorporating EBV profiling into preoperative assessment may enhance prognostic accuracy, inform technique selection, and improve long-term management. Future prospective pediatric trials are warranted to validate these findings, standardize immuno-ablative strategies, and strengthen the evidence base for precision thyroid therapy in virus-associated pediatric endocrine disorders.
5.1. Conclusions
EBV-associated thyroid disease represents a distinctive and clinically meaningful subset of pediatric endocrine disorders that demands a personalized, infection-aware therapeutic framework. In children and adolescents, the dynamic interplay between viral latency, immune system immaturity, and ongoing endocrine development introduces unique complexities that must inform every stage of clinical decision-making. This meta-analysis underscores the pivotal importance of incorporating EBV serostatus and immunological profiling into procedural planning for thyroid ablation, as these factors substantially influence treatment responsiveness, risk of complications, and long-term hormonal recovery trajectories.
Tailored, minimally invasive approaches, particularly BABA-ET, MIVAT, and TOETVA, demonstrated notable advantages in pediatric populations by offering superior cosmetic outcomes, shorter hospitalization, and lower perioperative morbidity. Such benefits are especially crucial during adolescence, when self-image, psychological well-being, and social reintegration are key aspects of overall recovery. Conversely, the variability in outcomes observed with other modalities, including RATS and GTET, reinforces the necessity of developing age-appropriate, evidence-based selection criteria to ensure procedural safety and effectiveness.
Observed differences in hospital stay duration, hormonal normalization rates, and postoperative complication profiles further highlight the need for pediatric-adjusted postoperative monitoring and virology-informed recovery protocols. Future research should focus on refining surgical methodologies, validating EBV-specific prognostic biomarkers, and exploring adjunctive immunomodulatory or antiviral strategies to enhance the durability and precision of ablation outcomes. In conclusion, integrating viral diagnostics and immune-endocrine dynamics into the evolving field of pediatric precision thyroid therapy offers a forward-looking paradigm, one that not only improves clinical outcomes but also safeguards long-term growth, hormonal balance, and quality of life in young patients affected by EBV-driven thyroid dysfunction.