1. Background
In late December 2019, a cluster of unknown pneumonia cases was reported in Wuhan, China. Health researchers were unable to take prompt action to control the outbreak, so the disease quickly spread worldwide. On February 11, 2020, the World Health Organization officially named the disease caused by the 2019 novel coronavirus as coronavirus disease 2019 (COVID-19).The coronavirus study group (CSG) of the International Committee on Taxonomy of Viruses named it severe acute respiratory syndrome (SARS), and on February 23, 2020, 77,041 cases of COVID-19 infection were confirmed in China. This number of infections has surpassed the SARS outbreak in China in 2002 (1, 2). The disease has rapidly spread too many countries around the world in Asia, Europe, the Americas, Africa, and Australia (3, 4). As of February 17, 2023, COVID-19 has infected more than 680 million people worldwide and killed about 7 million. Iran is among the first countries to be affected by the disease after China and ranks first in the Eastern Mediterranean Region, causing almost 144,000 deaths so far. Symptoms of COVID-19 include fever, malaise, dry cough, headache, and breathlessness (5-7). Compared to SARS-CoV, this virus is more resistant to temperature (8, 9). Due to the contagiousness of the corona disease and the absence of specific proven therapeutic drugs, early diagnosis of this disease is of particular importance. Clinical hematology tests can determine the prognosis of patients and, accordingly, channelize patient support and treatment measures (10). Decreased white blood cell and lymphocyte counts, neutrophilia, thrombocytopenia, increased CRP, erythrocyte sedimentation rate, and procalcitonin are some laboratory anomalies that are commonly seen in most patients. Tests performed on patients with COVID-19 at the time of their first visit and diagnosis indicate the severity and status of the disease (11, 12). A number of markers have been identified that could potentially be used in risk stratification models to predict the status of patients with COVID-19 and identify those who may have pulmonary involvement or require intubation. In some studies, the increase or decrease in lymphocytes and platelets at the beginning of the disease or during its course has been different in patients with severe and mild forms, and even decreased in severe disease. In some studies, a number of inflammatory markers such as CRP, markers of cardiac and muscle damage, as well as liver and kidney function and coagulation factors have also been significantly increased in patients with severe and fatal coronavirus. Several biomarkers have been identified that can potentially contribute to risk stratification models for predicting severe and fatal cases of the coronavirus. In hospitalized patients with pulmonary involvement, physicians are advised to use number of white blood cells and lymphocytes, neutrophil, the level of thrombocytopenia, interleukin, and ferritin as markers of potential progression to critical illness. D-dimer levels are consistently reported to be higher in these patients, while their gradual increase during the course of the illness is particularly associated with worsening of the disease. Other coagulation abnormalities, such as prothrombin time and prolonged thrombin time, increase fibrin degradation products, with severe thrombocytopenia leading to life-threatening intravascular coagulation, which requires constant vigilance and rapid intervention.
2. Objectives
The objective of our study is to investigate concomitant underlying diseases and their relationship with disease severity and prognosis, to examine laboratory parameters and their relationship with disease severity, and ultimately to identify high-risk groups.
3. Methods
In order to estimate the minimum sample size, data from a similar study were used (13). The maximum sample size was related to the mean hemoglobin between the two mild and very severe groups, which was estimated to be about 142 in each group and 284 in total. However, considering that the information in the files may not be complete and there may be sample dropout, and also to increase the power of statistical tests, it was decided to take about 200 samples in each group and a total of 400 samples.
Z1 - β = 1.28,
In this study, the records of all COVID-19 patients who were hospitalized with a diagnosis of COVID-19 since February 2020 (March 1398) during the early stages of the COVID-19 outbreak in Iran were reviewed. The study protocol was approved by the Ethics Committee of Kermanshah University of Medical Sciences. Pharyngeal swabs were taken to screen for COVID-19 at the time of presentation and hospitalization to the hospital. Retrospective data including demographic variables (including CBC, CRP, ESR, LDH, PT, PTT, INR, D-dimer, fibrinogen), medical and clinical status of the patients (including O2-saturation, and cases including involvement in lung CT scan), treatment protocol used, clinical history of the patients in terms of comorbidities, and final outcome of the patients were extracted from electronic medical records. In this study, the impact of underlying diseases on the severity of COVID-19 disease and patient survival was investigated, as well as the relationship of laboratory parameters with the severity of COVID-19 disease and other aspects of COVID-19 disease. We used the chi-square test to compare the differences between 3 groups (non-survivors, recovered, and treated).
Inclusion criteria included age greater than or equal to 12 years, and hospitalization. The definition of patients with mild conditions included patients without pulmonary signs on imaging, the definition of moderate patients included patients with fever and respiratory symptoms and radiological evidence of pneumonia, and finally the definition of critical patients included patients with respiratory failure, septic shock, or multi-organ failure or dysfunction. The definition of unstable patients included patients with shortness of breath, respiratory rate above 30 breaths per minute, oxygen saturation less than 93%, and infiltration greater than 50% within 24 to 48 hours.
3.1. Statistical Analysis
The Kolmogorov-Smirnov test was used to examine the normality of quantitative data. The Mann-Whitney test will be used for non-normal quantitative variables and the independent t-test will be used for normal quantitative variables. Analysis of variance or, if necessary, Kruskal-Wallis will be used to determine the relationship between quantitative variables and disease severity. The chi-square test will be used to determine the relationship between qualitative variables and severity, death, pulmonary involvement, and saturation if the assumptions are met, and otherwise, the change of variable or Fisher's exact test will be used. The significance level in all tests will be 0.05.
4. Results
Four hundred COVID-19 patients were studied, and 184 women and 216 men were included in the data. The mean age of patients in this study was 61.91 years with a standard deviation (SD) of 16.192, with a minimum age of 23 and a maximum age of 94 years. 394 patients had the opportunity to undergo a lung CT scan, which was performed to assess the clinical status of the patient in terms of the degree of pulmonary involvement. In this study, it was possible to perform CT scans in 376 (95.4%) patients, while it was not possible to do so in 18 (4.6%) patients. In this study, PCR test for COVID-19 was performed for 379 patients. It was not performed in twenty-one patients due to lack of patient cooperation and concerns about the risk of bleeding. In 231 (60.9%) patients, the PCR test was positive. In 148 (39.1%) patients, it was negative. Out of 184 female patients, 15 patients left the ward with their own consent, 121 patients recovered, and 48 patients died. Out of 216 male patients, 145 patients recovered and were discharged. Twenty patients gave their consent and left the ward and 51 patients died. This difference was not statistically significant, meaning there was no difference between the recovered patients in the two groups (P = 0.813). We evaluated the relationship between gender and the clinical status of patients at the time of hospitalization using the chi-square test, which was not statistically significant (P = 0.268). In examining the relationship between gender and the values of quantitative variables (ESR, Hb, PLT, PT, PTT, INR), we used the Mann-Whitney test, which was statistically significant, and the average level of these variables was higher in male patients than in female patients. The results of quantitative traits by gender are shown in Table 1.
| Variables; Gender | Mean ± SD | P-Value |
|---|---|---|
| WBC | 0.867 | |
| F | 9.0437 ± 5.86560 | |
| M | 12.1019 ± 47.59787 | |
| Hb | 0.000 | |
| F | 12.3574 ± 1.91671 | |
| M | 14.1074 ± 8.71850 | |
| PLT | 0.000 | |
| F | 233.2247 ± 88.53359 | |
| M | 205.7171 ± 103.90645 | |
| ESR | 0.011 | |
| F | 50.2095 ± 26.36072 | |
| M | 41.9240 ± 20.31835 | |
| LDH | 0.761 | |
| F | 858.5433 ± 887.39438 | |
| M | 753.4546 ± 334.45171 | |
| PT | 0.022 | |
| F | 13.4440 ± 3.28507 | |
| M | 13.8435 ± 3.32304 | |
| PTT | 0.035 | |
| F | 35.3881 ± 12.51401 | |
| M | 36.7980 ± 11.93307 | |
| INR | 0.032 | |
| F | 1.1737 ± 0.70221 | |
| M | 1.1818 ± 0.52359 | |
| Fibrinogen | 0.551 | |
| F | 458.7324 ± 98.65466 | |
| M | 463.0693 ± 86.18727 | |
| Pulse oximeter | 0.579 | |
| F | 84.33 ± 13.033 | |
| M | 82.35 ± 15.91 |
Abbreviations: SD, standard deviation; F, female; M, male.
a The statistical test used is Mann-Whitney.
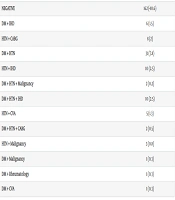
Comorbidities or medical history in patients with COVID-19 were shown in Table 2. The most common medical history was HTN, and the least common medical history was HTN + rheumatology + CKD, DM + malignancy, DM + rheumatology, and DM + CVA. The results saturation analysis showed that the mean of saturation was not significant according to the risk factors of DM, IHD, CVA, CABG, and rheumatology variables, but the mean of O2-saturation was significant according to the risk factors of HTN and malignancy. The results of saturation according to risk factors are shown in Table 3.
| Medical History | No. (%) |
|---|---|
| DM | 22 (5.5) |
| HTN | 73 (18.3) |
| IHD | 9 (2.3) |
| CVA | 3 (0.8) |
| CABG | 6 (1.5) |
| Malignancy | 13 (3.3) |
| Rheumatology | 5 (1.3) |
| Others | 18 (4.5) |
| CKD | 3 (0.8) |
| DM + CKD | 2 (0.5) |
| HTN + CKD | 2 (0.5) |
| HTN + Rheumatology + CKD | 1 (0.3) |
| NEGATIVE | 162 (40.6) |
| DM + IHD | 6 (1.5) |
| HTN + CABG | 8 (2) |
| DM + HTN | 31 (7.8) |
| HTN + IHD | 10 (2.5) |
| DM + HTN + Malignancy | 2 (0.2) |
| DM + HTN + IHD | 10 (2.5) |
| HTN + CVA | 5 (1.3) |
| DM + HTN + CABG | 2 (0.5) |
| HTN + Malignancy | 3 (0.8) |
| DM + Malignancy | 1 (0.3) |
| DM + Rheumatology | 1 (0.3) |
| DM + CVA | 1 (0.3) |
| Risk Factors; Disease | Mean ± SD O2-Saturation | P-Value |
|---|---|---|
| DM | 0.732 | |
| Yes | 84.68 ± 12.255 | |
| No | 83.11 ± 14.939 | |
| HTN | 0.000 | |
| Yes | 79.68 ± 17.087 | |
| No | 85.54 ± 12.243 | |
| IHD | 0.809 | |
| Yes | 84.97 ± 11.195 | |
| No | 83.27 ± 14.726 | |
| CVA | 0.194 | |
| Yes | 79.13 ± 13.410 | |
| No | 83.52 ± 14.462 | |
| CABG | 0.844 | |
| Yes | 85.20 ± 10.551 | |
| No | 83.35 ± 14.580 | |
| Malignancy | 0.002 | |
| Yes | 91.76 ± 4.944 | |
| No | 83.04 ± 14.617 | |
| Rheumatology | 0.372 | |
| Yes | 86.57 ± 12.095 | |
| No | 83.37 ± 14.485 |
Abbreviation: SD, standard deviation.
a The statistical test used is Mann-Whitney.
The association of DM, HTN, CVD, history of vascular surgery, rheumatic diseases, malignancy and other quantitative variables such as white blood cells, ESR, PLT, PT, PTT, INR, LDH, fibrinogen) with and without concomitant COVID-19 were examined. The results of quantitative traits on IHD risk factor are showed that the mean PT increased significantly in people with IHD, and there were no significant differences in other variables. The results of quantitative traits on CVA, GABC, malignancy, and rheumatology risk factors are showed that the mean differences between groups were not significant. The relationship between the oxygenation level by pulse oximetry in patients with COVID-19 and concurrent CVA, CABG, malignancy, rheumatology, myocardial ischemia and patients with COVID-19 and no history of comorbid was also examined, and this relationship and difference was not significant (0.194). The results of quantitative traits on DM risk factor showed that the mean WBC increased significantly in people who did not have DM, and there were no significant differences in other variables. A total of 145 patients out of 400 patients had HTN. Of these 145 patients, 83 patients (57.2%) recovered and were discharged. Twelve patients (8.3%) of this group of patients with concomitant HTN left the hospital with the patient's consent. The remaining 50 patients (34.5%) of this group of patients with concomitant HTN died. Concurrent analysis in the remaining 255 patients out of the total 400 patients who did not have HTN showed that 183 patients (71.8%) of this group of patients recovered and were discharged. Twenty-three patients (9%) of these patients left the hospital with the patient's consent. Forty-nine patients (19.2%) of the patients died. The difference between discharged and deceased patients in the two groups of hypertension with COVID and without HTN is statistically significant (0.003). Of the 145 patients with a history of HTN, the clinical condition was evaluated for stability and instability at the time of hospitalization, of which 119 patients (82.6%) had a stable condition. Twenty-five patients (17.4%) had unstable conditions. In comparison, in the remaining 254 patients of the 400 patients without HTN, 228 patients (89.8%) had stable conditions at the time of hospitalization, and 26 patients (10.2%) had unstable conditions. This difference was statistically significant (P = 0.041). The mean oxygen level in pulse oximetry in 255 patients without a history of HTN was (85.54, with a SD of 12.243) and in 145 patients with a history of HTN, the oxygenation level was (79.68, with a SD of 17.087), which was statistically significant. The results of quantitative traits on HTN risk factors are shown in Table 4. The results showed that there was a significant difference between Hb, LDH, PT, and INR variables, but there was no significant difference between other variables.
| Variables; HTN | Mean ± SD | P-Value |
|---|---|---|
| WBC | 0.591 | |
| Yes | 9.1063 ± 5.51770 | |
| No | 11.5988 ± 43.89311 | |
| Hb | 0.000 | |
| Yes | 13.3847 ± 10.63395 | |
| No | 13.2596 ± 2.12100 | |
| PLT | 0.808 | |
| Yes | 219.3427 ± 103.38456 | |
| No | 217.7090 ± 95.09046 | |
| ESR | 0.503 | |
| Yes | 44.7778 ± 24.44103 | |
| No | 46.3416 ± 23.21235 | |
| LDH | 0.006 | |
| Yes | 920.2324 ± 910.49533 | |
| No | 722.7042 ± 371.73860 | |
| PT | 0.004 | |
| Yes | 13.9007 ± 3.94519 | |
| No | 13.5184 ± 2.88158 | |
| PTT | 0.462 | |
| Yes | 36.8847 ± 15.41609 | |
| No | 35.7100 ± 9.93403 | |
| INR | 0.004 | |
| Yes | 1.2522 ± 0.84765 | |
| No | 1.1359 ± 0.42102 | |
| Fibrinogen | 0.919 | |
| Yes | 456.4211 ± 84.90456 | |
| No | 463.1638 ± 94.30975 |
Abbreviation: SD, standard deviation.
a The statistical test used is Mann-Whitney.
The group of patients with COVID-19 and a history of CVA were also examined and compared with the remaining patients with COVID-19 without a history of CVA. Those with CVA (9 patients) and those without CVA (391). Of the 9 patients with CVA, 5 patients died and 4 patients were alive. Compared to 391 patients without a history of CVA, 262 patients were alive and 35 patients were discharged with satisfaction, and 94 patients died, with a P-value of 0.045 by Fisher's test, which is a statistically significant difference.
The mean ± SD of oxygen level in all patients in pulse oximetry was 83.43 ± 14.439. The association of the mean oxygen level in all patients in pulse oximetry with other quantitative variables was examined using Spearman's correlation coefficient. Using Spearman's correlation coefficient, there was a weak and inverse correlation (-269) between white cell count and mean pulse oximetry oxygen level, which was statistically significant (P < 0.001). There was also a moderate and inverse correlation (-423) with LDH level, a weak and inverse correlation (-248) with PT level, a weak and inverse correlation (-131) with PTT level, and a weak and inverse correlation (-258) with INR level; and these relationships were significant (P = 0.000). The relationship between mean pulse oximetry oxygen level and D-dimer was also examined, which was statistically significant. The mean and SD of oxygen levels in pulse oximetry in the group of patients with positive D-dimer was 79.38 and in the group of patients with negative D-dimer was 87.32, which was statistically significant (0.009). The relationship between fibrinogen level, CRP and the mean oxygen level in direct pulse oximetry is very weak (-0.37) and is not statistically significant (P < 0.637 P < than 0.261). The relationship between the clinical status of patients who had unstable or stable conditions during hospitalization and the final outcome of these patients is as follows: 347 patients had stable conditions during hospitalization, of which 255 patients recovered and discharged, 32 patients left the hospital with satisfaction and 60 patients died. Fifty-one patients had unstable conditions during hospitalization, of which 10 patients recovered and discharged, 2 patients left the hospital with satisfaction and 39 patients died. The difference is statistically significant. (0.00). The mean saturation in D-dimer positive individuals was 17.916 ± 79.38 and in D-dimer negative individuals was 10.863 ± 87.32. The mean and SD of oxygen levels in pulse oximetry in the group of patients with positive D-dimer was 79.38 and in the group of patients with negative D-dimer was 87.32, which was statistically significant (0.009). The Mann-Whitney test determined that the difference in mean observed between the two D-dimer positive and D-dimer negative groups was significant (P = 0.009) and in D-dimer negative individuals, the mean saturation increased significantly.
5. Discussion
Laboratory parameters are not usually used for the diagnosis of COVID-19 due to their low sensitivity and specificity, but they are considered valuable prognostic indicators and provide useful information regarding the severity of the disease, the course of the disease, and the response to treatment. In this study, it was found that the mean difference in fibrinogen, WBC, and LDH between men and women was not significant; however, INR, PTT, PT, and Hb levels were significantly increased in men compared to women, and PLT and ESR levels were significantly increased in women compared to men. In a retrospective cohort study conducted on 219 COVID-19 patients, Elnaz Vafadar Moradi et al. reported that higher WBC counts were associated with an increased risk of one-month mortality (14). In addition, Ferrari et al. reported in a retrospective study that COVID-19 patients had significantly higher WBC counts than controls (15). In this study, the mean difference in WBC counts between men and women was not significant. Overall, the current evidence suggests that while WBC counts can be used as a predictor of severe COVID-19, the research findings are inconsistent and more studies are needed. The COVID-19 virus activates the immune system. The activation of the primary immune system, especially neutrophils triggers an inflammatory response followed by migration of monocytes and lymphocytes to the site of inflammation, leading to lymphopenia and monocytopenia. Elevated serum LDH levels are associated with poor prognosis in a variety of diseases, especially tumors and inflammation. The cytokine storm released by COVID-19 leads to alveolar damage and leakage of LDH into the circulation. In addition, the cytokine storm and systemic inflammatory response that characterizes severe COVID contributes to multi-organ damage and elevates LDH levels due to release from damaged tissues such as the liver, heart, kidneys, and skeletal muscle. In a retrospective observational study of 107 patients with COVID-19, Han et al. demonstrated that LDH is a good predictor for early detection of lung injury and severe cases (16). According to a meta-analysis by Gore et al., 52% of COVID-19 patients had elevated LDH levels (17). In this study, the difference in mean LDH between men and women was not significant. In a meta-analysis of 17 articles that examined inflammatory biomarkers in COVID-19 patients, Ghahramani et al. proved the relationship between higher ESR levels and Severity of the disease (18). In this study, the difference in mean ESR between men and women was significant, and it was significantly reduced in men, and as a result, the severity of the disease was less in men. A decrease in platelets is associated with a 3-fold increased risk of severe disease (19). The amount of platelets in men was significantly reduced compared to women, and as a result, it can be said that bone marrow cells are reduced more in men than in women, and platelets are more damaged in men, and platelets accumulate more in the lungs of men and are consumed more (20). In this study, the mean saturation was examined, and there was no significant difference between men and women. The relationship between the mean oxygen level in pulse oximetry and quantitative variables was also examined, using the Spearman correlation coefficient method. This analysis showed that in cases of low mean oxygen levels in patients, the mean levels of biochemical parameters such as LDH; PT, PTT, ENR, D-dimer, and the mean level of white blood cells are higher, which is significant with a P-value of 0.000. The relationship between the mean oxygen level in pulse oximetry and D-dimer was checked and it was determined that if the patient is positive, he is in an unstable condition in terms of oxygenation. The issue of thrombosis and the use of anticoagulation drugs should be given special attention. The issue of thrombosis and the use of anticoagulation drugs should be given special attention. In another study, it was shown that the stage of the disease is effective in the mortality of patients with cancer infected with the coronavirus, and an increase in mortality was not seen in patients with early-stage solid tumors, compared to the expected overall mortality. In some studies, patients with a history of COLD, DM, and CVA are at higher risk of death if they contract COVID-19. Some of the findings of this study are consistent with other studies. In this retrospective study, a number of important prognostic factors were identified that may increase the likelihood of clinical instability and death in patients with COVID-19. Patients with a history of HTN and patients with a history of CVA were at higher risk of death. Some of the findings of this study are consistent with other studies. The clinical conditions of the patients at the time of hospitalization were important and affected the final outcome of the patients (0.00), so that in patients whose initial conditions were unstable, the probability of death was is higher (0.00), so it is recommended to define newer hospitalization indications for COVID-19 patients. In the analysis of the difference in quantitative variables in the combination of diseases with COVID-19 and without these diseases with COVID-19, there were notable points. In the case of HTN with COVID-19, the mean level of PT and INR and LDH level is higher than in the case of COVID-19 without HTN, the mean hemoglobin level is lower, and with P-values of 0.004 and 0.04, 0.000, 0.04, respectively, this difference was significant. In the analysis of the combination of IHD with COVID-19, the average level of PT is higher than in the case of IHD without COVID-19, and with P-values of 0.004, respectively, this difference was significant. In cases of comorbidity with malignancy, only the mean Hb level was significantly lower with a P-value (0.024), which may be related to the underlying disease itself. Among patients who died of COVID-19, patients with a history of HTN and CVA had the highest frequency of death. One of the weaknesses of this study was the small number of samples in some disease groups, although it was possible to access a higher sample, which unfortunately was selected by our statistician from the beginning. Three of the authors of this article themselves visit COVID patients. During these visits, what they noticed was that overweight was present in a significant number of patients, especially women with hospitalized COVID-19, and was even associated with higher mortality. Due to the lack of attention to this issue from the beginning and the inability to examine (BMI), this factor cannot be discussed statistically. It was not possible to examine the economic and social status of the patients, or whether the patients had the possibility of using protective equipment permanently, or whether the patients had protective clothing before becoming infected. Given the higher mortality in patients with HTN, CVA, and patients with DM, these three cases should also be screened and specially controlled in infectious epidemics. Therefore, in addition to regular vaccination, wearing masks, appropriate social distancing, and maintaining hygiene are recommended for these people. People with underlying diseases should be monitored and screened.
5.1. Conclusions and Recommendations
Based on the findings of the study and similar studies, it is suggested that hematology markers, coagulation factors, and biochemical profiles, which are necessary initial measures to diagnose this disease, be used for early identification and determination of the course of the disease based on treatment protocols. Among patients who died from COVID-19, patients with a history of hypertension and cerebrovascular accidents had the highest frequency of death. We suggest that people with underlying diseases should be under active surveillance and frequent screening for COVID-19, and when these patients are infected with COVID-19, COVID-19 treatment guidelines should be implemented specifically.
5.2. Ethical Considerations
The studies involving human participants were reviewed and approved by the Kermanshah university ethics committee (Ref. no.4010704). The patients/participants provided their written informed consent to participate in this study.