1. Background
A common entrapment neuropathy involving median nerve in the upper limb, carpal tunnel syndrome (CTS) is reported in up to 19% of the general population (1, 2). Various risk and etiologic factors for CTS include mechanical industrial work, thyroid dysfunction, increasing age, chronic alcoholism, malignancy, pregnancy, female gender, and inflammatory rheumatic disease (2, 3). According to clinical examination and nerve conduction studies, it has been estimated that CTS is seen in one in every five person who complains of numbness, tingling and pain in the hands (1). On histopathology, non-inflammatory thickening and fibrosis of the sub-synovial connective tissue are the most characteristic findings of CTS (3, 4). Compression of median nerve may be caused from increasing age and trauma to synovium and flexor tendons in the carpal tunnel leading to degeneration and increased volume resulting in CTS (4). Type 2 diabetes mellitus (T2DM) is rapidly becoming a major health problem associated with life-threatening complications if not treated timely and adequately especially in Asian populations (5, 6). In the recent years, diabetes is being increasingly recognized to be a significant risk factor of hand-related disorders such as Dupuytren disease, trigger finger, diabetic cheiroarthropathy, ulnar nerve entrapment and median nerve entrapment (CTS) (7, 8). Timely diagnosis and management of diabetes is vital in preventing complications and morbidity (9). The risk and association between diabetes and CTS is being investigated (10). Prevalence of prediabetes in patients with CTS has been reported to be up to 60% (11). Rydberg et al. reported patients with CTS have a 35% increased risk of developing diabetes mellitus (12).
In China, Dong and Liu reported 39.3% patients of T2DM to suffer from CTS (13). Kwon et al. demonstrated CTS in 16.2% Korean patients of T2DM (14). From Pakistan, Furqan et al. reported CTS to be present in 13.2% patients with T2DM being associated with younger age, female gender and involving right hand more than the left (15). Our study addresses the limited understanding of CTS among patients with T2DM in Pakistan, particularly in Bahawalpur, where local data are scarce. It aims to determine the prevalence of CTS in this population and to explore its associations with demographic variables (age, gender), clinical factors (duration of diabetes, glycemic control), and other potential risk factors, including ethnic differences.
2. Objectives
By clarifying these relationships, the present study seeks to enhance early diagnosis and management of CTS in diabetic patients, ultimately contributing to improved clinical outcomes and reduced morbidity.
3. Methods
This cross-sectional study was conducted in the Department of Medicine at Bahawal Victoria Hospital, Quaid-e-Azam Medical College Bahawalpur Pakistan, between January and June 2024. The T2DM was identified based on an HbA1c level exceeding 7.0%, two random blood glucose readings of 200 mg/dL or higher, a prior diagnosis of T2DM and/or ongoing use of anti-hyperglycemic medication. The CTS was clinically diagnosed by symptoms of numbness, pain, tingling and burning affecting thumb, index, middle and ring fingers on history, along with positive Phalen’s and Tinel’s signs on examination. Phalen Sign is performed by flexion of wrists to 90 degrees for a duration of 60 seconds while maintaining elbows in extension and shoulders in neutral position; a positive sign in reported as elicitation of sensations of tingling or "pins and needles" in the median nerve distribution over thumb, index, middle and ring fingers, and indicates CTS (16). Tinel’s sign is done by percussion over the carpal tunnel through which median nerve passes just proximal to the wrist; the occurrence of symptoms in median nerve distribution is a positive sign and indicates CTS (16). In patients with positive clinical findings, CTS was confirmed by nerve conduction studies showing evidence of median nerve entrapment at the wrist. Diagnostic criteria included prolonged distal motor latency (> 4.0 ms), delayed sensory nerve conduction velocity (< 50 m/s) or a difference in sensory latency between the median and ulnar nerves of more than 0.5 ms across the wrist, consistent with entrapment neuropathy.
Patients with chronic or end-stage renal disease, coronary artery disease, chronic liver conditions, those undergoing hemodialysis or receiving steroid therapy for any reason, as well as patients with a history of hand or arm surgery or amputation, and pregnant women were excluded from the study. With a 5% margin of error and a 95% confidence level, the required sample size was calculated to be 177 participants using OpenEpi online calculator, based on an anticipated prevalence of CTS of 13.2% among T2DM patients (15). However to increase the strength of our study we included 210 patients. This study was carried out in alignment with the ethical principles outlined in the 1964 Declaration of Helsinki, as revised in 2000. Ethical approval and permission for data collection were secured from the head of department before the study began. Informed written consent was obtained from all participants prior to their enrollment. A total of 210 patients with type T2DM were included in the study using a non-probability consecutive sampling method.
Demographic data such as age, gender, and duration of diabetes were recorded, and each patient was clinically evaluated for glycemic control, including measurement of HbA1c levels. The patients were then evaluated for history regarding symptoms of CTS (numbness, pain, tingling and burning in thumb, index, middle and ring fingers) after which examination (Phalen’s and Tinel’s sign) was done. In patients with positive clinical findings, nerve conduction studies were done to confirm CTS as suggested by entrapment neuropathy of median nerve. All data were entered and analyzed using SPSS version 23. Categorical variables (gender, glycemic control status, presence of CTS) were summarized as frequencies and percentages, while quantitative variables (age, duration of diabetes, HbA1c levels) were expressed as mean ± standard deviation. To control for potential confounders, data were stratified, and associations were evaluated using chi-square or Fisher’s exact tests. Variables with a P-value < 0.05 were considered statistically significant. Binary logistic regression was applied to examine the relationship between clinical factors and CTS.
4. Results
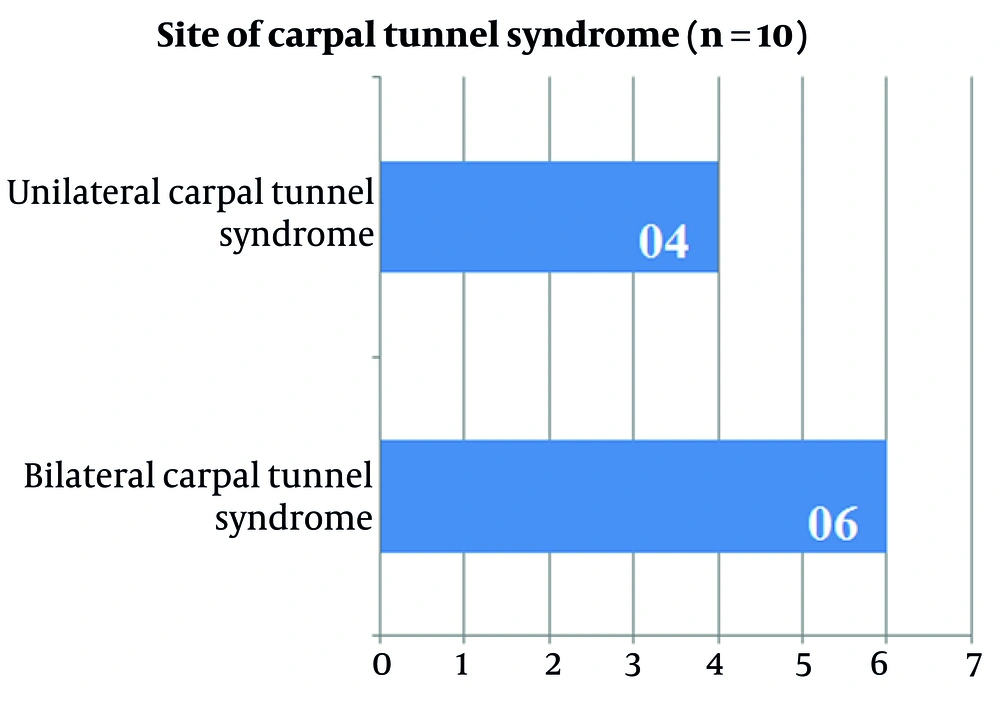
Mean age of the participants was 54.7 ± 14.5 years with 113 (53.8%) aged 55 years or above as shown in Table 1. Mean duration of diabetes was 6.7 ± 5.7 years with 126 (60.0%) having T2DM for 5 years or more. There was a female preponderance at 113 (53.8%). Mean HbA1c was 10.1 ± 2.4% and majority (n = 149, 71.0%) had poor diabetes control. The CTS was seen in 10 (4.8%) patients. Out of the 10 patients with CTS, 60 (60.0%) had bilateral involvement while 40 (40.0%) had unilateral involvement as presented in Figure 1. The CTS demonstrated no statistical association with gender (P = 0.347), age (P = 0.804), duration of diabetes (P = 1.000) or diabetes control (P = 0.727) as depicted in Table 2. Regression analysis examining the relationship between CTS and various patient factors also revealed no statistically significant associations as shown in Table 3.
| Demographic and Clinical Variables | Values |
|---|---|
| Gender | |
| Female | 113 (53.8) |
| Male | 97 (46.2) |
| Age (y) | |
| 54 or less | 97 (46.2) |
| 55 or more | 113 (53.8) |
| Duration of diabetes (y) | |
| 4 or less | 84 (40.0) |
| 5 or more | 126 (60.0) |
| Diabetes control | |
| Controlled/good | 61 (29.0) |
| Uncontrolled/poor | 149 (71.0) |
| CTS | |
| Present | 10 (4.8) |
| Absent | 200 (95.2) |
| Quantitative variables | |
| Mean age (y) | 54.7 ± 14.5 |
| Mean duration of disease (y) | 6.7 ± 5.7 |
| Mean HbA1c (%) | 10.1 ± 2.4 |
Abbreviation: CTS, carpal tunnel syndrome.
a Values are expressed as No. (%) or mean ± SD.
| Clinical Variables | CTS | P-Value | |
|---|---|---|---|
| Absent | Present | ||
| Gender | 0.347 | ||
| Female | 106 (93.8) | 70 (6.2) | |
| Male | 94 (96.9) | 30 (3.1) | |
| Age (y) | 0.804 | ||
| 54 or less | 92 (94.8) | 50 (5.2) | |
| 55 or more | 108 (95.6) | 50 (4.4) | |
| Duration of diabetes (y) | 1.000 | ||
| 4 or less | 80 (95.2) | 40 (4.8) | |
| 5 or more | 120 (95.2) | 60 (4.8) | |
| Diabetes control | 0.727 | ||
| Controlled/good | 59 (96.7) | 20 (3.3) | |
| Uncontrolled/poor | 141 (94.6) | 80 (5.4) | |
Abbreviation: CTS, carpal tunnel syndrome.
a Values are expressed as No. (%).
| Variables | Beta Coefficient (B) | S.E. | Wald | df | P-Value | Exp (B) | 95% CI for Exp (B) (Lower-Upper) |
|---|---|---|---|---|---|---|---|
| Gender | 0.710 | 0.706 | 1.010 | 1 | 0.315 | 2.034 | 0.509 - 8.118 |
| Age | -0.150 | 0.672 | 0.050 | 1 | 0.824 | 0.861 | 0.231 - 3.213 |
| Diabetes duration | -0.056 | 0.693 | 0.007 | 1 | 0.936 | 0.946 | 0.243 - 3.677 |
| Diabetes control | -0.477 | 0.819 | 0.340 | 1 | 0.560 | 0.621 | 0.125 - 3.087 |
5. Discussion
In China, Dong and Liu et al. reported 39.3% patients of T2DM to suffer from CTS which is significantly higher when compared to our study (13). In the present study, CTS was seen in 10 (4.8%) patients of T2DM out of which 60 patients had bilateral involvement while 40 patients had unilateral involvement. Kwon et al. and Furqan et al. reported CTS to be present in 16.2% and 13.2% patients with T2DM which are slightly higher than our findings (14, 15). Furqan et al. reported CTS to be associated with younger age, female gender and involving right hand more than the left (15). Kwon et al. also reported CTS to be more common in females but showed no association with diabetes itself (14). In the present study no statistical association of CTS was seen with patient’s gender (P = 0.347), age (P = 0.804), duration of diabetes (P = 1.000) or diabetes control (P = 0.727). The CTS was seen in 70 (6.2%) females compared to 30 (3.1%) males enrolled in the study. With regards to age, 50 (4.4%) patients of the 113 patients aged 55 years or more had CTS as compared to 50 (5.2%) patients out of 97 patients aged 54 years or younger. Of the 84 patients with diabetes duration of 4 years or less, 40 (4.8%) had CTS where as it was seen in 60 (4.8%) of the 126 patients with diabetes duration of 5 years or more. The CTS was present in 20 (3.3%) patients with good diabetes control compared to 80 (5.4%) with poor diabetes control. While this could suggest that these variables may not play a central role in CTS pathogenesis within this population, the absence of significant correlations might also be attributed to the relatively small number of CTS cases (n = 10), limiting the statistical power of subgroup analyses. Therefore, some true associations could have remained undetected due to the sample size. Overall, these results suggest that the factors examined may not play a crucial role in the development of CTS in this patient population, pointing to the need for further investigation into other potential risk factors or different demographic influences.
The management of CTS is decided according to patient preferences, severity of the symptoms and underlying etiologic risk factors (17). In patients with mild symptoms, splinting is employed as first-line (18). In patients with moderate symptoms, injecting corticosteroid into the carpal tunnel to provide symptom relief is indicated, but usually the effects are temporary (19). Surgical release to decompress the median nerve is reserved for patients who do not respond to conservative interventions (20, 21). However it should be noted that in patients of T2DM who undergo surgical release for CTS, there is an increased risk of infection if the blood sugar levels are not adequately controlled (22, 23). Therefore it is pertinent to target good glycemic control in addition to surgical release in such patients so that long-term benefits may be achieved.
This study was limited by its cross-sectional design, lack of a non-diabetic control group and the absence of CTS severity grading. Moreover, demographic and environmental factors unique to the study population, such as manual labor or ergonomic practices, were not assessed but may play a meaningful role in CTS prevalence. Since it was carried out at a single tertiary care center, the results may not be representative of the Pakistani population with T2DM. The use of non-probability consecutive sampling may have introduced selection bias, further limiting the generalizability of the findings to the broader diabetic population. Using an HbA1c cutoff of > 7.0% for diabetes diagnosis in our study may have excluded some patients, as current guidelines recommend 6.5%. While Phalen’s and Tinel’s signs were used as initial clinical screening tools, their sensitivity is less than 100%, so some cases of CTS without positive signs may have been missed. However, all clinically suspected cases were confirmed by nerve conduction studies to ensure diagnostic accuracy. Additionally, variations in healthcare access and regional factors could influence the prevalence of CTS in different settings. Therefore, we recommend that future research expand on our findings by including diverse populations across multiple institutions. Furthermore, the significance of early diagnosis and timely interventions cannot be overstated.
Timely lifestyle interventions, including improved diet and regular physical activity, combined with appropriate medication, play a crucial role in the effective management of both diabetes and CTS. Such strategies can help mitigate the risk of complications and improve overall patient outcomes. By prioritizing early detection and comprehensive care, we aim to reduce the morbidity and disability associated with these conditions, ultimately enhancing patients’ quality of life. Future studies should explore these interventions further to establish best practices in managing comorbidities in diabetic patients. Future research should aim to include larger, more diverse samples and explore additional risk factors such as occupation, Body Mass Index, diabetic neuropathy, and concurrent endocrine disorders. Multicenter studies with adequate statistical power will be essential to validate these findings and clarify the interplay between diabetes and CTS.
5.1. Conclusions
In our study, CTS was relatively uncommon. The lack of a significant association between CTS and factors such as gender, age, duration of diabetes and glycemic control suggests that other variables may influence its occurrence. Local factors including occupational exposure, lifestyle or genetic predisposition could contribute more prominently. Future large-scale, multicenter studies are needed to clarify these associations and improve early detection and management strategies.