1. Context
In recent years, telemedicine has emerged as a transformative force in the healthcare sector, enabling remote diagnosis, treatment, and monitoring of patients regardless of geographic limitations (1, 2). For nurses, these technologies enable early detection of patients' critical conditions, reduce medication errors, and support clinical decision-making; as a result, the quality of care and the efficiency of nursing processes are enhanced (2-4). As global healthcare systems face rising demands, resource shortages, and the need for timely interventions, intelligent telemedicine systems based on advanced technologies offer a promising solution (1, 5). The integration of big data and machine learning (ML) into telemedicine systems improves efficiency and diagnostic accuracy while enabling the delivery of personalized healthcare services (6, 7). Big data provides massive volumes of health-related information, while ML algorithms analyze this data to uncover hidden patterns, detect anomalies, and support clinical decision-making (7, 8). This combination not only improves the quality of care but also optimizes resource allocation and reduces operational costs (8, 9). Despite its great potential, the implementation of these technologies brings challenges such as data security, privacy concerns, and the need for robust infrastructure (10-12). This paper aims to explore the intersection of big data and ML in the context of intelligent telemedicine, outlining current advancements, practical applications, and existing barriers to adoption. The search strategy is detailed in Table 1.
| ML Use-Case | Nursing Roles | Patient Safety Impact | Cost and Outcome Benefits |
|---|---|---|---|
| Diabetes management | Remote monitoring, patient education, early intervention | Reduced hypoglycemia/hyperglycemia events | Lower emergency visits, improved glycemic control |
| Heart failure monitoring | Alert triage, care coordination, patient counseling | Early detection of decompensation, reduced readmissions | Decreased hospital stays, optimized medication use |
| COPD exacerbation prediction | Symptom monitoring, inhaler/O₂ adherence coaching | Reduced exacerbations and acute care visits | Lower hospitalization costs, improved patient QoL |
| Wound care assessment | Image capture, wound evaluation, care planning | Early infection detection, standardized wound care | Faster healing, fewer complications, reduced specialist visit |
| Alert fatigue management | Customize alert responses, prioritize clinical actions | Avoid missed critical alerts, reduce cognitive overload | Increased provider efficiency, reduced error rates |
| Personalized care plans | Use AI insights for tailored patient education and follow-up | Improved adherence and outcomes | Enhanced patient engagement, reduced complications |
Abbreviations: ML, machine learning; COPD, chronic obstructive pulmonary disease; AI, artificial intelligence.
2. Objectives
We decided to conduct a systematic and comprehensive investigation of the impact of big data analytics (BDA) and ML in telemedicine to support nursing practice, promote patient safety, and enhance care quality. The existing challenges and proposed solutions for the ethical and sustainable integration of these technologies into nursing clinical environments have also been discussed.
3. Methods
3.1. Machine Learning
3.1.1. Definitions, Algorithms, and Applications in Healthcare
Machine learning is a branch of artificial intelligence (AI) that focuses on the development of algorithms and statistical models that enable computers to learn from and make predictions or decisions based on data (13-22). Unlike traditional programming, where explicit instructions are given, ML systems identify patterns and improve their performance over time without being explicitly programmed for each task (22-24). There are three main types of ML (1, 25-27):
-Supervised learning: Where the algorithm learns from labeled training data (e.g., disease diagnosis based on patient records). Nurses play a key role by providing labeled data and clinical insights to train accurate algorithms.
-Unsupervised learning: Where the algorithm discovers hidden patterns in unlabeled data (e.g., clustering patients with similar symptoms). Nurses contribute by interpreting patterns and clusters identified by the algorithm to inform clinical decisions.
-Reinforcement learning: Where the system learns by receiving rewards or penalties based on its actions (used in optimizing treatment protocols). Nurses help guide algorithms by providing feedback on actions and outcomes to optimize clinical decision-making.
In healthcare, ML has a wide range of applications, including early disease detection, predictive analytics, personalized medicine, medical image analysis, drug discovery, and remote patient monitoring (28, 29). For example, ML models can analyze medical images to detect tumors with high accuracy, or predict patient deterioration in ICUs in real time (30, 31). The ability of ML to process large volumes of data and generate actionable insights makes it an essential tool in building intelligent, data-driven healthcare systems (32-34). Despite its transformative potential, challenges such as data quality, algorithm transparency, and ethical considerations must be carefully addressed to ensure safe and effective implementation in clinical settings (33, 35, 36).
3.2. The Role of Machine Learning in Telemedicine
In telemedicine, ML is applied in several key areas (19, 33, 36-40).
-Remote diagnosis: The ML models can analyze patient symptoms, images, or video data to assist healthcare providers in diagnosing conditions such as skin diseases, respiratory issues, or eye disorders via teleconsultation platforms.
-Predictive analytics: By identifying patterns in patient history and real-time data, ML can predict disease progression or the risk of complications, allowing for early intervention and proactive care.
-Virtual assistants and chatbots: The ML powers intelligent virtual agents that can handle initial consultations, triage symptoms, and provide guidance, improving efficiency and accessibility in telehealth systems.
-Personalized treatment plans: The ML enables the tailoring of treatment recommendations based on individual patient data, lifestyle, and genetics — even when care is delivered remotely.
Nurses face challenges, including ensuring data quality and maintaining patient safety.
3.3. Priority Clinical Use-Cases
3.3.1. Nursing Applications in Intelligent Telemedicine Systems
The integration of BDA and ML into telemedicine is not only transforming diagnosis and treatment but also redefining the role of nurses across various clinical settings. Below are key use-cases that illustrate how these technologies support nursing workflows, improve patient safety, and enhance care quality (3, 4, 41-47).
3.3.2. Diabetes Management
3.3.2.1. Use of Artificial Intelligence
Machine learning algorithms analyze continuous glucose monitoring (CGM) data, dietary inputs, and medication adherence to predict glycemic events (e.g., hypoglycemia):
Nursing role: Remote patient monitoring and education via telehealth platforms; early intervention based on predictive alerts from AI systems; counseling patients on lifestyle changes using personalized data.
Workflow effects: Reduction in emergency visits due to early detection; streamlined triage for high-risk patients, improved efficiency in follow-up scheduling and documentation.
3.3.3. Heart Failure Monitoring
3.3.3.1. Use of Artificial Intelligence
Predictive models use wearable device data (e.g., heart rate, weight, fluid retention) to anticipate decompensation episodes:
Nursing role: Monitoring dashboards and escalating alerts to cardiology teams; educating patients on signs/symptoms of worsening Heart Failure (HF); adjusting care plans collaboratively with physicians based on AI insights.
Workflow effects: Reduced readmission rates; enhanced coordination between home care and specialist teams; improved timeliness in medication adjustments.
3.3.4. Chronic Obstructive Pulmonary Disease
3.3.4.1. Use of Artificial Intelligence
ML algorithms analyze spirometry, oxygen saturation, and patient-reported symptoms to detect early signs of exacerbation:
Nursing role: Guiding patients on inhaler use and oxygen therapy adherence; remote coaching and breathing technique reinforcement; triaging patients based on AI-generated risk scores.
Workflow effects: Fewer acute care visits and hospitalizations; efficient use of teleconsultations for symptom escalation; empowerment of patients through data-informed self-care.
3.4. Inclusion Criteria
-Peer-reviewed articles in English and Persian between 2015 and 2025.
-Studies focusing on the application of big data and/or ML in telemedicine.
-Research explicitly addressing nursing practice, patient safety, or care quality.
-Empirical studies (qualitative, quantitative, or mixed methods), systematic reviews, or implementation reports.
3.5. Exclusion Criteria
-Editorials, opinion papers, and non-peer-reviewed sources.
-Studies not involving telemedicine or not integrating big data/ML.
-Articles with no mention of nursing or patient-centered outcome.
These technologies enable early detection of patients' critical conditions, reduce medication errors, and support clinical decision-making; as a result, the quality of care and the efficiency of nursing processes are enhanced.
4. Results
4.1. Common Machine Learning Algorithms for Telemedicine and Their Applications
4.1.1. Decision Tree
Classifying patient symptoms and recommending appropriate treatment paths in teleconsultation systems (48-50). Example: Determining whether a patient requires urgent in-person care or can be treated with medication remotely.
4.1.2. Random Forest
Predicting hospital readmission or risk of chronic conditions using historical health data (51, 52). Example: Forecasting kidney failure risk in diabetic patients via remote monitoring.
4.1.3. Support Vector Machine
Diagnosing diseases from medical images shared through telemedicine platforms (e.g., dermatology, radiology) (53-55). Example: Identifying potentially cancerous skin lesions from patient-uploaded images.
4.1.4. Artificial Neural Networks and Deep Neural Networks
Analyzing complex data such as ECG signals, heart sounds, or patient speech (33, 56). Example: Detecting arrhythmia from ECG data collected via wearable devices.
4.1.5. Naive Bayes
Classifying patient questions and providing automated responses via medical chatbots (57, 58). Example: Determining whether a patient’s question is about symptoms, medication, nutrition, or emergencies.
4.1.6. K-Nearest Neighbors
Suggesting similar treatments for patients with comparable medical histories and symptoms (59-61). Example: Recommending medication based on successful treatments in similar cases.
4.2. The Role of Big Data in Relation to Machine Learning Algorithms in Telemedicine
Big data serves as the backbone of ML-driven telemedicine systems. The ML algorithms require massive amounts of diverse, accurate, and well-structured data to function effectively — and big data naturally fulfills this need (41, 62). In telemedicine, data is collected from a wide range of sources including electronic health records (EHRs), medical imaging, physiological signals (such as ECG), wearable devices, patient-reported outcomes, chatbots, and prescription histories. This massive volume of information forms the foundation for training, validating, and optimizing ML models (63, 64). For example: Deep neural networks used for automated disease detection require millions of medical images to learn accurately (33, 58). Classification and decision-making models for predicting hospital admission or symptom categorization rely on both historical and real-time patient data (19, 61). In predictive analytics, big data helps identify early signs of chronic diseases like diabetes or HF (17, 42, 46).
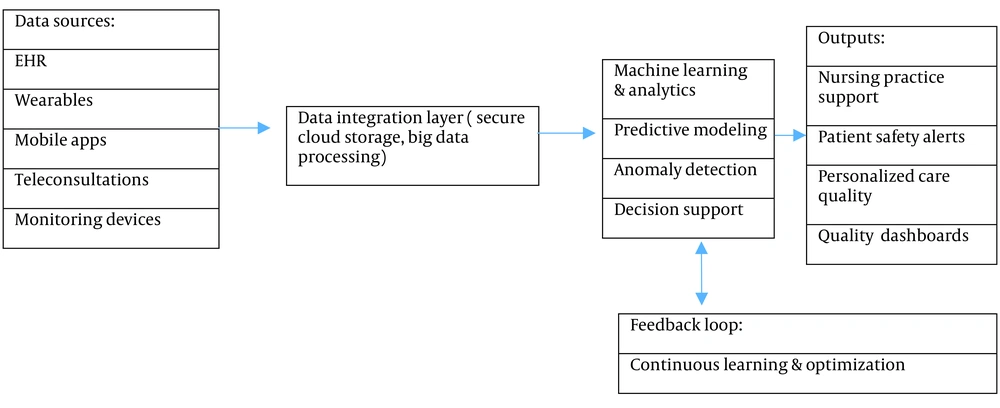
4.3. Integration of Machine Learning and Big Data in Telemedicine
The integration of ML and big data in telemedicine marks a significant step toward intelligent, efficient, and personalized healthcare delivery. Individually, ML enables systems to learn from data and make predictions or decisions, while big data provides access to vast and diverse health-related datasets. When combined, these technologies create powerful telemedicine systems capable of real-time analysis, predictive modeling, and decision support (63-65). For example, ML algorithms can process real-time data collected from wearable devices and remote monitoring tools, detecting anomalies or signs of health deterioration. Big data supplies the historical and contextual information that strengthens the accuracy and relevance of such predictions. Together, they support early diagnosis, personalized treatment plans, and proactive patient care — all delivered remotely (Table 1).
4.4. Ethics, Privacy, and Equity in Intelligent Telemedicine Systems
The integration of BDA and ML into telemedicine brings tremendous opportunities but also significant ethical, privacy, and equity challenges. Addressing these issues is essential to safeguard patient rights, ensure trust, and promote fair access to care (46, 63, 65).
4.4.1. Informed Consent
-Patients must be fully informed about the types of data collected, purposes of use, and potential risks and benefits associated with AI-driven telemedicine.
-Consent should be explicit, ongoing, and revisited especially when new analytics or ML models are introduced.
-Special attention is needed for vulnerable populations, including older adults, cognitively impaired patients, or those with limited digital literacy.
4.4.2. Data Minimization and Security
-Data collection should be limited to the minimum necessary to achieve clinical objectives, reducing unnecessary exposure.
-Robust cybersecurity measures (encryption, secure transmission, access controls) are mandatory to protect sensitive health information.
-Telemedicine platforms must comply with relevant regulations (e.g., HIPAA, GDPR) and undergo regular security audits.
5. Discussion
5.1. Workflow and Evaluation in Intelligent Telemedicine Systems
The successful deployment of BDA and ML in telemedicine critically depends on well-designed workflows and continuous evaluation to maximize patient safety, care quality, and operational efficiency (1, 33, 41, 42, 57).
5.1.1. Human-in-the-Loop
-HITL systems integrate human judgment with AI-driven decision-making to ensure contextual understanding, ethical oversight, and clinical validation.
-Nurses and clinicians review and interpret AI-generated alerts or recommendations before acting, maintaining ultimate responsibility.
-This collaboration enhances trust, reduces errors, and ensures AI serves as a support tool rather than a replacement for clinical expertise.
-This approach reinforces digital trust by keeping human oversight central to automated decision-making.
5.1.2. Alert Fatigue Management
-Excessive or irrelevant alerts can overwhelm healthcare providers, causing desensitization and increased risk of missing critical warnings.
-Strategies to manage alert fatigue include:
-Prioritizing alerts by severity and clinical relevance.
-Customizing alert thresholds based on patient profiles.
-Implementing tiered alert systems (e.g., informational, warning, critical).
-Integrating AI-driven filtering to reduce false positives.
-Effective management preserves provider attention and improves response times.
-Nurses play a crucial role in configuring and prioritizing AI-generated alerts to maintain clinical relevance.
5.1.3. Outcome Key Performance Indicators
Regular measurement of KPIs is essential to evaluate the impact of intelligent telemedicine on patient outcomes and workflow. Examples of relevant KPIs include:
-Reduction in hospital readmission rates.
-Time-to-intervention after AI alert.
-Patient adherence to care plans.
-Nurse workload and documentation time.
-Patient satisfaction and engagement scores.
-Continuous KPI monitoring enables iterative improvements in AI models and care protocols.
5.1.4. Cost-Benefit Perspective
5.1.4.1. Costs
Investments include technology infrastructure, training, ongoing maintenance, and potential workflow redesign. Early adopters may face upfront costs, but long-term savings arise from reduced complications and optimized resource use.
5.1.4.2. Benefits
Improved clinical outcomes, reduced emergency visits and hospitalizations, enhanced nursing efficiency, and higher patient satisfaction. Ultimately, a cost-benefit perspective grounded in long-term patient outcomes and system resilience will support equitable, scalable telemedicine adoption. Figure 1 illustrates the integrated workflow architecture, highlighting data inputs, analytical layers, and feedback mechanisms for continuous optimization.
This section highlights visual wound assessment with AI support, automated infection-risk alerts, and remote dressing protocols to improve monitoring, accessibility, and adherence. Nurses play a central role in patient education, triage, and translating remote assessments into clinical actions (Figure 1).
The cost-benefit analysis should report specific KPIs including 30-day readmission rate (%), number of avoided emergency visits per 100 patients, patient adherence rate (%), patient satisfaction score (Likert 1 - 5), and nursing workload (minutes per patient-day). Clearly defining these metrics and their measurement methods ensures reproducibility and comparability in clinical outcomes research.
Several future trends and opportunities are expected to shape this evolving field.
5.2. Enhanced Real-time Analytics
With the proliferation of Internet of Things (IoT) devices and wearable sensors, the volume of real-time health data will dramatically increase. The ML algorithms will evolve to process and analyze this data more efficiently, enabling instant diagnosis and timely intervention.
5.3. Explainable Artificial Intelligence
As ML models become more complex, there is growing emphasis on explainability to build trust among healthcare providers and patients. Explainable AI techniques will improve transparency, making it easier to understand, validate, and regulate ML-driven decisions in telemedicine
5.4. Conclusions
The convergence of ML and big data in telemedicine marks a pivotal evolution toward intelligent, patient-centered healthcare. By combining the predictive power of ML algorithms with the vast, diverse datasets provided by big data, telemedicine can move beyond basic remote consultations toward intelligent, personalized, and proactive medical care. This integration allows for early disease detection, real-time patient monitoring, personalized treatment plans, and data-driven clinical decision-making — all while expanding access to care in underserved regions. As technology continues to advance, this synergy is expected to further transform healthcare systems worldwide, improving efficiency, reducing costs, and enhancing patient outcomes. However, to fully realize these benefits, challenges related to data privacy, algorithm transparency, and infrastructure must be carefully addressed. Ultimately, the fusion of ML and big data paves the way for a smarter, more equitable, and adaptive global healthcare ecosystem — one that continuously learns and evolves with the needs of patients in the digital era.