1. Background
Sexuality is an integral part of individuals’ quality of life and interpersonal relationships (1) and has a significant influence on marital satisfaction (2). However, it remains a topic that is rarely discussed openly and is often neglected in both clinical and social contexts (3). Moreover, limited attention has been given to women’s sexual function and its stability or variation across different life stages (4). Sexual distress has also been found to be significantly associated with higher levels of depression (5). The prevalence of sexual dysfunction among women has been reported to range between 25% and 63%, and it is considerably higher among post-menopausal women (68 - 86.5%) (6). The prevalence of sexual problems in pre-menopausal and post-menopausal periods is on the rise. Increased life expectancy and the growth of the elderly population have presented the sexual health of menopausal women as an important issue. Sexual function alterations seen in the menopausal period and old age are affected by age, chronic diseases, drug use, hormonal changes, and socio-cultural characteristics (7). Recent evidence has also highlighted the impact of external and complementary factors — such as the COVID-19 pandemic and the use of herbal medicines — on female sexual health across different age groups (8, 9). These findings emphasize the multifactorial nature of female sexual function and the need for comprehensive evaluation in various contexts.
Therefore, old age and menopause transition have a huge adverse effect on sexuality, particularly sexual drive, excitement, orgasm, desire, and sexual movement (6). Female sexual dysfunction (FSD) is defined as any disorder that decreases sexual desire, subjective arousal, vaginal lubrication, and increases difficulty in achieving orgasm (10). Post-menopausal women are almost 2 times more likely to encounter sexual dysfunctionality than premenopausal women (11). However, limited data exist on how different domains of sexual function evolve over time. Previous studies have primarily been cohort-based or have reported prevalence rates among specific groups of women. To our knowledge, no study in Iran — where sexual topics remain largely taboo — has compared the sexual function of women in reproductive age with that of post-menopausal women (12). Therefore, the present study aimed to investigate differences in sexual function domains.
2. Objectives
The primary objective of this study was to compare sexual function between reproductive-aged and post-menopausal women. To provide a more detailed understanding of variations within reproductive-aged women, additional stratified analyses were performed across narrower age subgroups (21 - 27, 28 - 33, 34 - 39, and 40 - 45 years). These subgroup comparisons were considered secondary outcomes. In addition, the study aimed to determine and compare the frequency of sexual dysfunction between reproductive-aged and post-menopausal women.
3. Methods
3.1. Study Design
This cross-sectional analytical study was conducted in 2020 in southern Iran. Two different sample sizes were used in this study. For the comparative analysis of sexual function between reproductive-aged and post-menopausal women, considering the type 1 error of 0.05 and the power of 90%, and according to the study of Castelo-Branco et al. (13), who stated that sexual dysfunction was 38% in fertile women and 72% in post-menopausal women, the minimum sample size for each group was estimated to be 51 people. But in this study, a larger sample size was chosen to increase the power of the study (60 women in each group). Additionally, to assess the frequency and distribution of sexual dysfunction in a larger population, 404 women were included. The larger sample allowed for more precise estimates of proportions and percentages.
3.2. Recruitment of Participants
For the recruitment of midwives, the Vice-Chancellor for Research of Kerman University of Medical Sciences sent an official letter to the deputies of health and treatment in the selected provinces, requesting a list of telephone numbers of midwives working in clinical centers. The researcher then randomly contacted the listed numbers from each province. If the midwives agreed to participate, an email containing an invitation letter and detailed information about the research project was sent to them. All participants were informed that they could withdraw from the study at any time without any consequences. To ensure confidentiality, all collected data were anonymized. Informed consent was obtained electronically after providing an explanation of how to complete the online questionnaire. Finally, two midwives from each province were selected to assist in data collection.
A multi-stage sampling method was used in this study. In the first stage, random stratified sampling was applied to the southern half of the country, which includes six provinces: Bushehr, Khuzestan, Fars (Shiraz), Kerman, Kohgiluyeh and Boyer-Ahmad, and Hormozgan. Two cities were then randomly selected from each province. In the second stage, participants were recruited from comprehensive health service centers in each selected city using a quota sampling method proportional to the population size of the city and equally reproductive age and women of post-menopausal age. In the end, 199 reproductive age and 202 women of post-menopausal age were collected. In this way, 60 women from the reproductive age group and 60 women from the post-menopausal age group were randomly selected, making a total of 120 participants for comparison between the two groups. The random selection from each group provided an equal chance for all participants, ensuring the reliability and accuracy of the study results.
3.3. Inclusion and Exclusion Criteria
Inclusion criteria included married, sexually active women; women of reproductive age (18 - 45 years) with regular menstruation; and post-menopausal women who had undergone natural menopause (≥ 12 months since the last menstrual period), were not using hormone replacement therapy (HRT), and had no history of major chronic illnesses such as diabetes, cardiovascular disease, or psychiatric disorders. All participants were able to provide informed consent and respond to questionnaires. The menopausal women had undergone natural menopause, and one year had passed from their last period. Their uterus and ovaries were healthy, and they were not receiving HRT. They had no history of physical or mental illness affecting their quality of life, including diabetes, osteoarthritis, heart disease, and lung disease, and were able to answer questions.
3.4. Data Collection
The instruments used in this study were a personal information questionnaire, a sexual function questionnaire, and demographic variables. The personal information questionnaire consisted of questions about age, etc. Sexual function was measured using the Female Sexual Function Index (FSFI), which is a standardized, multidimensional self-report questionnaire developed by Rosen et al. (14) to assess sexual function over the past 4 weeks. It contains 19 items covering six domains: Sexual desire (2 items), arousal (4 items), lubrication (4 items), orgasm (3 items), satisfaction (3 items), and pain (3 items). The FSFI-19 is scored from 0 to 36, with lower scores indicating poorer sexual function, and an FSFI score below 26.55 is taken as an indicator of FSD. Higher scores on function domains represent better function; higher scores on the FSFI and dimensions represent better sexual function. The minimal clinically significant improvement of the FSFI was set at a > 20% increase, as was reported in a previous study (15). Fakhri et al. reported Cronbach’s alpha ≥ 0.70 for all subscales, confirming internal consistency (16). Babakhanian et al. (17) found test-retest reliability coefficients ranging from 0.76 to 0.89. Construct validity was confirmed by comparing mean FSFI scores between clinical and control groups (P < 0.001). In this study, self-administered questionnaires were used. For illiterate participants, face-to-face interviews were conducted by a trained female interviewer to maintain standardization.
3.5. Statistical Analysis
Data were analyzed using SPSS version 16. Quantitative variables were reported as standard deviation (SD). The Shapiro-Wilk test was used to assess normality and all datasets were normal. Student t-test, partial correlation coefficient, and Mann-Whitney test were used for data analysis, and a P-value of less than 0.05 was considered statistically significant. Multivariate logistic regression analysis was used to control for potential confounding factors such as age and marriage duration.
4. Results
The study included 60 women of reproductive age and 60 women of post-menopausal age. The mean ± SD age of the reproductive age women was 33.21 ± 6.51 years, and the youngest participant in this group was 19 and the oldest was 56. The mean ± SD age of post-menopausal women was 51.31 ± 6.08 years, and the youngest participant in this group was 41 and the oldest was 69 years old. The research subjects were all married women. The mean ± SD of period of marriage in the post-menopausal women was 23.29 ± 7.27 years and in the reproductive age women was 7.12 ± 5.81 years (P < 0.001).
As Table 1 shows, the dimensions of arousal, lubrication, orgasm, satisfaction, and pain, as well as the overall score of women's sexual function at reproductive age, were significantly higher than post-menopausal women. In other words, they had a higher average score. However, the scores of the two groups were significantly different only in the orgasm dimension. In our study, improvement in desire, orgasm, satisfaction, and total FSFI scores was not clinically significant.
| Variables | Mean ± SD | P-Value a | Study Population |
|---|---|---|---|
| Desire | 0.778 | 2.90 ± 1.16 | |
| Fertile | 2.93 ± 1.17 | ||
| Menopause | 2.87 ± 1.16 | ||
| Arousal | 0.099 | 3.12 ± 1.53 | |
| Fertile | 3.35 ± 1.42 | ||
| Menopause | 2.89 ± 1.61 | ||
| Lubrication | 0.222 | 3.58 ± 1.79 | |
| Fertile | 3.98 ± 1.43 | ||
| Menopause | 3.37 ± 1.79 | ||
| Orgasm | 0.043 b | 3.66 ± 1.60 | |
| Fertile | 3.96 ± 1.42 | ||
| Menopause | 3.42 ± 1.73 | ||
| Satisfaction | 0.109 | 4.27 ± 1.14 | |
| Fertile | 4.57 ± 1.16 | ||
| Menopause | 4.21 ± 1.28 | ||
| Pain | 0.424 | 4.21 ± 1.64 | |
| Fertile | 4.09 ± 1.44 | ||
| Menopause | 4.33 ± 1.82 | ||
| Total | 0.015 b | 22.04 ± 7.35 | |
| Fertile | 23.66 ± 6.14 | ||
| Menopause | 20.43 ± 8.12 |
Abbreviation: SD, standard deviation.
a Independent sample t-test.
b Significant P-value < 0.05.
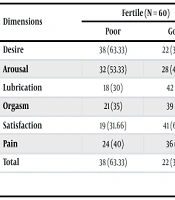
As can be seen in Table 2, in general, the total score for good sexual function is 36.66% in women of reproductive age and 23.33% in post-menopausal women, which is not significantly different between the two groups in all dimensions of sexual function.
| Dimensions | Fertile (N = 60) | Menopause (N = 60) | Both Groups | P-Value b | |||
|---|---|---|---|---|---|---|---|
| Poor | Good | Poor | Good | Poor | Good | ||
| Desire | 38 (63.33) | 22 (36.66) | 41 (68.33) | 19 (31.66) | 79 (65.83) | 41 (34.16) | 0.564 |
| Arousal | 32 (53.33) | 28 (46.66) | 34 (56.66) | 26 (43.33) | 66 (55) | 54 (45) | 0.137 |
| Lubrication | 18 (30) | 42 (70) | 22 (36.66) | 38 (63.34) | 40 (33.33) | 80 (66.67) | 0.604 |
| Orgasm | 21 (35) | 39 (65) | 26 (43.33) | 34 (56.66) | 47 (39.16) | 73 (60.83) | 0.350 |
| Satisfaction | 19 (31.66) | 41 (68.33) | 24 (40) | 36 (60) | 43 (35.83) | 77 (64.16) | 0.341 |
| Pain | 24 (40) | 36 (60) | 29 (48.33) | 41 (51.66) | 53 (44.16) | 67 (55.83) | 0.869 |
| Total | 38 (63.33) | 22 (36.66) | 46 (76.66) | 14 (23.33) | 84 (70) | 36 (30) | 0.195 |
a Values are expressed as No. (%).
b Chi-square test.
Results of multiple linear regression show that only the arousal variable has a significant difference between fertile and menopausal women, and fertile women have a better situation (Table 3).
| Groups | Fertile vs. Menopause (β) | SEβ | P-Value |
|---|---|---|---|
| Desire | -0.008 | 0.014 | 0.585 |
| Arousal | -0.041 | 0.020 | 0.052 |
| Lubrication | 0.026 | 0.021 | 0.229 |
| Orgasm | -0.024 | 0.025 | 0.345 |
| Satisfaction | -0.014 | 0.023 | 0.545 |
| Pain | -0.005 | 0.027 | 0.858 |
The results in the stratified age groups were reported in Table 4. Desire and arousal of women in the 21 - 27 age group were significantly better than the reference group (post-menopausal women). However, there was no significant difference between other age groups and other dimensions (Table 4).
| Age (y) | Desire | Arousal | Orgasmic | Pain |
|---|---|---|---|---|
| 15 - 20 | 1.72 (0.19 - 13.4) | 4.39 (0.27 - 47.31) | 1.38 (0.21 - 12.87) | 0.95 (0.14 - 6.54) |
| 21 - 27 | 3.52 (1.55 - 7.43) b | 3.22 (1.43 - 5.29) b | 1.59 (0.86 - 3.61) | 1.76 (0.95 - 3.78) |
| 28 - 33 | 1.41 (0.56 - 4.19) | 0.92 (0.42 - 2.64) | 0.79 (0.32 - 2.98) | 1.22 (0.54 - 2.87) |
| 34 - 39 | 0.77 (0.28 - 3.11) | 0.96 (0.41 - 2.37) | 0.77 (0.38 - 1.72) | 1.69 (0.63 - 5.73) |
| 40 - 45 | 1.19 (0.48 - 2.61) | 0.55 (0.20 - 1.75) | 0.84 (0.29 - 2.33) | 2.57 (0.72 - 7.81) |
| Post-menopaused | Ref | Ref | Ref | Ref |
a Values are expressed as odds ratio (95% CI).
b Significant level of 0.05.
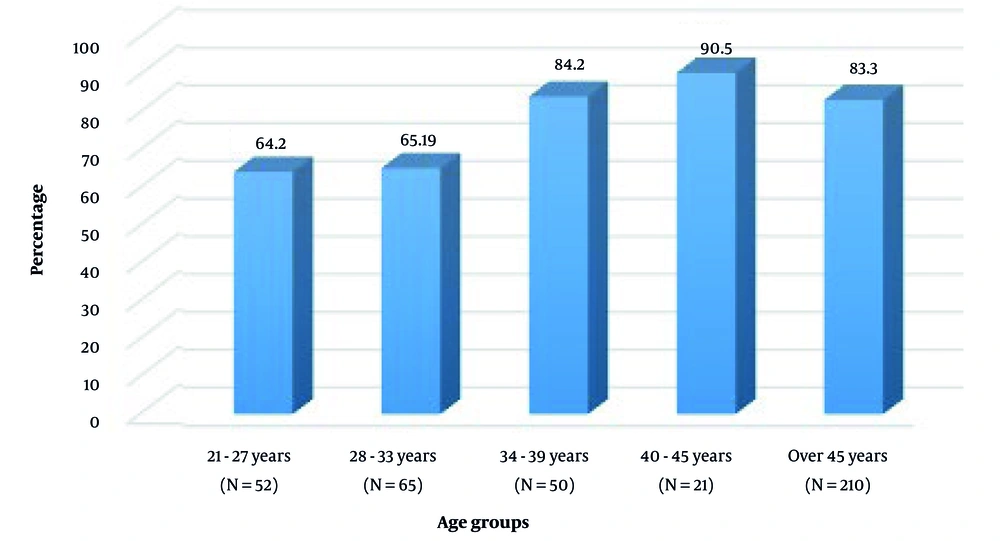
Table 5 shows the correlation of the dimensions of sexual function and the overall score with age and marriage duration in participants. In addition, the partial correlation to control the confounding factor age was computed. As the results show, the dimensions of arousal, lubrication, satisfaction, and total score of sexual function are inversely related to age and decrease with increasing age. Also, the total score and all dimensions of sexual performance showed an inverse relationship with the duration of marriage. Figure 1 shows the frequency of sexual dysfunction in different groups.
| Dimensions | Age | Marriage Duration | ||
|---|---|---|---|---|
| Correlation | P-Value | Correlation | P-Value | |
| Desire | -0.184 | 0.001 | -0.311 | < 0.001 |
| Arousal | -0.122 | < 0.001 | -0.296 | < 0.001 |
| Lubrication | -0.163 | 0.023 | -0.244 | 0.002 |
| Orgasm | -0.129 | 0.071 | -0.232 | 0.003 |
| Satisfaction | -0.201 | 0.019 | -0.76 | 0.003 |
| Pain | -0.132 | 0.272 | 0.287 | 0.002 |
| Total | -0.244 | 0.002 | -0.284 | < 0.001 |
The frequency study included 199 women of reproductive age and 203 women of post-menopausal age, with the mean ± SD of women of 32.9 ± 6.65 included. The frequency of low sexual function was 100% for women aged 15 - 20 years, 64.2% for women aged 21 - 27 years, 65.19% for women aged 28 - 33 years, 84.2% for women aged 34 - 39 years, and 90.5% for women aged 40 - 45 years. In menopausal women, this figure was 83.3% (Figure 1).
5. Discussion
In our study, the mean of sexual function scores based on FSFI is higher in reproductive age than post-menopausal age, but surprisingly when we look at these scores based on the clinical point of view as seen in Table 2, there is no significant difference between the two groups in all FSFI dimensions. The highest frequency of low sexual function was 90.5% in women aged 40 - 45, followed by 83.3% in postmenopausal women, and then 84.2% in those aged 34 - 39.
In our study, the frequency of low sexual function was calculated using the FSFI, a validated and reliable tool used to evaluate female sexual function in Iran and other countries (18). The frequency of low sexual function was 64.2% among women aged 21 - 27 years, 65.2% among those aged 28 - 33 years, 84.2% among those aged 34 - 39 years, and 90.5% among women aged 40 - 45 years. According to a meta-analysis of 11 studies involving 8,248 women conducted in Iran in 2016, the overall prevalence of FSD was 43.9% (95% CI: 35.0 - 52.8). Subgroup analysis based on Iranian cities showed wide variation in prevalence: 19.2% in Babol, 64.4% in Dezful, 45.2% in Sari, 64.0% in Tehran, 74.0% in Urmia, 46.2% in Ilam, and 31.5% in Bushehr (19). The frequency of low sexual function observed in our study was approximately twice as high as those reported in several previous Iranian surveys. This difference may be due to cultural attitudes toward sexuality, differences in sample characteristics, or the sensitivity of participants in self-reporting sexual issues.
Among postmenopausal women, the frequency of low sexual function was 83.3%. In comparison, the prevalence of sexual dysfunction among middle-aged women in Chile was 23.3%, 37.7%, 61.5%, 56.0%, and 53.6% among women aged 40 - 44, 45 - 49, 50 - 54, 55 - 59, and 60 - 64 years, respectively (13). Similarly, the prevalence of low sexual function was 43.4% in a study of 1,009 Turkish women aged over 20 years (20), and 51.2% among Chilean middle-aged women (18). The frequency of low sexual function in our sample was notably higher than that reported in most international studies. This may be partly explained by sociocultural barriers to open communication about sexual issues, limited access to sexual health education, and the absence of regular screening or counseling programs for women in Iran. Nevertheless, the overall pattern observed — showing a decline in sexual function with increasing age and menopausal status — is consistent with global evidence.
Although the frequency of sexual dysfunction was high in both groups, postmenopausal women showed a higher frequency compared with reproductive-aged women. Consistent with our findings, a study in China demonstrated that sexual dysfunction significantly increased during early and late postmenopausal stages compared with reproductive and perimenopausal stages. Importantly, a positive effect of HRT was observed in early postmenopause (21). Khani et al. conducted a systematic review and meta-analysis and concluded that the prevalence of FSD progressively increases from premenopause (22.7 - 72.2%) to perimenopause (37.3 - 78.2%) and post menopause (8.7 - 89.0%). This finding is consistent with our study, showing an overall trend of increased dysfunction with advancing reproductive stage. Although our prevalence rates in both reproductive-aged and postmenopausal women appear higher than the global averages reported in the review (22), the overall pattern aligns with existing evidence. Similarly, a study conducted in Istanbul on 1,009 women indicated that sexual dysfunction increased with age and menopause, with sexual desire and arousal being the most affected domains (20).
In our study, menopausal women never bothered to talk with their doctor. Compared to the studies mentioned above, a higher proportion of women in our study avoided visiting a doctor for sexual problems. Iranian midwives mention several reasons that hinder menopausal women from discussing their sexual problems. These include humiliation and a tendency to seek help from friends, relatives, and traditional healers rather than healthcare providers, ignorance of sexual problems, women’s attitude toward sexuality, and stereotypes (23). Almost all Iranian women with a history of ectopic pregnancy aged between 18 and 40 years did not talk about their sexual problem with their healthcare providers (24). Fifty percent of the survivors of allogeneic hematopoietic stem-cell transplantation never discussed their sexual problem with healthcare providers (25). Indonesian women did not openly discuss sexual problems and get embarrassed quickly when talking about sexuality (26). This highlights the fact that healthcare providers need to initiate talks with both healthy women and women with impaired sexual function. Nevertheless, Turkish women mentioned that health professionals never asked them about sexual health during their visits, and it is shameful and sinful for Turkish women to talk about their sexual (20). Among women with FSD, 1,423 (30.3%) never sought help, 1,339 (28.5%) considered looking for information on the Internet or in books, and 1,066 (22.7%) had visited a doctor (27).
The study data were collected using self-reported questionnaires. There are several biases in self-reported data such as selection biases, detection biases, and the difficulty of removing confounding factors (28). It is also important to evaluate the sexual function of husbands because it has a direct effect on the wife’s sexual function (7). These issues should be addressed in future studies. The quota sampling strategy was employed in some parts of sampling, which may lead to selection bias and its generalizability to the entire population is questionable. Random population sampling should be considered in future research.
The results of our studies exhibited that the odds ratio of desire and arousal disorders were 3.52 and 3.22 times higher in menopausal women than in women aged between 21-27 years, respectively. Similar to the present study, the odds ratio of total sexual dysfunction score was 10.65 times higher in menopausal women than in fertile women (7).
5.1. Conclusions
Although the frequency of sexual dysfunction was high in both groups, postmenopausal women showed a higher frequency compared with reproductive-aged women. Menopause is considered a risk factor for sexual problems. Menopausal women never seek help from health providers to address their sexual problems. Desire and arousal domains are the most common sexual problems followed by orgasm, lubrication, and satisfaction in fertile women. The most common sexual problem in menopausal women is the arousal domain followed by satisfaction, desire, orgasm, and lubrication, respectively. It is necessary for healthcare professionals to be sensitive and carefully evaluate all women, especially menopausal women, who are more prone to sexual problems. Health providers should place a premium on these issues.