1. Background
Antibiotic resistance and the emergence of antibiotic-resistant bacteria have become significant global health concerns in recent years, as highlighted by the World Health Organization (1). The lack of effective antibiotics against resistant species underscores the need for further practical and fundamental research on antibiotic resistance in this field (2). Staphylococcus aureus, in particular, has emerged as a major cause of severe infections in both hospital and community settings, leading to significant mortality and morbidity in patients (3). Hemodialysis patients are especially vulnerable to S. aureus infections, with an incidence rate twice that of other patient populations (4). This heightened susceptibility is attributed to their weakened immune systems and frequent vascular manipulations. Moreover, these patients can serve as potential sources of infection for others, further complicating infection control efforts in healthcare settings (3). The nose is the most common site of S. aureus colonization in hemodialysis patients. This nasal carriage can lead to infections and complications through hand contact or nasal manipulation, potentially contaminating catheters or other infection-prone sites (5, 6). The increasing resistance of hospital strains of S. aureus to various antibiotics has made choosing appropriate treatment a significant challenge (7). Understanding the microbial sensitivity patterns of S. aureus and cases of induced resistance is crucial for each medical center to develop effective treatment strategies (8). Vascular-related infections are significant factors in morbidity and mortality among immunocompromised and hemodialysis patients (9). Several factors increase the risk of nosocomial infections in these populations, including poor hygiene practices and the presence of hospital infection strain carriers among staff and hospitalized individuals (10, 11). The rapid increase in S. aureus resistance to antibiotics further complicates treatment options, necessitating ongoing research and surveillance (12, 13). Given the growing antibiotic resistance of hospital strains of S. aureus, this study aims to investigate the prevalence of nasal carriers of S. aureus and determine antibiotic resistance patterns in hemodialysis patients. Additionally, we examine the association between positive nasal cultures and catheter infections in previous years.
2. Objectives
This research seeks to provide valuable insights for improving patient care and infection control strategies in hemodialysis settings, ultimately contributing to the development of more effective prevention and treatment approaches for this vulnerable patient population.
3. Methods
This retrospective cohort study was conducted at Shahid Beheshti Hospital in Hamadan, Iran, from October 2022 to October 2023. All individuals meeting the inclusion criteria and referred to the dialysis ward of Shahid Beheshti Hospital in Hamadan were included via the census method, with a sample size of 176 individuals. The study population included all patients undergoing hemodialysis in the hemodialysis department during this period.
3.1. Inclusion and Exclusion Criteria
Inclusion criteria encompassed all kidney failure patients undergoing hemodialysis through fistula, graft, or catheter at Shahid Beheshti Hospital. Exclusion criteria were the use of antibiotics in the last three weeks and those who did not consent to sampling.
3.2. Sample Collection and Processing
Nasal swab samples were collected from hemodialysis patients using sterile swabs, following proper sampling protocols. Samples were transferred to the laboratory in appropriate transport media. Various tests, including catalase and coagulase tests, were employed to identify S. aureus. A positive D-test indicates that bacteria have inducible clindamycin resistance, meaning they appear susceptible to clindamycin initially but can become resistant when exposed to another antibiotic like erythromycin. This is shown in a lab test by a D-shaped blunting of the bacterial growth zone around the clindamycin disc, facing an erythromycin disc.
3.3. Antibiotic Susceptibility Testing
Antibiogram testing was performed using the disk diffusion method on Mueller-Hinton agar medium based on Clinical and Laboratory Standards Institute (CLSI) guidelines. The sensitivity and resistance of S. aureus to various antibiotics, including cefoxitin, penicillin, ampicillin, erythromycin, doxycycline, clindamycin, cefazolin, cotrimoxazole, ciprofloxacin, tetracycline, vancomycin, rifampin, and imipenem, were determined.
3.4. Sample Size and Ethical Considerations
The sample size was 176 patients, who were selected via the census method with regard to the inclusion criteria. Written informed consent was obtained from each participant before data collection. The study was approved by the Ethics Committee of Hamadan University of Medical Sciences (No: IR.UMSHA.REC.1401.670).
3.5. Data Collection
A comprehensive checklist was used to collect data, including:
- Demographic information (age, sex, education level, marital status, occupation, place of residence)
- Hemodialysis duration
- Hemoglobin level
- Recent hospitalization history
- Recent antibiotic use
- Underlying diseases (diabetes, hypertension, kidney stones, urological problems, glomerulonephritis, ADPKD, rheumatological diseases)
- Duration of underlying disease
- Opium use and smoking status
- Catheter type and insertion site
- Type of vascular access
- History of packed cell transfusion and blood product injection
- Complete blood count (CBC) and routine test results
- Dialysis adequacy
Data were collected through patient histories and medical files.
3.6. Statistical Analysis
Data analysis was performed using SPSS version 20 (IBM Corp., Armonk, NY). Descriptive statistics were presented as frequencies and percentages for categorical variables. The normality of continuous variables was assessed using the Shapiro-Wilk test. Group comparisons between positive culture and negative culture patients were conducted using Pearson's chi-square test for categorical variables including age, sex, marital status, education level, occupation, and place of residence. Univariate and multivariable logistic regression analyses were performed to identify risk factors associated with catheter infections. Results were expressed as odds ratios (OR) with 95% confidence intervals (CI). All statistical tests were two-tailed, and P-values < 0.05 were considered statistically significant.
4. Results
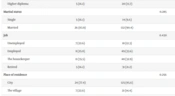
According to the findings of the present study, out of 31 patients with positive culture results, full details were presented in Table 1. There was no statistically significant association between the age, sex, marital status, and place of residence of patients and culture results.
| Variables | Positive Culture | Negative Culture | P-Value |
|---|---|---|---|
| Age (y) | 0.329 | ||
| Under 60 | 17 (54.8) | 66 (45.2) | |
| Over 60 | 14 (45.2) | 80 (54.8) | |
| Gender | 0.437 | ||
| Male | 17 (54.8) | 91 (62.3) | |
| Female | 14 (45.2) | 55 (37.7) | |
| Education | 0.947 | ||
| Illiterate | 7 (22.6) | 35 (24) | |
| Under diploma | 13 (41.9) | 59 (40.4) | |
| Diploma | 6 (19.4) | 32 (21.9) | |
| Higher diploma | 5 (16.1) | 20 (13.7) | |
| Marital status | 0.285 | ||
| Single | 5 (16.1) | 14 (9.6) | |
| Married | 26 (83.9) | 132 (90.4) | |
| Job | 0.430 | ||
| Unemployed | 7 (22.6) | 18 (12.3) | |
| Employed | 8 (25.8) | 49 (33.6) | |
| The housekeeper | 11 (35.5) | 48 (32.9) | |
| Retired | 5 (16.1) | 31 (21.2) | |
| Place of residence | 0.256 | ||
| City | 24 (77.4) | 125 (85.6) | |
| The village | 7 (22.6) | 21 (14.4) |
a Values are presented as No. (%).
Also, according to the results (Table 2), there was no significant association between the history of catheter infection and the result of S. aureus nasal culture (P = 0.4). However, there was a significant association with the number of catheter infections, as the frequency of catheter infection status = 0 versus frequency of catheter infection status >1 was associated with positive culture [n = 16 (48.4%) vs. 8 (25.8%), P = 0.009].
| Variables | Positive Culture (n = 31) | Negative Culture (n = 146) | P-Value |
|---|---|---|---|
| History of infection (yes) | 16 (51.6) | 47 (37.2) | 0.400 |
| Frequency | 0.009 | ||
| 0 | 15 (48.4) | 99 (67.8) | |
| 1 | 8 (25.8) | 36 (24.7) | |
| > 1 | 8 (25.8) | 11 (7.5) |
a Values are presented as No. (%).
According to Table 3, the risk of having a single catheter infection in those who have a positive culture is 46% higher, with P = 0.420, and the risk of having more than one catheter infection in those who have a positive nasal culture is 5 times higher, with OR = 4.80; CI = (1.66 – 13.85), P = 0.004. Independent of other variables, the risk of having two or more catheter infections in those who have a positive culture compared to those who have a negative culture is almost 6 times higher, with OR = 6.43; CI = (2.01 – 20.53), P = 0.002.
| Variables | Univariate OR (95% CI) | P-Value | Multivariable OR (95% CI) | P-Value |
|---|---|---|---|---|
| 1 infection | 1.46 (0.57 - 3.37) | 0.420 | 1.46 (0.55 - 3.87) | 0.440 |
| > 1 infections | 4.80 (1.66 - 13.85) | 0.004 | 6.43 (2.01 - 20.53) | 0.002 |
| Recent hospitalization (yes) | 0.20 (0.06 - 0.69) | 0.011 | 0.27 (0.04 - 1.76) | 0.171 |
| Recent antibiotic use (yes) | 0.27 (0.10 - 0.75) | 0.011 | 0.56 (0.11 - 2.79) | 0.492 |
The highest sensitivity was observed to rifampin, with 90.3% sensitivity. After that, cefotaxime and cefazolin, each with 80.6%, ranked next. The lowest sensitivity was observed to penicillin, with 12.9%. The highest resistance was observed to penicillin, with 87.1%, followed by ampicillin with 77.4%. Imipenem ranked third, with 74.2% resistance (Table 4).
| Antibiotic | Resistance | Sensitivity |
|---|---|---|
| Cefoxitin | 6 (19.4) | 25 (80.6) |
| Penicillin | 27 (87.1) | 4 (12.9) |
| Ampicillin | 24 (77.4) | 7 (22.6) |
| Erythromycin | 21 (67.7) | 10 (32.3) |
| Doxycycline | 10 (32.3) | 21 (67.7) |
| Clindamycin | 10 (32.3) | 21 (67.7) |
| Cefazolin | 6 (19.4) | 25 (80.6) |
| Co-trimoxazole | 8 (25.8) | 23 (74.2) |
| Ciprofloxacin | 9 (29) | 22 (71.0) |
| Tetracycline | 10 (32.3) | 21 (67.7) |
| Vancomycin | 7 (22.6) | 24 77.4 () |
| Rifampin | 3 (9.7) | 28 (90.3) |
| Imipenem | 23 (74.2) | 8 (25.8) |
a Values are presented as No. (%).
As the results of Table 5 show, 20 cases (64.6%) of S. aureus grown were sensitive to methicillin, 5 cases (16.1%) were resistant to methicillin, and 6 cases (19.3%) were D-Zone positive (inducible clindamycin resistance) despite resistance to erythromycin.
| Resistance Type | Values |
|---|---|
| MSSA | 20 (64.6) |
| MRSA | 5 (16.1) |
| D-Zone positive | 6 (19.3) |
Abbreviations: MSSA, methicillin-sensitive S. aureus; MRSA, methicillin resistant S. aureus.
a Values are presented as No. (%).
5. Discussion
In the current study, out of 176 hemodialysis patients, 31 patients (17.5%) were nasal carriers of S. aureus, of which 20 cases (64.6%) were methicillin-sensitive S. aureus (MSSA), 5 cases (16.1%) were resistant to methicillin (MRSA), and 6 cases (19.3%) were also D zone+ (positive ‘D-zone test’) (14). In addition, 7 cases (22.6%) were also resistant to vancomycin.
In Matthias Scheuch et al.'s study in 2019 in Greifswald, Germany (9), 43% of the studied hemodialysis patients became carriers of S. aureus during 25 months. Sixteen percent of the patients were constant carriers of S. aureus, which was close to the results of the current study. Among the samples isolated in this study, only two cases (2.32%) were MRSA, which means that the prevalence of MRSA is lower than in the present study (15).
In A. Price et al.'s study conducted in Birmingham in 2015 (11), 49% of patients had at least one positive nasal culture result within 18 months. The higher prevalence of S. aureus carriers in this study may be due to prospective examination and multiple culture tests of patients during 18 months. On the other hand, 10% of the positive samples were MRSA, which is less than the present study (16).
In the study of Sheikh al-Islami Ejraii et al. in Qom in 2018 (17), out of 244 hemodialysis patients, 61 (25%) were nasal carriers of S. aureus, of which 7 (11.5%) were resistant to methicillin and 52 (85.8%) were sensitive to methicillin (18). Compared to the present study, the number of carriers was higher (25%), but the number of methicillin-resistant MRSA cases (11.5%) was lower.
In addition, in the study by Kang et al. in Taiwan in 2012 (19), which was conducted on the nasal carriers of Staphylococcus in hemodialysis patients, out of 296 patients, 3.8% of the cases were MRSA, which is lower than the rate of methicillin-resistant cases in the current study (16.1%).
Also, in the study of Wang et al. in 2012 (20) in Taiwan, 541 hemodialysis patients were examined, of which 32 (5.9%) carried MRSA and 89 (16.5%) were carriers of MSSA, which was lower than the rate of methicillin-resistant cases in the present study (16.1%).
Also, in the study of Oumokhtar et al. (21) in Morocco in 2010 on 70 hemodialysis patients, 49.2% were nasal carriers of S. aureus and 3.3% were resistant to methicillin (MRSA), so the prevalence of methicillin-resistant cases in this study was lower than our study.
In the study by Tashakori et al. in 2014., among the dialysis patients of Rafsanjan Hospital, among the 61 hemodialysis patients, 12 (19.67%) were nasal carriers of S. aureus, 6.65% of which were MRSA and 13.11% of which were MSSA, which means the positive nasal carriers in this study were close to the results of the present study (22), but the amount of methicillin-resistant cases in this study was lower than that of the present study, which indicates the increase of bacterial resistance to methicillin in the present study.
According to the studies conducted, the prevalence of MRSA has increased over time and over the years. In fact, this issue can be considered a warning sign; therefore, the need to pay more attention to preventive measures is felt. Also, in the present study, the 22.6% resistance to vancomycin was reported, which was of great concern.
Similarly, in Zacharioudakis et al., vancomycin-resistant enterococci (VRE) have become important nosocomial pathogens causing outbreaks worldwide. Vancomycin-resistant enterococci colonization is prevalent in dialysis centers. Previous antibiotic use, in particular vancomycin, and recent hospitalization are important predicting factors of colonization, whereas the risk of VRE infection is significantly higher for colonized patients (4).
In the present study, the highest sensitivity to rifampin was observed with 90.3%, followed by cefotaxime and cefazolin, each with 80.6%. The rate of vancomycin sensitivity was also 77.4%. In the study of Sheikhul-Islami Ejraii et al. in Qom (17), the highest sensitivity to vancomycin was reported with 96.7%, followed by rifampin with 95.1%, which compared to the present study, the resistance to vancomycin increased by 19.3%. In Motamedifar et al.'s study (23), all strains were sensitive to vancomycin, and the rate of sensitivity to rifampin was in the next rank (97.3%), which was close to the results of the present study in terms of the rate of sensitivity to rifampin, but resistance to vancomycin increased by 22.6%.
In the present study, the highest resistance was to penicillin with 87.1% and amoxicillin with 77.4%. In the study of Akbarzadeh et al., there was 100% resistance to penicillin and amoxicillin in hemodialysis patients of Imam Khomeini Hospital in Tabriz, which is similar to the present study (24). In fact, this issue can be considered a warning and requires the design and implementation of preventive interventions.
In the current study, there was no significant association between the history of blood infection associated with catheter and the type of vascular access with the results of the nasal culture of the patients, which was in line with the results of Scheuch et al.'s study in 2019 in Greifswald, Germany (9). However, a significant association was observed between the positive culture result of the patients and the frequency of blood infection associated with the catheter (suffering more than once from the infection associated with the catheter). In A. Price's study conducted in Birmingham in 2015, patients who had not been eradicated of nasally colonized S. aureus were more likely to have S. aureus bacteremia than those who had been eradicated (11). The present results show the necessity of screening and nasal culture of hemodialysis patients with catheter-associated blood infection, which may make it possible to reduce the frequency and recurrence of catheter-related infections in dialysis patients through screening and identifying positive cases.
In the present study, there was a significant association between the history of being hospitalized in the last one month with the results of nasal cultures of patients and the use of antibiotics in the last month with the results of nasal cultures of patients, which was similar to the study by LU et al. in Taiwan in 2008 (13). In that study, there was a significant association between hospitalization in the last month and antibiotic treatment during this period with the percentage of methicillin-resistant S. aureus (MRSA) carrier (13); however, the result of the present study was contrary to the study of Sheikhul-Islami Ejraii et al. in Qom (17) and Diawara et al., which could be due to the type of antibiotics used in patients (25).
In the present study, there was no significant association between age and nasal carriage of S. aureus, which was consistent with the study of Sheikhul-Islami et al. (16, 17) and the study of Tashakkori et al. (22). In the study of Diawara et al. (25), younger patients were more nasal carriers of S. aureus, which contradicts the findings of the present study. It seems that this difference is due to the fact that young people were a small part of the statistical population of the present study.
Also, in the present study, 54.8% of cases of positive cultures were in men and 45.2% of cases were in women. Statistically, there was no significant association between gender and nasal transmission of S. aureus; this finding was in line with the results of the study by Sheikhul-Islami Ejraii (17), Diawara et al. (25), and Tashakkori (22).
In the present study, no statistically significant association was observed between education, occupation, marital status, and residence of patients with nasal carriage of S. aureus, which is similar to the study by Karimzadeh (26) and Askarian (27).
Therefore, according to the findings of the present study, it is recommended to perform screening, periodic cultures, and use of topical antibiotics to eradicate S. aureus colonized in the nose of hemodialysis patients to prevent multiple catheter infections. In addition, performing nasal culture in hemodialysis patients with catheter infection and eradication of nasal S. aureus is recommended to prevent re-infection and recurrence of catheter-related infection.
In addition, in order to find the prevalence of S. aureus resistance to methicillin, it is necessary to conduct additional analytical studies with a larger number of samples. Especially, retrospective cohort studies are necessary in order to obtain the prevalence in different departments of the hospital, the association with diseases, hospital personnel, treatment staff, and how S. aureus is transmitted.
One of the limitations of the current study was the retrospective cohort nature of the research method, which means causality cannot be inferred, so it is suggested to conduct interventional studies with a larger number of samples and using the cohort method. It is also suggested to conduct a prospective study to investigate the effect of eradicating S. aureus colonized in the nose on the possibility of catheter infection in hemodialysis patients and the frequency of catheter infection. The single-center setting and possible selection bias might be other limitations, for which performing such studies in multi-centers and using population data in place of control data in a case-control study are suggested. Finally, the wide confidence intervals for some odds ratios indicate limited precision in our effect estimates.
5.1. Conclusions
The prevalence of MRSA and antibiotic resistance in hemodialysis patients is concerning. Nasal S. aureus carriage was associated with an increased risk of recurrent catheter-related infections. Regular screening, decolonization, and appropriate antibiotic selection, along with infection control measures, may help reduce infection rates in this vulnerable population.