1. Background
War is detrimental to any country, with short- and long-term adverse effects. Technological advancements in the last century resulted in the production of mass-destruction weapons, including chemical weapons (1). The mental impact of chemical attacks is often more severe than physical injuries (2). Studies show that nearly one in four returning soldiers have severe mental problems (3), posing societal challenges. Extensive research has explored the relationship between war, stress, physical injuries, and mental health issues among veterans. Symptoms of mental disorders, such as memory malfunction, anxiety (4), depression (5), self-loathing, loneliness, mental health problems (6), stress, and dementia (4), have been confirmed in war victims (7). Irritability and aggression are common behavioral problems experienced by veterans due to their exposure to stressful and life-threatening situations (8). Aggression has various health consequences, including physical ailments, suicide, substance abuse, cardiovascular diseases (9), and chronic pain (10).
As a result of distressing thoughts and impulses, people with obsessive-compulsive disorder (OCD) engage in repetitive behaviors (11). It has been stated that 100 out of every 700 war veterans experience paranoia, which entails persistent distrust and complaints about others (12). Fear greatly disrupts life, causing a severe anxiety disorder (13). According to Fijtman et al. (14), veterans are more likely to be affected by severe mental diseases, such as bipolar disorder, and commit suicide. Even years after the Iran-Iraq war, post-traumatic stress disorder (PTSD) and poor mental health are still severe issues for veterans in Iran (15). With an emphasis on long-term impacts, this study attempts to compare the mental health and problems of veterans exposed to chemical weapons to healthy people.
Chemical agents in weapons cause death, permanent or temporary damage, weakness, paralysis, and disability, impacting executive functions (16). Executive functions include cognitive abilities, namely working memory, inhibitory control, cognitive flexibility, planning, reasoning, and problem-solving (17), mainly associated with the frontal lobe (18). Limited knowledge exists on the long-term effects of chemical gas exposure on human executive functions, but recent studies suggest various impacts (19, 20). Damage to the frontal lobe leads to executive dysfunction (21) and affects daily activities (22). Studies on attention deficit (23) have shown verbal memory deficits among veterans exposed to blast waves (24), non-verbal memory deficits in PTSD patients (25), and impaired future thinking (26), planning (27), attention (28), and cognitive flexibility in individuals with PTSD (29, 30). However, the effects of chemical weapons on veterans’ executive functions remain unexplored. This research compares memory, inhibitory control, attention, planning, decision-making, social cognition, and cognitive flexibility between veterans exposed to chemical weapons and healthy individuals, filling a crucial gap.
Research suggests that veterans’ mental and clinical problems emerge years later (15, 30). While comparing the mental state of veterans exposed to chemical weapons with healthy individuals may not directly impact treatment decisions, it can enhance screening, diagnosis, and intervention strategies. Furthermore, comparing mental conditions can enhance supportive care and rehabilitation efforts for veterans exposed to chemical weapons.
2. Objectives
Considering research gaps, theoretical importance, and the significance of veterans’ mental health, this study seeks to answer the question: How do mental disorders and executive functions differ between veterans exposed to chemical weapons and healthy individuals?
3. Methods
This case-control study was approved by the Research Ethics Committee of Aja University of Medical Sciences (IR.AJAUMS.REC.1400.232) following the World Medical Association’s (Declaration of Helsinki) code of ethics. The participants included veterans exposed to chemical weapons during the Iran-Iraq war and healthy individuals. Sampling was performed through the purposive sampling method. The inclusion criteria were: (1) Age of 44 - 55 years; (2) no prior exposure to warfare-related substances or metals (e.g., chemical agents and occupational exposure to lead and zinc); (3) not drinking alcohol; (4) not using supplemental antioxidants; (5) not taking psychoactive agents; (6) not being affected by chronic or mental illness; (7) not having received radiation therapy, surgery, or anesthesia within the previous year; and (8) ability to comprehend and respond to study-related questions. A total of 85 veterans who had been exposed to chemical weapons and an equal number (85 individuals) of healthy individuals matched in age, gender, education level, and residence were selected. After obtaining informed consent, both groups completed questionnaires on mental disorders (SCL-90), cognitive ability, and demographic information in one session.
The SCL-90 questionnaire, consisting of 90 questions, assessed mental symptoms and distinguished between healthy individuals and those with illness. Each question is rated on a 5-point scale, ranging from “none” to “severe.” The questionnaire comprises nine dimensions, including physical complaints, obsession-incontinence, depression, anxiety, aggression, morbid fear, paranoid thoughts, and psychosis, and entails seven additional questions. The internal reliability of the questionnaire was reported as 0.89, with the highest correlation coefficient for depression (0.95) and the lowest for psychosis (0.77). In Iran, Akhavan Obiri and Shoairi confirmed the scale’s reliability with a Cronbach’s alpha coefficient of 0.97 and a retest coefficient of 0.84. In the present study, the scale’s reliability was confirmed with Cronbach’s alpha coefficients of 0.71, 0.73, 0.73, 0.81, 0.77, 0.73, 0.75, 0.73, 0.74, and 0.76 for physical complaints, obsession-incontinence, sensitivity in mutual relationships, depression, anxiety, aggression, morbid fear, paranoid thoughts, psychosis, and the overall scale, respectively.
The cognitive ability scale developed by Nejati was used to measure executive functions. This 37-item questionnaire assesses memory, inhibitory control, selective attention, decision-making, planning, sustained attention, social cognition, and cognitive flexibility. Responses are given on a Likert scale from rarely, as 1, to almost always, as 4. Nejati reported a Cronbach’s alpha coefficient of 0.83 for this scale, and its validity and reliability were confirmed through significant Pearson’s correlation at a 0.01 level. The present study used Cronbach’s alpha coefficient to calculate the scale’s reliability. The subscales of memory (0.78), inhibitory control and selective attention (0.72), decision making (0.71), planning (0.79), sustained attention (0.74), social cognition (0.76), and cognitive flexibility (0.74) demonstrated reliability, with an overall Cronbach’s alpha of 0.90. The validity of the scale was also confirmed by five experts in the field of psychology.
The research data were analyzed using the SPSS statistical software (version 20.0, USA), employing multivariate analysis of variance (MANOVA) to examine the descriptive information.
4. Results
This study included one hundred and seventy male participants, all former army forces who had participated in the Iran-Iraq war. The participants had a mean age of 49.73±73.49 years, with a range of 44 - 55 years. Among the subjects, 45 individuals (26.5%) had education levels below a diploma, 77 (45.3%) had completed a diploma, and 48 (28.2%) had tertiary education. In terms of employment status, 14 participants (28.2%) were unemployed, 54 (31.8%) were employed as workers, 64 (37.6%) were self-employed, and 38 (22.4%) were retired.
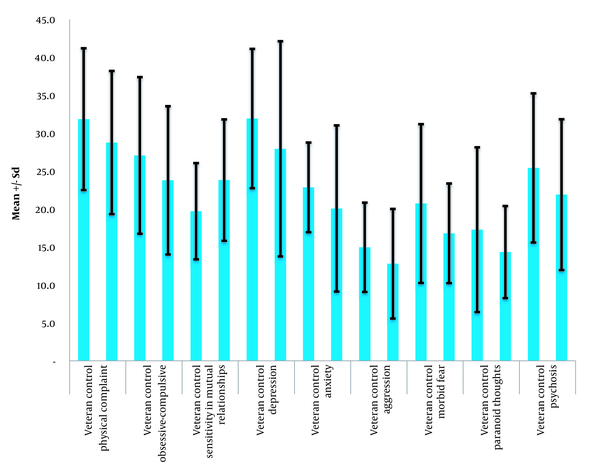
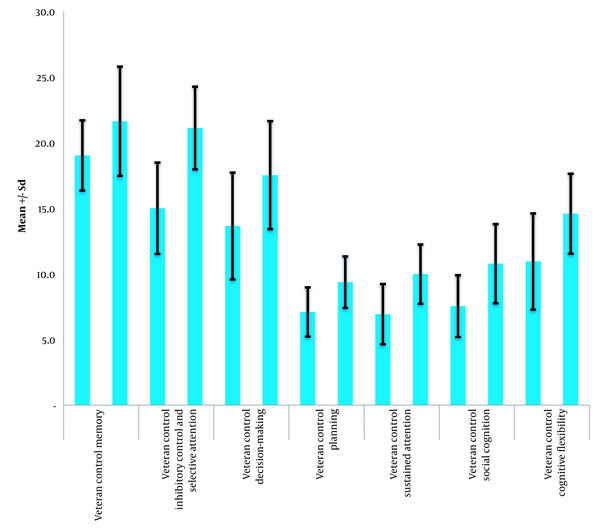
The results presented in Table 1 demonstrate that the average levels of mental disorders among veterans exposed to chemical weapons were higher than those of the general population across all subscales. The highest average score was observed for the depression component, while the lowest average score was associated with the aggression component. In addition, the findings in the table indicate that the average scores of executive brain functions are higher in the normal group than the veterans exposed to chemical weapons across all subscales. Within the group of veterans exposed to chemical weapons, the lowest average score was related to the sustained attention component, while the highest pertained to the memory component. These differences are represented in Figures 1 and 2.
| Group | Mean ± SD |
|---|---|
| Brain executive functions | |
| Memory | |
| Veteran | 19.02 ± 2.67 |
| Control | 21.62 ± 4.16 |
| Inhibitory Control and Selective Attention | |
| Veteran | 15.00 ± 3.47 |
| Control | 21.10 ± 3.15 |
| Decision-Making | |
| Veteran | 13.64 ± 4.06 |
| Control | 17.51 ± 4.11 |
| Planning | |
| Veteran | 7.09 ± 1.87 |
| Control | 9.36 ± 1.96 |
| Sustained Attention | |
| Veteran | 6.92 ± 2.29 |
| Control | 9.97 ± 2.25 |
| Social Cognition | |
| Veteran | 7.54 ± 2.35 |
| Control | 10.77 ± 3.02 |
| Cognitive Flexibility | |
| Veteran | 10.94 ± 3.66 |
| Control | 14.57 ± 3.04 |
| Mental disorders | |
| Physical complaint | |
| Veteran | 31.82 ± 9.33 |
| Control | 28.74 ± 9.42 |
| Obsessive-Compulsive | |
| Veteran | 27.04 ± 10.31 |
| Control | 23.76 ± 9.76 |
| Sensitivity in Mutual Relationships | |
| Veteran | 23.80 ± 8.00 |
| Control | 19.69 ± 6.34 |
| Depression | |
| Veteran | 31.90 ± 9.18 |
| Control | 27.91 ± 14.17 |
| Anxiety | |
| Veteran | 23.83 ± 2.91 |
| Control | 20.05 ± 10.95 |
| Aggression | |
| Veteran | 14.94 ± 5.88 |
| Control | 12.77 ± 7.22 |
| Morbid fear | |
| Veteran | 17.08 ± 4.88 |
| Control | 16.68 ± 6.58 |
| Paranoid thoughts | |
| Veteran | 17.27 ± 10.85 |
| Control | 14.31 ± 6.07 |
| Psychosis | |
| Veteran | 25.4 ± 9.82 |
| Control | 21.88 ± 9.93 |
Descriptive Indices of Brain Executive Functions and Mental Disorders separated by Group (n = 85 in Each Group)
Levene’s test did not reveal a significant difference in the homogeneity of variance between the two groups (veterans exposed to chemical weapons and the general population) (P > 0.05). Moreover, the results of the Kolmogorov-Smirnov test indicated the normal distribution of the scores (P > 0.05). Therefore, MANOVA was employed to examine the differences between the two groups in terms of mental disorders and executive brain functions.
Based on the MANOVA results (Table 2), the two groups have shown a significant difference in all components of brain executive functions and mental disorders.
| Variables | Sum of Squares | Hypothesis df | Error df | Mean Square | F | P-Value | Partial Eta Squared |
|---|---|---|---|---|---|---|---|
| Brain executive functions | |||||||
| Memory | 287.3 | 1 | 168 | 287.3 | 23.477 | 0.001 | 0.123 |
| Inhibitory control and selective attention | 1584.476 | 1 | 168 | 1584.476 | 143.884 | 0.001 | 0.461 |
| Decision-making | 636.712 | 1 | 168 | 636.712 | 38.031 | 0.001 | 0.185 |
| Planning | 219.112 | 1 | 168 | 219.112 | 59.474 | 0.001 | 0.261 |
| Sustained attention | 394.594 | 1 | 168 | 394.594 | 76.064 | 0.001 | 0.312 |
| Social cognition | 444.853 | 1 | 168 | 444.853 | 60.669 | 0.001 | 0.265 |
| Cognitive flexibility | 561.653 | 1 | 168 | 561.653 | 49.416 | 0.001 | 0.227 |
| Mental disorders | |||||||
| Physical complaint | 403.788 | 1 | 168 | 403.788 | 4.856 | 0.034 | 0.027 |
| Obsessive-compulsive | 457.888 | 1 | 168 | 457.538 | 4.538 | 0.035 | 0.026 |
| Sensitivity in mutual relationships | 716.476 | 1 | 168 | 716.476 | 13.735 | 0.001 | 0.076 |
| Depression | 676.006 | 1 | 168 | 676.006 | 4.740 | 0.031 | 0.027 |
| Anxiety | 327.624 | 1 | 168 | 327.624 | 4.231 | 0.041 | 0.025 |
| Aggression | 199.153 | 1 | 168 | 199.153 | 4.591 | 0.034 | 0.027 |
| Morbid fear | 656.212 | 1 | 168 | 656.212 | 8.61 | 0.004 | 0.049 |
| Paranoid thoughts | 370.594 | 1 | 168 | 370.594 | 4.789 | 0.030 | 0.028 |
| Psychosis | 525.888 | 1 | 168 | 525.888 | 5.387 | 0.020 | 0.031 |
Results of Multivariate Analysis of Variance to Compare Brain Executive Functions and Mental Disorders Between the Two Groups
As presented in Table 3, the parametric test one-way ANOVA indicated a significant difference in at least one of the components of mental disorder and brain executive functions between the two groups (P < 0.05).
Multivariate Analysis of Variance Results Comparing the Collective Effect of the Mean Scores of Brain Executive Functions and Mental Disorders
5. Discussion
This study compared mental disorders and executive brain functions between veterans exposed to chemical weapons and controls. Veterans had significantly higher average scores in mental disorder indices than healthy individuals in physical complaints, obsession-incontinence, sensitivity in interpersonal relationships, depression, anxiety, aggression, morbid fear, paranoid thoughts, and psychosis. Mental disorders can manifest as physical complaints. Due to war conditions and stresses, veterans were exposed to more mental and physical risks, resulting in increased physical complaints compared to controls. Mental pressures on veterans have led to ambiguity, anxiety, and more physical complaints (31). This explains the higher physical complaint scores in veterans compared to controls (32, 33).
Our results showed that veterans exposed to chemical weapons had more obsessive-compulsive symptoms than controls. Personal crises and significant adverse events can trigger OCD. Mental trauma experienced in war environments can provoke OCD symptoms in soldiers and veterans (34). Veterans had higher sensitivity scores in mutual relationships compared to controls. Previous studies have shown that Iraq and Afghanistan war veterans face multiple mental disorders and encounter difficulties in family relationships (35-37). War-induced anxiety prevents these people from establishing proper relationships, leading to increased sensitivity in mutual relationships (38).
Depression scores were higher in veterans exposed to chemical weapons compared to ordinary individuals. Depression involves various factors, including physical and environmental causes (e.g., poisoning). Considering the dire conditions veterans were exposed to, particularly with chemical weapons, their higher depression scores are justified. However, physical and environmental causes alone cannot account for the high depression scores. Some factors, such as the lack of social support and impaired socioeconomic activities (39), also contribute to the higher depression scores in veterans exposed to chemical weapons than in healthy individuals. These findings are aligned with previous findings (39-41).
In accordance with the results of other investigations (40, 42, 43), anxiety was higher among veterans exposed to chemical warfare compared to controls, likely due to the stress caused by physical conditions and resulting internal conflicts (40). Aggression among these veterans is associated with feelings of shame, depression (44), anxiety (45), and other mental problems (46). Veterans exposed to chemical weapons had higher scores in morbid fear and paranoid thoughts than controls, which can be attributed to mental disorders, including depression and anxiety (12). Similarly, the psychotic score of these veterans was higher than controls, consistent with the studies of Benazzi (47) and Lee and Nathan (48). Depression and anxiety may contribute to psychotic symptoms.
Cognitive function, including memory, inhibitory control, selective attention, decision-making, planning, sustained attention, social cognition, and cognitive flexibility, was significantly lower among veterans exposed to chemical warfare than controls. The difficulty in preventing irrelevant information from entering memory, disorganized memory, and mental confusion contributes to the low memory scores of veterans (20, 49, 50). Binder et al. (51) also noted weak memory function in war soldiers exposed to explosions. Selective attention was weaker in veterans due to attention bias and cognitive impairments (23, 46, 52). Weak executive function in decision-making and planning was observed among veterans, consistent with previous studies (27). Sustained attention scores were lower among veterans, possibly due to impaired cognitive functions (28, 46, 53). Impaired social cognition linked to PTSD affects the ability to understand and respond to others (54).
Finally, our research findings showed lower cognitive flexibility scores in veterans exposed to chemical weapons than controls. Cognitive flexibility is a structure considered part of executive functions and can be measured using behavioral paradigms (55). The critical nodes involved in cognitive flexibility in the context of the surrounding environment consist of the executive control network, which is closely related to attention and working memory (29).
This research, similar to other studies, had certain limitations. For instance, the data collection method relied on self-reporting through research questionnaires, which means that participants’ temporary perspectives may influence the information provided. Furthermore, some of the reported data may be influenced by changes in the participants’ lifestyles as they adapt to the constraints and adverse consequences of chemical exposure on their physical, mental, and social well-being. Therefore, it is recommended to incorporate proper planning strategies to improve the quality of life for these individuals.
5.1. Conclusions
Veterans exposed to chemical weapons had higher mental disorder symptoms across all domains compared to the control group. Veterans also had lower executive brain capabilities than healthy people. These findings show that chemical warfare exposure harms veterans’ mental health and cognition. Veterans had higher rates of mental problems and cognitive impairment due to special stressors and war’s horrific conditions. These results are relevant for mental health professionals treating chemical weapons veterans. This population’s greater mental disorder symptoms and lower cognitive functions can inform focused mental therapies. Specialists can help veterans exposed to chemical weapons by creating programs to reduce mental impacts and improve cognitive performance.