1. Context
Calcium channel blockers (CCBs) are commonly prescribed for adults with cardiovascular conditions (1). These blockers are typically categorized into 2 groups: Non-dihydropyridines and dihydropyridines. They find utility in treating a range of cardiovascular conditions, including hypertension, angina pectoris, coronary spasm, supraventricular dysrhythmias, hypertrophic cardiomyopathy, and pulmonary hypertension (2).
In 1997, Mahmoudian et al. introduced 2 novel CCBs, mebudipine ([±]-t-butyl, methyl-1, 4-dihydro-2, 6-dimethyl-4-[3-nitrophenyl]-3, 5-pyridine dicarboxylate) and dibudipine. These compounds, both non-symmetrical and symmetrical analogs of nifedipine, were synthesized and subjected to biological activity studies. The results suggested that these new dihydropyridine derivatives hold promise as treatments for hypertension and angina due to their effective relaxation of smooth muscle in vascular and ileal systems (3).
Mebudipine, in particular, exhibits more potent inhibitory effects that are time- and voltage-dependent when compared to nifedipine. It has demonstrated effectiveness in managing heart failure without significant negative inotropic effects while still exerting negative chronotropic effects (4).
Since no studies have explored mebudipine’s cardioprotective effects in the past 2 decades, this review delves into the potential cardioprotective properties of mebudipine. Additionally, it briefly touches upon other beneficial effects associated with this drug.
2. Evidence Acquisition
This article succinctly presents the breakthroughs in mebudipine studies, which were discovered through extensive searches in renowned scientific databases, including ScienceDirect, Google Scholar, Scopus, and PubMed. Two blinded researchers conducted these searches to identify all eligible studies using the keyword "mebudipine." The specific focus was on investigating the "Mebudipine effect on the cardiovascular system."
All studies related to this drug within the last 20 years, identified using the mentioned keywords, were thoroughly examined. A total of 25 original articles from the literature were found, and each of them underwent a comprehensive review for inclusion in this study. This review article discusses all the original research studies concerning mebudipine’s effects on the cardiovascular system or any organs that impact cardiovascular function.
3. Results
3.1. Pharmacokinetics of Mebudipine in Rats
Mebudipine, a novel calcium antagonist, underwent a study in rats. Following intravenous administration, its plasma concentration exhibited a half-life of 2.84 hours, a blood clearance of 1.67 L/h/kg, and a volume of distribution of 6.26 L/kg. However, upon oral administration, mebudipine displayed low bioavailability, indicating a significant first-pass effect. The drug is rapidly distributed into various tissues, including the brain, heart, liver, and kidneys, residing in the same compartment as plasma (5). Additionally, Bohlooli et al. (6) developed a high-performance liquid chromatography (HPLC) method to measure dibudipine levels in biological fluids in rats. The drug also exhibited low oral bioavailability and demonstrated a bi-exponential decline following intravenous injection. The HPLC method proved to be user-friendly and suitable for further investigations. Furthermore, a new compound called mebudipine was identified, and an HPLC method was developed to measure it in rabbit plasma. This method was found to be accurate, sensitive, and suitable for studying the pharmacokinetics of Mebudipine (7).
3.2. Determination of Mebudipine in Human Plasma
A study conducted by Asgari et al. (8) aimed to measure mebudipine levels in human plasma. In plasma, mebudipine exhibited a limit of quantification of 5 ng/mL, a mean extraction efficiency of 84%, and linearity within the range of 5 to 100 ng/mL (r2 > 0.99). This study demonstrated that liquid chromatography-tandem mass spectrometry is a reliable method for detecting mebudipine in human plasma. It offers accuracy, sensitivity, selectivity, and low coefficients of variation and error.
3.3. Mechanism of Vasoselective Action of Mebudipine
Mebudipine, a novel CCB, was investigated for its vasoselective action. It effectively inhibited potassium chloride (KCl)-induced contractions and demonstrated a greater impact when aortic rings were depolarized. Compared to nifedipine, mebudipine exhibited stronger inhibitory effects and displayed negative chronotropic and inotropic effects (9). Mebudipine had a negative impact on heart rate but positively affected inotropy, distinguishing it from nifedipine. These findings suggest that mebudipine has the potential for use in cardiovascular diseases without causing harmful side effects. It may exert a selective and protective effect on calcium channels in ischemic areas, making it a promising treatment option for cardiovascular diseases with a favorable safety profile. Mebudipine, a dihydropyridine CCB, demonstrated greater time- and voltage-dependent inhibitory effects compared to nifedipine (9).
3.4. Evaluation of Mutagenicity of Mebudipine, a New Calcium Channel Blocker
Gholami et al. (10) conducted an Ames assay with liver enzymes (S-9 mix) to assess the mutagenic effects of mebudipine. The test was found to be reliable and accurate. Mebudipine was evaluated for mutagenicity using Salmonella TA102, both with and without S-9. Six doses, ranging from 39 μg to 1250 μg per plate, were employed. The colony counts remained within the safe range for all doses, indicating that mebudipine did not exhibit mutagenic properties.
3.5. Mebudipine as a Nanoemulsion Drug
A nanoemulsion drug delivery system was developed to enhance the oral bioavailability of mebudipine, a calcium channel blocker with low water solubility. Khani et al. (11) conducted a study to evaluate the impact of nano-formulation on the pharmacokinetic parameters of mebudipine in rats. According to the study, mebudipine nanoemulsion exhibited 2.6-, 2.0-, and 1.9-fold higher relative bioavailability compared to suspension, ethyl oleate solution, and micellar solution, respectively. Their research suggested that employing a nanoemulsion as a delivery method is highly advantageous for molecules with poor water solubility, such as mebudipine.
To enhance the effectiveness of antihypertensive therapy, a nanoemulsion was developed to improve the bioavailability of mebudipine. The particle size in the formulation was assessed using dynamic light scattering. Subsequently, artificial neural networks were utilized to identify the factors influencing the particle size of the nanoemulsion. Three input variables were examined, namely the amount of surfactant system (T80 + S80), the quantity of polyethylene glycol, and the amount of ethanol as cosurfactants, while the particle size served as the output parameter. The model indicated that as each input value increased, the particle size decreased. Furthermore, it was determined that the quantity of surfactant had the most significant impact on regulating the final particle size of the nanoemulsion (12).
3.6. Improved Oral Bioavailability of Mebudipine upon Administration in PhytoSolve and Phosal-Based Formulation
An investigation by Khani and Keyhanfar (13) explored how PhytoSolve and phosal-based formulation (PBF) could enhance the oral absorption of mebudipine, a calcium channel blocker with low water solubility. The study assessed the absorption of various mebudipine formulations (PhytoSolve, PBF, oily solution, and suspension) in rats through oral administration. Both PBF and PhytoSolve formulations could be mixed with water in any proportion and did not exhibit separation or drug precipitation during storage for up to a month. Notably, when mebudipine was formulated with PhytoSolve and PBF, it displayed superior bioavailability compared to suspension and oily solutions. These novel formulations hold promise as alternative carriers to increase the oral bioavailability of poorly water-soluble molecules like mebudipine (13).
3.7. Therapeutic Effects of Mebudipine
3.7.1. Effects on the Heart, Blood Pressure, and Internal Mammary Artery
Mebudipine and dibudipine demonstrated a mild reduction in left atrium contractions in rats compared to nifedipine. Both drugs effectively lowered rat blood pressure, with mebudipine exhibiting a similar effect to nifedipine, while dibudipine’s effect was somewhat weaker but of longer duration (14). Notably, mebudipine exhibited slower absorption kinetics than nifedipine. These new compounds, mebudipine, and dibudipine, displayed relaxing effects similar to nifedipine on KCl-treated human internal mammary arteries. Mebudipine was particularly identified as a vasoselective compound with potent blood pressure-lowering effects and significant vasorelaxant properties. Both compounds reproduced their vasorelaxant actions in human vascular preparations and showed mild cardio-depressant effects (14).
3.7.2. Effects on Heart Myocardial Arrhythmia Induced by Ischemia-Reperfusion Injury
Following an ischemic injury, reestablishing blood flow to the heart can lead to hazardous cardiac arrhythmias and the death of myocardial cells through apoptosis and necrosis. Calcium channel blockers (CCBs) have been recognized for their ability to safeguard the myocardium from damage and arrhythmias (15). Ghiasi et al. conducted a study to investigate mebudipine’s impact on myocardial arrhythmias and tissue injury in isolated rat hearts subjected to ischemia/reperfusion. The study closely monitored electrocardiographs, assessed serum lactate dehydrogenase (LDH) and creatine phosphokinase (CPK) activities in coronary effluent, and examined the microscopic architecture of the myocardium. Mebudipine demonstrated a reduction in ventricular arrhythmias, an improvement in edema and inflammation, and decreased tissue damage compared to the control group (15).
3.7.3. Effect on Oxidative Stress and the Nitric Oxide System in Myocardial Ischemia-Reperfusion Injury
Myocardial infarction, characterized by a loss of blood supply to the heart, leads to oxidative stress and myocardial necrosis. In a study by Ghyasi et al., mebudipine’s impact on lipid peroxidation and antioxidant enzymes in myocardial ischemia-reperfusion injury was explored. The results indicated that mebudipine reduced oxidative damage and lipid peroxidation while enhancing antioxidant enzyme activities and myocardial function. Consequently, this drug has the potential to mitigate the severity of the cardiac ischemic injury and exhibit cardioprotective effects. Mebudipine may influence the nitric oxide system and heart function during ischemia-reperfusion injury in rats. A deficiency in nitric oxide production can contribute to myocardial ischemia-reperfusion injury. Administration of mebudipine resulted in improved heart function, reduced levels of lactate dehydrogenase and creatine kinase in coronary effluent, and increased nitric oxide metabolite levels in the heart compared to the control group (16).
3.7.4. Effect on Vascular Flow of Isolated Kidney in Normal and Diabetic Rats
Calcium channel blockers are commonly prescribed for hypertension and can also improve renal function in individuals with essential hypertensive renal disease or diabetic renal disease. Recent studies have highlighted the beneficial effects of dihydropyridine-type CCBs, such as mebudipine and dibudipine, in enhancing renal blood flow in normal rat kidneys. Sepehr-Ara et al. examined the impact of these new drugs on blood flow in diabetic rat kidneys, comparing them to nifedipine, and assessed whether their effects varied in isolated perfused kidneys. The study concluded that mebudipine and dibudipine were more effective than nifedipine in inhibiting phenylephrine (PE)-induced perfusion pressure in diabetic rats, even at lower concentrations. Furthermore, it has been shown that CCBs, specifically dihydropyridine derivatives, are commonly used to treat hypertension. They can also help improve renal function in patients with essential hypertensive renal disease or diabetic renal disease. These compounds were found to exert similar vasodilatory effects in both vascular and ileal smooth muscle tissue (17).
3.7.5. Effects on Cerebral Oxygen-Glucose Deprivation/Reperfusion Injury
Tavakoli-Far et al. conducted a study to investigate the potential neuroprotective effects of new calcium channel blockers, mebudipine, and dibudipine on primary murine cortical neurons subjected to oxygen-glucose deprivation/reperfusion injury. Their findings suggested that the neuroprotective effects were dose-dependent and possibly associated with a reduction in nitric oxide production. These findings indicate a potential role for mebudipine and dibudipine in protecting neurons from ischemic injury (18).
3.7.6. Effects on PC12 Cells Against Oxygen-Glucose Deprivation and Glutamate
Mebudipine and dibudipine, two new L-type CCBs, demonstrated significant neuroprotective effects against glutamate and oxygen-glucose deprivation-induced neurotoxicity in PC12 cells. Importantly, they outperformed nimodipine in terms of neuroprotection (19).
3.7.7. Effects on Voltage-Activated Calcium Currents in PC12 Cells
Rouzrokh et al. investigated 2 novel CCBs, mebudipine, and dibudipine, and assessed their relaxing effects on vascular and atrial smooth muscle. Their potency was compared to amlodipine using differentiated PC12 cells. The study found that mebudipine exhibited similar potency to amlodipine, whereas dibudipine was somewhat less potent. Notably, undifferentiated PC12 cells did not display voltage-activated Ca2+ currents (20).
3.7.8. Effects on Guinea-Pig Isolated Common Bile Duct
Beigly et al. examined the effects of CCBs on contractions in the guinea pig bile duct. All the compounds tested reduced the amplitude of the contractile response and shifted the concentration-response curve of calcium chloride to the right. Additionally, these compounds exhibited antagonistic effects on the contractile response of the K+-depolarized bile duct, although their inhibitory effects were not significantly different (21).
3.7.9. Effect on Ca2+ Spikes in F1 Neuronal Soma Membrane in Helix Aspersa
New calcium channel blockers, mebudipine, and dibudipine, were synthesized and evaluated for their inhibitory actions on high-threshold Ca2+ spikes in helix aspersa. Both compounds demonstrated reversible effects, with mebudipine being identified as the most potent among them. Notably, neither the new dihydropyridines nor nifedipine altered the resting membrane potential (22). Table 1 shows the pharmacokinetics of mebudipine.
| References | ||
|---|---|---|
| Pharmacokinetics of mebudipine | Quickly enters tissues like the brain, heart, liver, and kidney but has low bioavailability due to the first-pass effect. | (5) |
| Liquid chromatography-tandem mass spectrometry is a reliable method for detecting it. | (8) | |
| PhytoSolve and Phosal-based formulation can improve its absorption. | (13) | |
| Surfactants play the most significant role in regulating the ultimate particle size of mebudipine nanoemulsion. | (12) | |
| The nanoemulsion delivery method is advantageous for mebudipine. | (11) | |
| HPLC was a reliable method to measure mebudipine in rabbit plasma | (7) |
Pharmacokinetics of Mebudipine
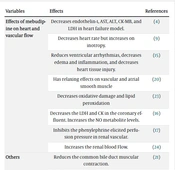
As shown in Table 2, mebudipine effects on the cardiovascular system and some organs of the body have been reported.
| Variables | Effects | References |
|---|---|---|
| Effects of mebudipine on heart and vascular flow | Decreases endothelin-1, AST, ALT, CK-MB, and LDH in heart failure model. | (4) |
| Decreases heart rate but increases on inotropy. | (9) | |
| Reduces ventricular arrhythmias, decreases edema and inflammation, and decreases heart tissue injury. | (15) | |
| Has relaxing effects on vascular and atrial smooth muscle | (20) | |
| Decreases oxidative damage and lipid peroxidation | (23) | |
| Decreases the LDH and CK in the coronary effluent. Increases the NO metabolite levels. | (16) | |
| Inhibits the phenylephrine elicited perfusion pressure in renal vascular. | (17) | |
| Increases the renal blood Flow. | (24) | |
| Others | Reduces the common bile duct muscular contraction. | (21) |
| Decreases oxygen-glucose deprivation-induced neurotoxicity in PC12 cells. | (19) | |
| It not found to be mutagenic. | (10) | |
| It is in line with optimized selective mineralocorticoid receptor analogs. | (25) | |
| Inhibits high threshold Ca2+ spikes in Helix aspersa. | (22) | |
| It protects primary murine cortical neurons from oxygen-glucose deprivation/reperfusion injury. | (18) |
Mebudipine Effects on the Cardiovascular System and Some Organs of the Body
4. Discussion
1,4-DHP nifedipine is commonly prescribed for hypertension and angina but possesses certain drawbacks, including its rapid onset of vasodilating action and a short half-life. To address these limitations, newer analogs such as mebudipine and dibudipine have been developed, featuring t-butyl substituents aimed at altering metabolism without compromising activity. Bohlooli et al. (5) conducted a study to investigate the metabolism of these novel 1,4-DHP compounds in rat hepatocytes. Interestingly, mebudipine and dibudipine were found to undergo metabolism in a manner similar to nifedipine, involving hydroxylation followed by O-glucuronidation. Importantly, these compounds exhibited longer in-vitro half-lives compared to nifedipine, rendering them promising candidates for further development.
Furthermore, researchers explored the potential of nanoemulsions to enhance the effectiveness of antihypertensive treatment by improving the bioavailability of mebudipine. Khani et al. in 2019 employed dynamic light scattering to measure particle size and utilized artificial neural networks to identify variables influencing particle size (12). In a similar study, Shanaghi et al. (26) investigated the impact of surfactant/lipid concentration on particle size. Additionally, Ilić et al. in 202327 demonstrated that lipid nanocarriers could facilitate drug delivery to the brain by overcoming blood-brain barriers in the central nervous system (CNS). In line with these findings, Khani et al. in 2016 evaluated the oral nanoemulsion drug delivery of mebudipine, resulting in improved oral bioavailability (11). Nanoemulsions have gained recognition as an advantageous drug delivery option, offering easy preparation, enhanced drug absorption, and improved bioavailability. They can encapsulate both hydrophilic and hydrophobic drugs and represent a valuable addition to current therapeutic strategies (27). Additionally, Ajdary et al. (28) discovered that employing a PBF in a sustained-release formulation of clomiphene citrate could enhance targeting efficiency, thereby improving its impact on implantation and gene expression.
Moreover, Aali et al. (4) investigated the effects of mebudipine and amlodipine on heart rate in animals with heart failure (HF). Their findings revealed that mebudipine was capable of reversing plasma biomarker values in treated animals, restoring them closer to baseline levels when compared to the HF control group. These results suggest a potential protective effect of mebudipine on the heart organ. This notion is supported by the study conducted by Ghiasi et al. (15), which demonstrated that mebudipine could reduce ventricular arrhythmias. Additionally, CCBs have long been used as routine medications for the treatment of arrhythmias (29). Furthermore, Ghyasi et al. (16) reported that the administration of mebudipine led to improved heart function and increased nitric oxide metabolite levels in the heart. These findings collectively suggest that mebudipine may help mitigate oxidative damage, similar to verapamil (a non-dihydropyridine CCB) (30).
4.1. Conclusions
Based on the mentioned study, it appears that mebudipine exhibits a protective effect on the cardiovascular system and various other human organs. The mechanisms contributing to its cardioprotective effects may involve the reduction of endothelin-1, AST, ALT, CK-MB, and LDH levels. Additionally, mebudipine has a positive impact on heart inotropy, resulting in reduced occurrences of ventricular arrhythmias, edema, oxidative damage, inflammation, and decreased heart tissue injury. Furthermore, mebudipine demonstrates vasorelaxant properties, affecting blood vessels and smooth muscles in the atria.