1. Introduction
Cervical cancer is one of the top five most common cancers in women worldwide with a high mortality rate (1). Radical hysterectomy is indicated for patients with cervical cancer (2). Others suggest radical hysterectomy in the early stages of cervical cancer for reducing the recurrence rate and improving the patients’ survival (3). This is while radical hysterectomy is associated with several complications, such as infection, thromboembolism, genitourinary injury, bleeding, nerve injury, and dehiscence, which increase the risk of postsurgical morbidity and mortality (4). Furthermore, the patient undergoing hysterectomy is deprived of conception in the future, which can affect her sexual and social life (5). Accordingly, studies have focused on observational therapies for patients with cervical cancer who wish to preserve their fertility, known as fertility-sparing management strategies, including neoadjuvant chemotherapy, trachelectomy, and large loop excision of the transformation zone (large loop conization) (6). These methods are suggested for early-stage cervical cancers with specific pathologies, such as squamous cell carcinoma and adenocarcinoma, but not at other stages or other pathologies, like neuroendocrine tumors (REF).
Radical trachelectomy (RT) with pelvic lymph node assessment (with or without neoadjuvant chemotherapy) is an acceptable method for selected patients with cervical cancer, who wish to maintain their fertility (7). This method can be performed by two approaches; abdominal and vaginal, each with their own advantages and disadvantages (8). The vaginal radical trachelectomy (VRT) has the advantage of less bleeding and higher pregnancy rate, while the abdominal approach has other advantages, such as larger resection, lower recurrence rate, and better oncology results that allow for safe management of invasive cervical cancers ≥ 2 cm with a survival rate similar to radical hysterectomy (8). However, the matter of lower fertility rate compared to the general population, the higher rate of pregnancy complications, and the need for hysterectomy in future questions the choice of trachelectomy over radical hysterectomy, mainly for the sake of fertility preservation (9). The patient reported here, was a 39-year-old woman with high-grade invasive cervical cancer, squamous cell carcinoma (SCC) that was successfully managed by laparoscopic lymphadenectomy and radical trachelectomy and leading to normal pregnancy in the following years.
2. Case Presentation
The case described here was a 39-year-old woman, married at the age of 18 years, with two successful pregnancies at the ages of 20 and 22 years. On admission (Jan 2016), she expressed her concern for frequent vaginal discharge and postcoital bleeding. On physical examination, she had no systemic problem; in the examination of external genitalia, the external appearance of the vulva was normal and examination with speculum showed normal appearance of the cervix and a multiparous and hypertrophic cervix was observed with yellow discharge, suggestive of chlamydia cervicitis. Pelvic examination showed that the consistency of the cervix was harder than normal; uterus and adnexa were normal. Simultaneous vaginal and rectal examination showed that the parameters and fornices of vagina were free. The results of Pap smear showed squamous intraepithelial lesion (HSIL).
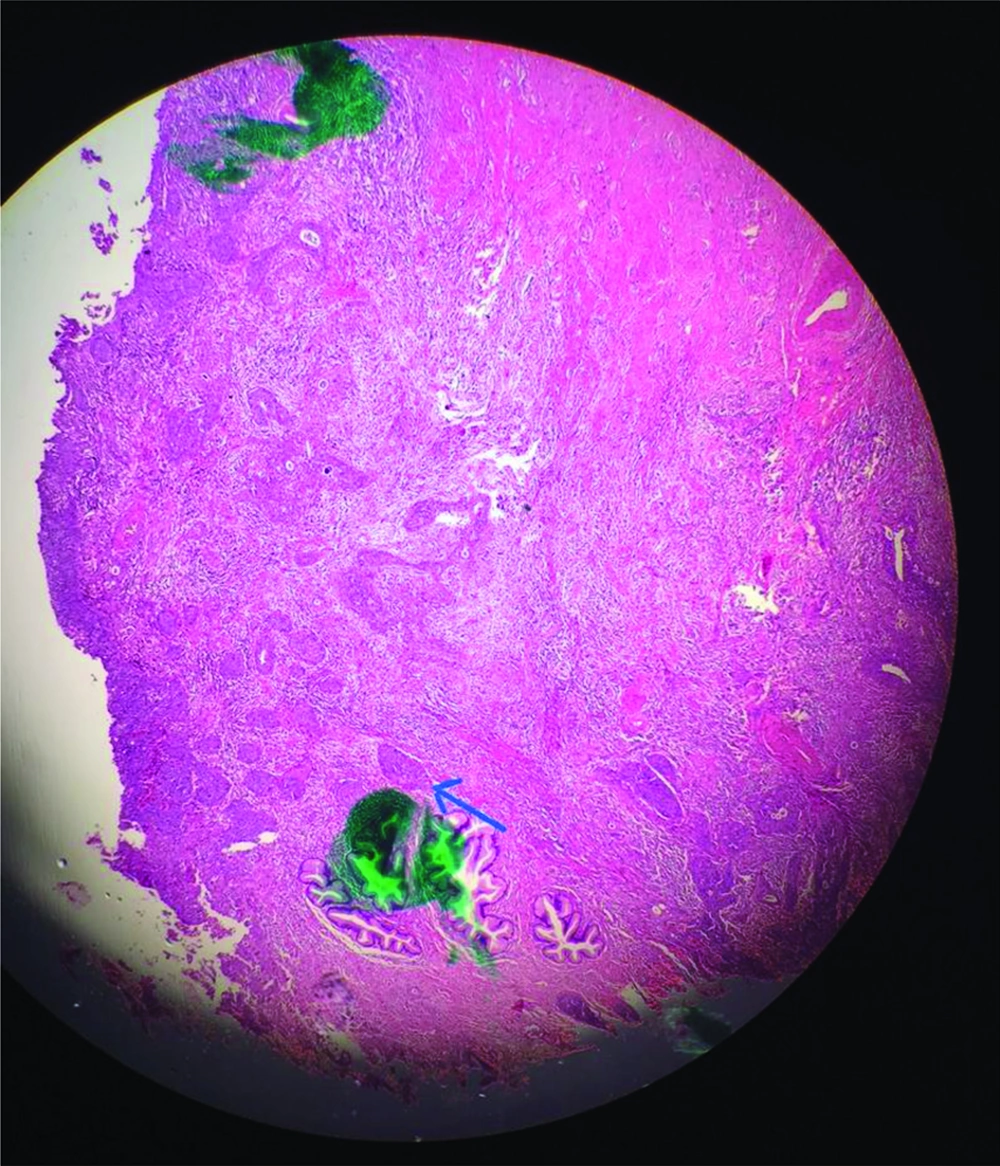
The patient underwent vaginocervical colposcopy, performed by an oncologist gynecologist. Cervical colposcopy was performed using 3% acetic acid solution and green filter, the results of which revealed an acetowhite dense lesion at 5 o’clock position of the cervix, coarse mosaic and coarse punctuation with abnormal vascularization (not branching), suggestive of high-grade lesion. The cervical lesion was biopsied and the pathologic report was cervical intraepithelial neoplasia grade 3 (CIN III). Therefore, the patient was scheduled for conization, performed by the same oncologist gynecologist, the results of its pathologic examination which showed invasive cervical SCC, large cell, non-keratinizing, and the depth of invasion was reported at 6mm, which suggested the stage at IB1 (Figure 1). During surgery, under anesthesia, the parameters and fornices of vagina were normal.
After consulting with the patient, the patient expressed her willingness to preserve her uterus for future pregnancy. As the magnetic resonance imaging (MRI) suggested a small lesion, limited to exocervix with appropriate distance to internal os, without parameter or vaginal involvement (Figure 2), VRT was suggested for the patient after explaining the probable complications of this surgery to her. A laparoscopic oncologist and an oncologist gynecologist performed the surgery. Laparoscopic lymphadenectomy was performed at dorsal lithotomic position and the lymph nodes of para-aortic, common iliac, external iliac, internal iliac regions were resected bilaterally and extracted using an endobag (We could not perform sentinel node biopsy, as we did not have gamma probe at the center). The samples were sent immediately for frozen section examination, the results of which showed that the lymph nodes were negative for malignancy. The VRT was performed for the patient by one laparoscopic and one gynecologic oncologist with great caution not to damage the ureters. The internal margin at about 0.5 cm of the cervical internal os was sent for frozen section, the results of which were negative, as well. A permanent cerclage with MersileneTM thread was done and the uterine corpus was sewn to the vagina and the VRT was ended this way. There was no apparent tumor on the cervix (macroscopically) and the appearance of the cervix was a hypertrophic and hyperemic cervix. After surgery, the patient was transferred to the recovery room and then to the gynecologic ward; she received prophylactic antibiotics with 2 g Keflin; the first dose was given at the beginning of the surgery and continued until 24 hours. Pneumatic compression was used for prophylaxis of deep vein thrombosis during surgery. Also, 5,000 IU subcutaneous heparin was prescribed for the patient in beginning and before surgery and continued TDS until two days after surgery. The final pathologic report confirmed the results of conization.
Two days after surgery, the patient was discharged with good condition and with a prescription of 40mg Clexane® every day for one week and diclofenac tablet twice a day (in case of pain). The patient was advised to refer to the physician, in case of fever, urinary problems, and vaginal bleeding. As recommended by her physician, she referred to the gynecologist every three months for follow-up. During the first six weeks, the patient had no post-surgical complications. At each visit, the patient was examined with vaginal examination. Six months after surgery, the patient was visited by the gynecologist and a Pap smear was performed for the patient, the results of which were negative. One year after surgery, she underwent colposcopy examination and high risk HPV (Cobas® test) by the gynecologist, the results of which were normal and negative, respectively. After two years of follow-up, the patient was advised that she can get pregnant from this time on. She conceived naturally; during pregnancy, under prenatal observation and obstetric consultation, she experienced no complications and at 38th gestational week she underwent an elective cesarean section. She gave birth to a full-term girl neonate with the first and fifth minute APGAR of 10/10. One year after delivery, the patient had a normal life without any postsurgical complications. Written informed consent was obtained from the patient for reporting this case.
3. Discussion
Cervical cancer is an important cancer among women and fertility-sparing procedures are becoming more common with the recent development for earlier detection of cervical cancer, decreased age of cervical cancer in women, increased age of conception, and willingness of women to preserve their fertility (6). Here we reported our experience in order to draw the researcher’s attention to the fact that the issue of the fertility-sparing procedure is not only important for oncologists and gynecologic surgeons, but also for obstetricians, due to the incomparable conditions of pregnancy in the post-trachelectomy patient (10).
The presented case here had term delivery two years after surgery, conceived naturally, without any complications during this pregnancy or any miscarriages during the post-surgical period. Several aspects of this finding is noteworthy. First, it has been previously reported that patients undergoing RT may have low fertility rate, while the patients presented here, naturally conceived in about less than two years after her surgery. The second important finding in the patient was the interval between surgery and pregnancy. Four months was suggested for stopping the contraception, as she had no postsurgical complication and normal test results at each postoperative visit, while a minimum of 6 months is recommended for sufficient wound healing and preparedness of the uterus for conception (10). Thirdly, previous studies have reported a high risk of miscarriage, preterm delivery, and premature rupture of membranes (11, 12), which were not observed in the patient presented here she experienced a full-term pregnancy with live and healthy fetus. This is while the mean gestational age of 33 weeks is reported in patients following RT and a high rate of preterm delivery is reported (11).
Although there were no pregnancy complications in our patient, the increased risk of pregnancy complications has to be fully explained to the patient, before she decides on the conception and the patient should be advised to refer frequently for the follow-up and follow the instructions carefully (10), as we did for the patient. Pre-operative obstetric consultation for a better pregnancy outcome in patients candidate of RT also have been suggested (13). According to the experience, we believe that appropriate obstetric care in addition to appropriate surgical strategies can result in favorable obstetric outcome after VRT, although the tumor stage and underlying diseases of the patient also play an important role.
According to the oncologist, the patient’s outcome in the present study showed that VRT can be successfully performed in patients with invasive cervical cancers that is in line with the results of previous studies (14, 15). Our patient had invasive cervical SCC at stage IB1 (due to 6mm depth of invasion). This is while most have considered trachelectomy for tumor stages IA1-IIA (16) and recent evidence has suggested its safety in cervical cancers IB1 ≥ 2 cm (14, 15). The case presented here also showed the safety of this procedure in IB1 cervical SCC with no postoperative complications and no recurrence until 2 years after surgery. Although the patient had no recurrence, the physician explained the symptoms of recurrence, such as abdominal or pelvic pain, lymphedema, abnormal vaginal bleeding or discharge, urinary symptoms, and weight loss at the time of discharge and at each postoperative visit, as recommended (9). Some patients may require adjuvant chemotherapy or radiation (17, 18), although the patient presented here did not. Notably, the patients require special postoperative care, even when not pregnant, in order to diagnose the recurrent cases and manage them appropriately.
In conclusion, the case presented here confirmed the results of previous studies on the safety of VRT in patients with invasive cervical SCC and showed that these patients can have a normal pregnancy when all obstetric considerations are taken into account. These results suggested this procedure as an appropriate option for preservation of the woman’s childbearing function without significant complications. Hence, this study only reported one case and further studies are required to confirm these results.