1. Background
Malignancy and the management methods of cancer can lead to several side effects by direct and indirect mechanisms (1). Radiation cystitis is bladder lining urothelium inflammation as a complication of bladder irradiation due to pelvic organs malignancies (2). Pelvic organs malignancies are more common in men. However, prostate (3-7) and bladder cancer in men and uterine and ovarian cancer in women are more common than pelvic organs malignancies (8). Radiation therapy (RT) is a therapeutic option to manage the pelvic organs malignancies and bladder is one of the organs irritating during pelvic region radiation, 6% - 21% of these patients experienced lower urinary tract symptoms (LUTS) and 9% of men who radiated due to prostate cancer suffered from moderate to severe radiation cystitis symptoms (2, 9, 10). Radiation-induced cystitis symptoms vary from microscopic hematuria and LUTS to gross hematuria, urinary incontinence, fistulae formation, and death (11).
The concept of a defective glycosaminoglycan (GAG) barrier is thought to be related to the pathogenesis of several vesical situations, including urinary tract infection, calculi, idiopathic detrusor overactivity, interstitial cystitis (IC), and chemical or radiation cystitis, as such may assign different approaches to the management of those diseases (12, 13).
There is an increasing body of evidence that introduces different modalities to manage this situation and repair the GAG layer, including hyperbaric oxygen, intravesical heparin, hyaluronic acid (HA), oral pentosane polysulfate (Elmiron), and even surgery (13, 14).
A derivative of HA, sodium hyaluronate, has been produced to recharge the insufficient GAG layer and has been used successfully in the management of IC and newly in treating RT-induced Cystitis (15).
Among which, intravesical hyaluronic acid (HA) instillation revealed promising outcomes treatment for various uncomfortable symptoms in the bladder, such as interstitial cystitis. However, the evidence for radiation cystitis is limited and the definite regimen was not clarified (16, 17).
Radiation-induced cystitis symptoms have detrimental sequels on the quality of life (QOL) and a number of valid tools are introduced to evaluate these effects such as King’s health questionnaire (KHQ) (18), but there are few studies reporting outcomes using valid QOL criteria following treatment with intravesical Cystistat.
The King’s Health questionnaire is a health-related QOL instrument for the evaluation of cases with LUTS disease. The questionnaire has demonstrated validity and reliability in both genders and is available in 34 culturally and linguistically validated translations. All King’s Health questionnaire domains are scored on a 0 (best) to 100 (worst) scales (19).
2. Objectives
Thus, this randomized controlled trial (RCT) aimed at assessing the potency of a specific regimen of Cystistat in controlling radiation cystitis symptoms by focusing on patients’ QOL and its chronological change.
3. Methods
3.1. Population and Sample Size
In this RCT, from October 2017 to 2019, 72 patients, blind to treatment regimen, who underwent radiotherapy (conventional or intensity-modulated radiotherapy (IMRT)) due to pelvic malignancy after at least 6 months from RT were enrolled in this study. The RT was delivered in different centers and developed cystitis symptoms in grades II and III according to the radiation therapy oncology group (RTOG). Classification of durable complications and toxicity after RT was made in Shohada-e-Tajrish Hospital, Tertiary Referral Center, Tehran, Iran. Three subjects in the case and two in the control group were categorized in grade III cystitis symptoms.
Sample size calculations were based on the outcome of QOL score after 3-month intravesical instillation of Cystistat in a pilot study among 10 patients with grade II radiation cystitis. A 10% loss to follow-up was anticipated with a significance level of 0.05 and a power of 80%. Finally, the sample size to illustrate the superiority of a treatment arm to a control arm was 30 patients.
3.2. Exclusion Criteria
Patients with a history of benign prostate hyperplasia (BPH), urethral stricture disease, neurology and neurosurgery problems, diuretics drugs consumption, diabetes mellitus, and vesicoureteral reflux were excluded.
3.3. Study Protocol
Before any interventions, urine culture requested, cystoscopy and bladder wall random biopsy were carried out for all the patients. Finally, patients with negative urine culture and normal cystoscopy except radiation consequences and negative for malignancy pathology were reported and if patients did not respond to routine treatments of cystitis were included in the study. Before the treatment, all demographic data and type of cancer were collected. Grades of hematuria range from 0 to 100 and scores of pelvic pain, according to Visual Analogue scale (VAS), range from 0 to 10 were collected by questionnaire and all the patients fulfilled KHQ to evaluate QOL before treatment and 3, 6, and 9 months after treatment.
3.4. Randomization
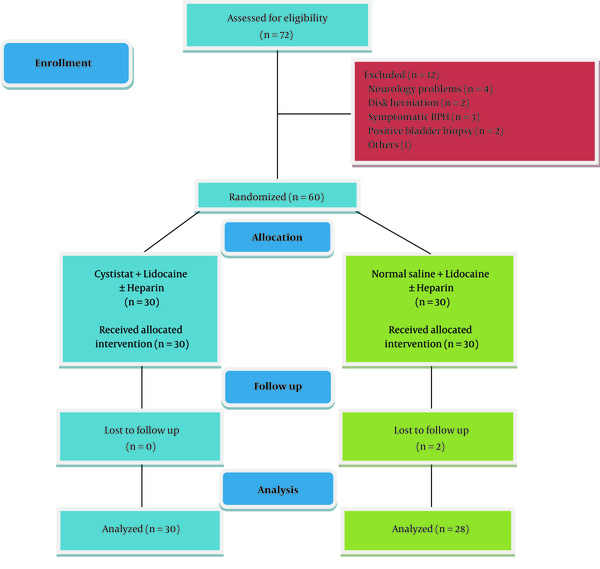
The patients were randomly assigned to 2 arms using a random number table, and allocation was concealed by sealed envelopes. In the first group, 40 mg (50 ccs) of cystistat (Mylan, United States) with a vial of 2% lidocaine and one vial of heparin 5000 unit was injected into the bladder via 14 French nelaton catheters, and in the second group, cystistat was replaced with 50 ccs normal saline and the solution was kept in the bladder for one hour. According to the Ethics Committee comment, heparin was used as a standard treatment for both groups. In patients with gross hematuria, heparin was omitted from the solution. This solution was injected weekly for up to 4 weeks and then monthly for up to 2 months and after each instillation, the patients received antibiotics for 3 days to prevent infection. All cases visited at 3, 6, and 9 months after the intervention. Figure 1 shows the selection process of the patients in this study.
3.5. Primary and Secondary End-Point
Improvement in hematuria and VAS of pelvic pain as a primary goal and promotion of QOL score in the form of KHQ as a secondary goal were collected from all the subjects and was compared between the two arms.
3.6. Statistical Analysis
We used SPSS21 software to analyze data, and quantitative variables were shawn through mean ± standard deviations (SD). Independent t-test, chi-square, and repeated measurement test were used to data analysis.
This study was approved by the ethics committee of Shahid Beheshti University of Medical Sciences, Urology and Nephrology Research Center and also the written informed consent was taken from the patients.
4. Results
We enrolled 58 patients in this study (30 cases in the case group-28 cases in the control group). The mean age of them was 63.93 ± 10.89 years old (range: 38 - 82 years). Sixteen patients were female (53.3%) in the Cystistat group and 16 patients were male (57.1%) in the control group. Most common malignancies between men were prostate cancer (12 cases), rectal cancer (8 cases) and colon malignancy (6 cases) and in women were ovarian, uterine, and cervix (8, 6, and 6 patients, respectively).
The radiation therapy session and dosage were 25 - 28, 45 - 60 Gy in rectal cancer; 33 - 36, 55 - 70 Gy in prostate adenocarcinoma; 25 - 28, 50 - 60 Gy in cervix malignancy, 25 sessions, 45 Gy in endometrial cancer and 10 courses, 30 Gy in ovarian cancer.
There was no statistically significant difference between the sexes in the two study groups (P = 0.29). Table 1 shows the baseline data of the patients.
| Characteristics | Group | Values | P Value |
|---|---|---|---|
| Age | Case | 62.73 ± 10.44 | 0.39 |
| Control | 65.21 ± 11.40 | ||
| Total score of KHQ1 | Case | 452.00 ± 100.69 | 0.41 |
| Control | 414.44 ± 90.70 | ||
| General health | Case | 70.00 ± 23.11 | 0.80 |
| Control | 66.96 ± 21.57 | ||
| Incontinence impact | Case | 66.62 ± 23.17 | 0.58 |
| Control | 69.00 ± 20.15 | ||
| Role limitations | Case | 60.52 ± 20.75 | 0.77 |
| Control | 58.89 ± 19.49 | ||
| Physical limitations | Case | 62.36 ± 18.77 | 0.40 |
| Control | 55.32 ± 15.06 | ||
| Social limitations | Case | 66.97 ± 17.48 | 0.85 |
| Control | 61.46 ± 17.55 | ||
| Relationships | Case | 61.07 ± 17.13 | 0.56 |
| Control | 58.90 ± 18.40 | ||
| Emotions | Case | 66.97 ± 16.09 | 0.30 |
| Control | 63.83 ± 16.99 | ||
| Sleep/energy | Case | 63.85 ± 16.99 | 0.89 |
| Control | 58.30 ± 16.65 | ||
| Severity measures | Case | 71.07 ± 17.47 | 0.87 |
| Control | 57.70 ± 17.26 | ||
| VAS2 | Case | 7.90 ± 1.626 | 0.41 |
| Control | 7.54 ± 1.753 |
Comparison of the Basic Characteristics of the Patients Between the Two Groupsa
As the above table shows, there were no statistically significant differences between the groups at baseline (P > 0.05), and the distribution of data was normal.
Table 2 lists the changes in King’s Health questionnaire Scores sub-categories at different times in 1, 3, and 6 months after intervention.
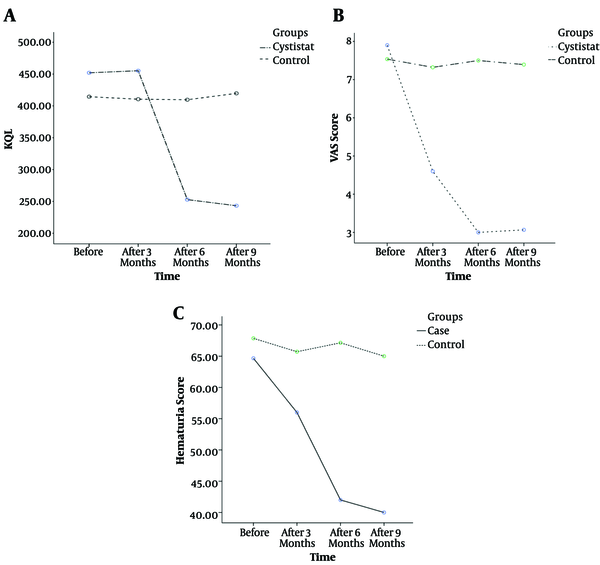
As Table 2 shows, the mean of each-sub-category of QOL, total score of QOL, and VAS were significantly improved in comparison to the control group at each time of follow-up after 3, 6 and 9 months of intervention (P < 0.05).
The mean score of hematuria was 64.66 ± 20.80 in the case group and 67.85 ± 20.61 in the control group (P = 0.56). However, it was significantly different in the third, sixth, and ninth month follow-ups (in the third month: 56 ± 13.28 vs. 65.71 ± 15.25; in the sixth month: 42 ± 12.14 vs. 67.14, in the ninth month: 40 ± 11.74 vs. 65 ± 11.70 in case and control groups, respectively).
| Characteristics | Group | After 3 Months | P Value | After 6 Months | P Value | After 9 Months | P Value |
|---|---|---|---|---|---|---|---|
| Total score of KHQ1 | Case | 455.23 ± 54.47 | 0.659 | 252.78 ± 52.36 | < 0.0001 | 243.17 ± 60.77 | < 0.0001 |
| Control | 410.50 ± 76.38 | 409.67 ± 62.84 | 419.69 ± 60.21 | ||||
| General health | Case | 36.67 ± 14.28 | < 0.0001 | 20.00 ± 13.77 | 0.019 | 20.00 ± 15.25 | < 0.0001 |
| Control | 55.36 ± 19.67 | 61.61 ± 18.61 | 61.61 ± 19.816 | ||||
| Incontinence impact | Case | 33.30 ± 17.49 | < 0.0001 | 19.98 ± 16.59 | < 0.0001 | 25.53 ± 20.84 | 0.025 |
| Control | 61.85 ± 19.69 | 64.23 ± 17.98 | 67.80 ± 16.94 | ||||
| Role limitations | Case | 50.52 ± 14.82 | 0.118 | 35.53 ± 13.67 | < 0.0001 | 34.41 ± 13.81 | < 0.0001 |
| Control | 56.51 ± 13.84 | 59.47 ± 12.34 | 60.66 ± 11.28 | ||||
| Physical limitations | Case | 46.08 ± 17.87 | 0.051 | 32.20 ± 17.48 | < 0.0001 | 27.74 ± 14.74 | < 0.0001 |
| Control | 54.73 ± 14.93 | 55.93 ± 13.75 | 59.48 ± 13.15 | ||||
| Social limitations | Case | 47.18 ± 17.48 | 0.005 | 34.60 ± 13.34 | < 0.0001 | 35.33 ± 14.26 | < 0.0001 |
| Control | 60.07 ± 16.27 | 59.08 ± 14.10 | 61.07 ± 14.87 | ||||
| Relationships | Case | 48.86 ± 15.11 | 0.001 | 33.30 ± 14.52 | < 0.0001 | 32.74 ± 14.84 | < 0.0001 |
| Control | 62.46 ± 14.06 | 57.70 ± 13.95 | 57.70 ± 14.67 | ||||
| Emotions | Case | 54.58 ± 11.00 | 0.040 | 43.11 ± 8.47 | 0.002 | 42.19 ± 9.853 | 0.021 |
| Control | 61.86 ± 15.16 | 60.87 ± 12.30 | 63.83 ± 14.37 | ||||
| Sleep/energy | Case | 51.63 ± 14.06 | 0.077 | 33.30 ± 15.79 | < 0.0001 | 31.63 ± 17.70 | < 0.0001 |
| Control | 58.90 ± 16.64 | 59.48 ± 17.22 | 58.90 ± 16.64 | ||||
| Severity measures | Case | 56.35 ± 14.95 | 0.917 | 38.57 ± 15.08 | < 0.0001 | 39.03 ± 16.20 | < 0.0001 |
| Control | 55.92 ± 16.33 | 55.32 ± 15.24 | 58.00 ± 18.21 | ||||
| VAS2 | Case | 4.60 ± 1.35 | < 0.0001 | 3.00 ± 1.74 | < 0.0001 | 3.07 ± 1.17 | < 0.0001 |
| Control | 7.32 ± 1.41 | 7.50 ± 1.23 | 7.39 ± 1.16 |
Compared Data From 3, 6, and 9 Months of Follow-Up Between the Two Groupsa
Repeated measure test showed that total QOL score was significantly better in the cystistat group than in the control group (P < 0.001) by the time of follow-ups (Figure 2A).
The findings demonstrated that at follow-ups times VAS score was significantly decreased in the cystistat group compared to the control group (P < 0.001) (Figure 2B).
The findings also indicated that hematuria score was significantly decreased in the cystistat group (P < 0.001) by the time of follow-ups (Figure 2C).
4.1. Adverse Events
Two participants in the control group and one patient in the case group were involved urinary tract infection during intravesical instillation of agents that were managed with proper antibiotics based on antibiograms from urine culture. One woman from the case group developed bladder stone formation after three months without any previous history and a risk factor that litholopaxy was carried out for her and after that, the patient did not have any complaint.
5. Discussion
The pathogenesis of radiation cystitis damages the GAG layer of the bladder mucosa. This layer protects the bladder wall from toxic agents and microorganisms; therefore, it seems that any defects in this layer cause cystitis symptoms (20). Radiation cystitis is one of the main challenges in urology due to its unknown cause. Different remedial efforts such as radiation dose limitation and adjustment of irradiation field, oral drugs such as orgotein, vitamin E, and steroids trialed, however, were not completely successful in the treatment. The only approved oral therapy for radiation cystitis is Elmiron or pentose polysulfate sodium (17). Intravesical use of bacillus Calmette-Guerin was also utilized for this indication; however, the findings were controversial (21). The other intravesical therapeutic approach tested is constructed on the instillation of dimethyl sulfoxide (DMSO), which is conclusive in the management of many symptoms, but the reality that it is an organic solvent raises worries for its long-time use (21).
Among different therapeutic options, intravesical use of some agents was reported and their response rates were 45% for chondroitin sulfate, 56% for heparin, and 44% for pentosane polysulfate (22).
In this trial, we presented that the use of cystistat; HA; in contrast to the control arm, significantly improved the QOL and VAS and hematuria score after 9 months. HA is a main mucopolysaccharide in the epithelial, connective, and neural tissues and stands for one of the major portions of the extracellular matrix that significantly be conductive to cell proliferation and migration. Moreover, it plays the part of a defensive barrier versus irritating factors that can destroy the epithelium. It might leucocyte migration, suppress immune complexes, and boost modulation of the fibroblasts, proliferation of the endothelial cell, and improvement of the curing tissues. Impairment of the GAG layer may result in direct exposure to components of urine, to bacteria and fungi (17). This injury can lead to radiation cystitis. Therefore, HA can be an option for the treatment of radiation cystitis. Kallestrup et al. (16) reported higher response rates with instillation HA treatment, and the valuable effect was conserved for ≥ 3 years. Morales et al. (23) showed that 71% of the participants who underwent HA instillations, demonstrated improvement of symptoms and disclosing the direct correlation between GAG layers, HA, and control of the IC.
Sommariva et al. (24) prospective trial showed that sodium hyaluronate declines the symptoms of RT-cystitis. Generally, 67 (97%) patients presented complete relief of pain and dysuria.
Engelhardt et al. (25) mentioned that after HA treatment, 50% of the subjects revealed bladder symptom remission without any additional treatment in 5-year follow-up and 41.7% of subjects with symptom recurrence revealed recovery with HA maintenance treatment. Miodosky et al. (26) in their study concluded that HA instillations can show instant benefit in releasing the pain, macroscopic hematuria, and voiding frequency, and acceptable advantageous duration of the treatment. Vassillis et al. (17) showed that the mean score of radiation cystitis before and after the cystistat instillations was 2.70 ± 0.47 and 1.45 ± 0.51, respectively (P < 0.01)17. Pyo and Cho in a meta-analysis showed a significantly positive effect in 6-month follow-up in interstitial cystitis patient (27).
Shao et al. have also demonstrated that intravesical administration of sodium hyaluronate is as influential as hyperbaric oxygen therapy in the management of RT cystitis. In this randomized study of 36 cases with pelvic malignancies, this management plan was well tolerated and resulted in a reducing of pelvic pain, bladder bleeding, and urinary frequency for ≥ 12 months (28).
Kallestrup et al. (16) demonstrated that HA reduced the pain associated with IC, nocturia, and frequency for at least a span of 3 years.
5.1. Conclusions
This was the first study in the Iranian population indicating that patients with radiation cystitis could significantly benefit from HA, and their hematuria would be successfully resolved rather than control group, in addition to lowering the VAS score, so their QOL would be improved. Although the follow-up time was short-midterm for 9 months, the results showed the effect of time in an improving pattern. In view of the HA instillations efficacy and the absence of systemic harm effects, the management of cystistat in radiation cystitis is suggested.
5.2. Limitation and Recommendation
As a limitation, the potential effect of heparin itself on the outcome of the study in both groups can interfere with the study results.
Another study limitations are few numbers of patients in each group and short follow-up of patients, but in addition to these limitations, this study was a RCT and compared all the sub-categories of KHQ of life questionnaire between the two groups; therefore, based on the data, we can candidate patients with radiation cystitis for cystistat instillation according to their most annoying problems decreasing their QOL.