1. Background
The death of a family member due to fatal diseases is one of the most stressful events in a child's life. Childhood cancer is one of these diseases and the second leading cause of mortality, following accidents, in children aged five to 14 years (1). The diagnosis of cancer in children and adolescents is a life-changing event for the family that causes considerable stress for them and exposes all family members to different challenges for resuming or recovering their normal lives (2). The healthy siblings of a child with cancer experience psychological distress during the child's illness and after their death (3) and are thus predisposed to behavioral and emotional problems. There is growing evidence indicating that siblings of children with cancer suffer from significant psychological distress. Internalizing problems such as anxiety and depression and externalizing behavioral problems have been reported. In addition, siblings suffer from problems at school, psychosomatic complaints, lower quality of life, and posttraumatic stress (PTS) (4).
After the sick child dies, their siblings experience an extra loss due to the death of their sibling, while it is accompanied by their mourning parents’ unavailability (5). They commonly project signs such as anger, anxiety, guilt, social isolation, shame, prolonged depression, low self-esteem, sleep disorder, and minimum personality development (6). As an overwhelming, severe, and long-term process, mourning one’s siblings is regarded as a developmental and growth challenge for children that is a major risk factor for psychiatric disorders in childhood and later in adulthood life. Literature review shows a high prevalence of prolonged grief in the relatives of patients with cancer (7). This debilitating and common disease distresses the siblings of the sick child more than any other disease. In the course of the disease, the healthy siblings show adaptive problems (8) and based on Bowlby's clinical experiences and findings (9), many of these adaptive problems (anger, anxiety, and depression) are expressed with greater intensity in mourning after the loss. Therefore, considering the changes in the bereaved siblings, such as changes in personality, attitude toward the future, interest in school assignments, goals, lifestyle, activities, hobbies, anxiety, depression, communication problems, and being at a critical age (10, 11), the loss can hinder development and cause further behavioral and emotional problems in the future if the bereavement issues faced by these children are not specifically targeted and resolved (12).
Nonetheless, many studies have been conducted on bereaved children with an emphasis on the loss of a parent, and very few have examined children with an experience of mourning their siblings (10, 13, 14). The siblings of a deceased child with cancer have similar experiences of the disease as their parents but are often not the center of attention (15). Several methods have been proposed for treating grief disorder based on different approaches. While these interventions often emphasize the importance of talking about the deceased person and feelings of bereavement, children are unable to express their emotions and feelings due to their low level of abstract thinking (16). Some of them avoid talking about their loss to avoid facing reality, pain, and the consequences of the death of their loved ones (17). Using cognitive-behavioral therapy has the least effect on the emotional problems of these children. Moreover, in seeking to treat prolonged grief, the cognitive-behavioral therapy approach does not take into account the intensity of the bereaved children's distress, their cognitive abilities, and developmental differences, which can affect the effectiveness of this therapy (18). In addition to explaining children's behavioral problems, the attachment theory and the body of research on it provide powerful tools for achieving developmental goals and are full of important findings for designing and inventing suitable interventions to facilitate the primary relationships (19).
As an attachment-based play therapy, theraplay is based on Bowlby's attachment theory (1988), in which therapy is regulated where the child's emotional development has stopped, and the process of attachment has disintegrated according to the early stages of the child's development. With one child's illness and their subsequent loss, the surviving siblings have had no chance to form a secure attachment style, and this lack causes many adaptive problems during the illness and the loss. Attachment-based play therapy can assess the feelings and emotions of these children and provide them with positive aspects, warm and compassionate care, a sense of worth, and a response to their needs so as to enable them to regulate their emotions and gain what the child has lost before. This therapy is not based on cognitive representation; rather, it is related to emotions and can be practiced for a wide range of emotional, social, and behavioral problems at different ages from childhood to adulthood (20, 21). The results of a study by Mäkelä and Vierikko (2004) showed that theraplay is effective for both boys and girls in reducing their behavioral and emotional problems, particularly their aggressive behaviors, and this reduction persisted in the follow-up investigations (22). Theraplay seeks to help children regulate their emotions and behaviors and challenge their negative working models (23) with the assumption that this intervention is effective on children suffering from loss, separation, abuse, and neglect.
Since studies show the effectiveness of theraplay on children's psychiatric problems and no studies have yet been conducted on the effect of psychiatric interventions on internalizing and externalizing problems in bereaved siblings, the present study was conducted to determine the effectiveness of theraplay in improving internalizing and externalizing problems in bereaved siblings.
2. Objectives
Accordingly, the object of this study was to investigate the effect of theraplay in improving Internalizing and Externalizing problems in bereaved siblings.
3. Methods
The protocol of the study was approved by the Ethics Committee of the University of Social Welfare and Rehabilitation Sciences (code: IR.USWR.REC.1398.050). This quasi-experimental study utilized a single-subject multiple baseline design. The study population included all the mothers and six to 10-year-old siblings of children with cancer who had received treatment at Mahak Pediatric Cancer Hospital and died in 2017 - 18. The participants were selected through convenience sampling. The siblings of the deceased child with cancer were assessed in terms of the inclusion and exclusion criteria, and four child-mother pairs were ultimately selected as the sample. The most important inclusion criteria for children were T score > 60 in the internalizing and externalizing problems scale of the Child Behavior Checklist (CBCL), the experience of sibling loss due to cancer for at least one year, an age range of six to 10 years, not receiving psychotherapy and medication before or during entering the study and announcing parents' consent for their child to participate in the meetings by completing the consent form. For mothers, experiencing child mourning due to cancer, having a child aged six to 10 years, not receiving other treatments such as parenting training, being biological parents of the child, and living with the spouse and children were the most important criteria. Also, the exclusion criteria from this study for children were having a specific and obvious physical illness during the intervention period and exposure to stressful events during the intervention period that would affect the results and for mothers, they were getting divorced or having a serious decision to divorce all four participants have been the mother as the primary caregiver in their developmental processand they did not have a babysitter and did not go to kindergarten. Only at the time of hospitalization were their sick siblings in the care of friends and relatives, and all four children participating in the study had no other siblings. To determine the baseline, all the children were assessed using the CBCL three times before beginning the intervention at one-month intervals and then attended 15 weekly, 45-min-long, individual sessions. The participants were assessed again using the CBCL in the third, fifth, seventh, ninth, 11th, 13th, and 15th sessions. The first and second follow-up results were obtained two weeks and 1.5 months after the intervention.
3.1. Participants
3.1.1. Participant 1
This nine-year-old girl had lost her identical twin sister due to nephroblastoma in 2017 at the age of seven. Her father was 42-years-old, with an associate degree, and self-employed while her mother was 37-years-old, a bachelor of Law, and a housewife. During the initial interview, the mother stated that she is a quiet, calm, secluded, and shy girl, and is always worried and constantly thinks that "something might happen to her parents and she will lose them". She experienced pain in different parts of her body, the physical cause of which was not determined after numerous visits to the doctor.
Her normative scores were high and within the clinical range in anxious/depressed (75), withdrawn/depressed (70), somatic complaints (68), and aggressive behavior (69). Moreover, her normative internalizing problems score was 76, which was higher than the cutoff point of 63 and within the clinical range.
3.1.2. Participant 2
This 10-year-old boy was the first child of the family. His father was 38-years-old, with a middle school degree, and a newspaper clerk, while his mother was a 30-year-old diplomat and a housewife. During the initial interview, the mother stated that he is a mysterious boy who is very dependent on her, is restless and easily distracted, and has low attention and concentration. In addition, he was stubborn and aggressive, and lied a lot, did not do his personal work alone, and had low social skills, got nervous easily, and fought with others. His younger sister had died of neuroblastoma in 2018 at the age of three. In the initial assessment, he had very high normative scores within the clinical range in anxious/depressed (90), social problems (81), attention problems (90), rule-breaking behavior (82), and aggressive behavior (84). Moreover, his internalizing (82) and externalizing problems (84) T-scores were higher than the cutoff point of 63 and within the clinical range.
3.1.3. Participant 3
This seven-year-old girl was the first child of the family. Her father was 38-years-old, with a diploma, and an installation technician, while her mother was a 32-year-old bachelor of nursing and housewife. The mother stated in the initial interview that she is a shy girl who has a great desire to do things without mistakes; she worries about making a mistake, ruining something, or wasting money, and therefore tries not to do anything that her mother blames, has low self-esteem, and is dissatisfied with her appearance. She lost her younger sister due to synovial sarcoma at the age of one in 2018. In the initial assessment, she had a very high normative score within the clinical range in anxious/depressed (75), thought problems (73), and rule-breaking behavior (73). Moreover, her normative score in internalizing problems (75) was higher than the cutoff point of 63 and within the clinical range. Her normative scores of attention problems (65) and externalizing problems (62) were borderline.
3.1.4. Participant 4
This eight-year-old girl was the second child of the family. Her father was 52-years-old, with a middle-school degree, and self-employed (shopkeeper), while her mother was 40-years-old, level of education was below diploma and a housewife. She was the second child in the family. The mother stated in the initial interview that she is a stubborn, excited, talkative, and irregular girl. She was very afraid of the dark and lonely, had sleep problems and nightmares. She lost her older sister due to glioma in 2017. In the initial assessment, she had high normative scores within the clinical range in anxious/depressed (66), social problems (69), thought problems (68), and rule-breaking behavior (67). Moreover, her normative score in externalizing problems (66) was higher than the cutoff point of 63 and within the clinical range.
3.2. Statistical Analysis
Visual analysis of graphic displays of level, Reliable Change Index (RCI), and clinical significance was used to analyze the data. Data analysis and drawing graphs were performed in Microsoft Excel 2016. Statistical significance was evaluated by the RCI, and the clinical significance was determined by calculating the effect size. In the RCI, the pretest score was subtracted from the posttest score, and the result was divided by the standard error of the difference between the two scores. If the absolute value of the result was equal to or greater than 1.96, it indicated that the obtained result was mostly due to experimental manipulation factors than measurement error (24). The mean baseline reduction (MBLR) method was used to calculate the effect size. In this method, the mean of the treatment or follow-up phase observations is subtracted from the mean of baseline observations, then divided by the mean baseline observations, and the result is multiplied by 100 (25). The formula for calculating effect size at treatment and follow-up stages was as follows:
Effect size = (Mean 100 × Mean baseline observations - Mean treatment or follow-up stages observations) / (Baseline observations)
3.3. Theraplay for the Bereaved Sibling: Therapy Program
Theraplay was an intervention focused on the mother and the child. In addition to the therapy sessions in which both mother and child participated, training sessions for parenting were also held for the mothers. This intervention was designed and performed by the researcher with the guidance of the consulting professor based on the Security Cycle Program (26) and the parenting program using theraplay (27) and play therapy techniques. The protocol consisted of three parts. The first part included play therapy sessions, which were implemented by two trained play therapists. These sessions aimed at creating a secure and peaceful environment for the children to externalize their negative emotions, share memories and feelings, normalize their painful emotions following the death of their siblings, increase their feeling of control over their surrounding events, and increase self-esteem and self-belief. The first session consisted of interviews with the parents for data collection (the interview was focused on the parent-child relationship and attachment). The second session consisted of observations using the Marschak Interaction Method (MIM), in which a parent and a child perform a series of tasks in each other’s presence at the same time. The interactions were recorded and then analyzed by the therapist to prepare for the meeting with the parents. In the third session, the therapist and parents talked about observations of their interactions and then reached an agreement about the therapy objectives (feedback session with the mother). Sessions four to seven specifically addressed emotions of grief, fear, anger, guilt, and loneliness caused by the loss of the sibling. The eighth, ninth, and 10th sessions dealt with wishes and changes following the death of the sibling. The 11th and 12th sessions focused on the concepts of security, secure base, and safe place. The 13th and 14th sessions addressed the child's positive attributes and abilities. The 15th session finalized the course with celebrations and distributing giving prizes. The second part of the protocol included group sessions with the mothers aiming to provide a secure and peaceful environment for the Externalizing of their negative emotions generated by mourning their child, assess their children's problems and parent-child interactions, and also provide attachment-based training in line with the particular needs of their bereaved children. The third part of the protocol consisted of games and homework for the mothers and children to help achieve the specified objectives. The games were partly emotion-oriented and partly relationship-oriented. Theraplay was carried out over 15 weekly 45-min-long sessions at the Mother and Child Clinic of Shahid Beheshti University of Medical Sciences.
3.4. Assessment Tools
3.4.1. Children Behavior Checklist (CBCL)
This checklist is an empirical assessment system containing a series of forms for assessing competence, adaptive functioning, and emotional-behavioral problems (28). In addition to DSM-based scales, CBCL contains two major symptoms, namely internalizing symptoms (including anxious/depressed, withdrawn/depressed, and somatic complaints), and externalizing symptoms (including rule-breaking behavior and aggressive behavior). Its reliability was assessed using test-retest with an eight-day interval, which showed a high correlation for the subscales (0.8 to 0.9) and total problems (0.9). The questionnaire was completed separately by the mothers and fathers, and the scores obtained showed a high correlation between the scores (r = 0.61). The construct validity of the scale was determined based on its predictive relationships and correlations with other scales, such as the behavior checklist of England & Richman (1977; r = 0.56 - 0.77), the child behavioral screening checklist by Mutton-Seaman et al. (1977; r = 0.7), and the aggressive behavior scale (r = 0.47) (29). The present study used scales related to externalizing and internalizing symptoms. Cronbach’s alpha in a range of 0.48 to 0.75 was calculated for the eight subscales in Iran. The findings showed that the Persian version of CBCL had good reliability (30).
4. Results
4.1. Subscales of Internalizing Problems
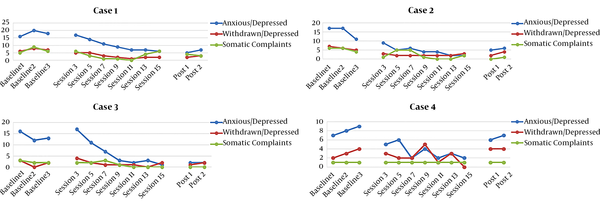
Table 1 presents the scores of subscales of internalizing problems (including anxious/depressed, withdrawn/depressed, and somatic complaints) in the four participants. The results of visual and quantitative data analysis (Figure 1 and Table 1) showed that the subscales of internalizing problems of the four participants had a significant decrease in the intervention period. The significantly decreasing trend of the scores on this subscale in subjects 1, 2, and 3 continued during the follow-up period.
| Variables | Baseline | Therapy | Follow-up | Baseline-Therapy Improvement (%) | Baseline-Follow-up Improvement (%) |
|---|---|---|---|---|---|
| Anxious/depressed; Participant 1 | 18 ± 2.02 | 10.14 ± 1.33 | 6 ± 2.48 | 43.66 | 66.66 |
| Anxious/depressed; Participant 2 | 15 ± 1.49 | 4.57 ± 0.97 | 5.5 ± 1.83 | 69.53 | 63.33 |
| Anxious/depressed; Participant 3 | 13.66 ± 2.81 | 6.28 ± 1.84 | 2 ± 3.44 | 54.02 | 85.35 |
| Anxious/depressed; Participant 4 | 8 ± 0.821 | 3.43 ± 0.538 | 6.5 ± 1.006 | 57.12 | 18.75 |
| Withdrawn/depressed; Participant 1 | 7 ± 0.802 | 2.85 ± 0.525 | 2.5 ± 0.982 | 59.28 | 64.28 |
| Withdrawn/depressed; Participant 2 | 6 ± 0.480 | 2.43 ± 0.314 | 3.5 ± 0.588 | 59.5 | 41.66 |
| Withdrawn/depressed; Participant 3 | 1.667 ± 0.742 | 1.57 ± 0.486 | 1.5 ± 0.909 | 6.54 | 10.71 |
| Withdrawn/depressed; Participant 4 | 3 ± 0.803 | 2.28 ± 0.526 | 4 ± 0.984 | 24 | -33.33 |
| Somatic complaints; Participant 1 | 6.67 ± 1.29 | 3 ± 0.847 | 2.5 ± 1.46 | 55.02 | 62.52 |
| Somatic complaints; Participant 2 | 5.33 ± 1.15 | 1.857 ± 0.756 | 2 ± 2.143 | 65.29 | 65.2 |
| Somatic complaints; Participant 3 | 2.33 ± 0.594 | 1.14 ± 0.389 | 1.35 ± 0.727 | 51 | 42.1 |
| Somatic complaints; Participant 4 | 1 ± 0 | 1 ± 0 | 1 ± 0 | 0 | 0 |
Results of Repeated Measures Analysis of Variance for Participants’ Subscales of Internalizing Problems a
4.2. Anxious/Depressed
The mean baseline scores of the anxious/depressed subscale in participants 1, 2, and 3 were within the clinical range, but reduced to the normal and normative range after the intervention in the follow-up stage. The mean baseline scores of participant 4 were borderline, but fell in the normal range in the follow-up stage.
4.3. Withdrawn/Depressed
According to Table 1, the mean baseline scores of participants 1 and 2 in the withdrawn/depressed subscale (7 and 6, respectively) were within the clinical range, but the intervention brought them to the normal range in this subscale. The percentage of improvement in participant 4 was 24% for this subscale during the therapy and -33.33% in the follow-up period, which means that the score reduced by 24% in the therapy stage compared to baseline but increased by 33.33% in the follow-up period compared to baseline. In this subscale, participant 3 fell within the normal range.
4.4. Somatic Complaints
The mean score of participant 1 in somatic complaints was 6.67 at the baseline, i.e. within the clinical range, but reduced to 3 in the therapy stage and 2.5 in the follow-up stage and fell within the normal range. The mean score of participant 2 was 5.33 at the baseline, 1.857 during therapy, and 2 in the follow-up stage, with effect sizes of 65.29 and 65.2, respectively. After the intervention, the scores of this subscale fell within the normal range in participant 2.
4.5. Internalizing Problems
According to Table 2, which compares the average scores of the participants in different stages, participants 1, 2, and 4 were in a better position in the treatment and follow-up phases than the baseline both in terms of the treatment process and its level. This difference is a reason for the positive effect of treatment in participants 1, 2, and 4. This trend was observed in participant 4 only in the treatment phase and was not observed in the follow-up phase. The effect sizes on this scale in the treatment phase and follow-up of Internalizing problems were 50 and 62.1% for the first participant, 69.61, 52.52% for the second participant, 49.4 and 80.19% for the third participant, and finally 44.91 and 4.16% for the fourth participant. That is, the treatment was more effective in participants 1 and 2.
| Participant | Baseline | Treatment | Follow-up | Effect Size (Percentage of Recovery) | Significance | ||
|---|---|---|---|---|---|---|---|
| Baseline - Treatment | Baseline - follow-up | Absolute Value | Significance | ||||
| Participant 1 | 31.67 ± 3.48 | 16 ± 2.27 | 12 ± 4.26 | 50 | 62.1 | 3.72 | Significant |
| Participant 2 | 26.33 ± 2.52 | 8 ± 1.65 | 12.5 ± 3.09 | 69.61 | 52.52 | 5.82 | Significant |
| Participant 3 | 7.66 ± 3.81 | 9 ± 2.5 | 3.5 ± 4.67 | 49 | 80.19 | 1.86 | Not significant |
| Participant 4 | 12 ± 1.41 | 6.71 ± 0.925 | 11.5 ± 1.73 | 44.91 | 4.16 | 3.14 | Significant |
| Total | 21.92 ± 1.96 | 10.14 ± 1.28 | 9.87 ± 2.41 | 53.79 | 54.97 | 5 | Significant |
Repeated Measurement Results of Internalizing Problems a
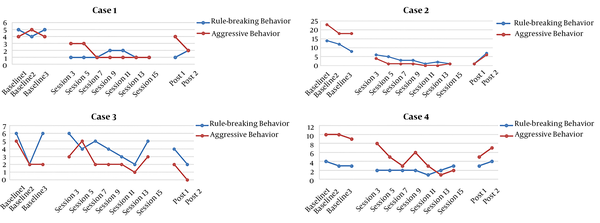
Subscales of Externalizing problems: Table 3 presents the scores of subscales of externalizing problems (including rule-breaking behavior and aggressive behavior) in participants 1 to 4. Generally, the results showed that theraplay could reduce the subscales of externalizing problems.
| Variables | Baseline | Therapy | Follow-up | Baseline-therapy improvement (%) | Baseline-follow-up improvement (%) |
|---|---|---|---|---|---|
| Rule-breaking behavior; Participant 1 | 4.67 ± 0.310 | 1.29 ± 0.203 | 1.5 ± 0.380 | 72.37 | 67.88 |
| Rule-breaking behavior; Participant 2 | 11.33 ± 1.64 | 4 ± 1.07 | 4 ± 2.01 | 64.69 | 64.69 |
| Rule-breaking behavior; Participant 3 | 4.67 ± 0.933 | 4.14 ± 0.611 | 3 ± 1.14 | 11.34 | 35.76 |
| Rule-breaking behavior; Participant 4 | 3.33 ± 0.342 | 2 ± 0.224 | 3.5 ± 0.419 | 39.94 | -5.1 |
| Aggressive behavior; Participant 1 | 4.33 ± 0.557 | 1.57 ± 0.365 | 3 ± 0.682 | 63.74 | 30.72 |
| Aggressive behavior; Participant 2 | 19.68 ± 1.49 | 1.88 ± 0.976 | 3.5 ± 1.83 | 90.44 | 82.21 |
| Aggressive behavior; Participant 3 | 3 ± 0.810 | 2.57 ± 0.530 | 1 ± 0.992 | 14.33 | 66.66 |
| Aggressive behavior; Participant 4 | 9.68 ± 1.2 | 4 ± 0.783 | 6 ± 1.46 | 58.68 | 38.01 |
Results of Repeated Measures Analysis of Variance for Participants’ Subscales of Externalizing Problems a
4.6. Rule-Breaking Behavior
The score of participant 1 for rule-breaking behavior was within the clinical range at baseline. According to Table 3, the score of this subscale reduced after the intervention and reached 1.5 in the follow-up stage, which was within the normal range. Although the mean scores in this subscale were reduced in participants 2 and 3, they still remained within the clinical range. In participant 4, the rule-breaking behavior scores reduced by 39.9% in the therapy stage and increased by 5.1% in the follow-up compared to baseline.
4.7. Aggressive Behavior
According to Table 3, the percentage of improvement in this subscale was 63.74% during therapy and 30.72% in the follow-up stage for participant 1, 90.44 and 82.21% for participant 2, 14.33, and 66.66% for participant 3, and 58.68 and 38.01% for participant 4, respectively. In other words, therapy was more effective in participants 1 and 2. According to the visual analysis (Figure 2) and the interpretation of Table 3, the scores were positive for participants 1 and 2, in the follow-up stage for participant 3, and during therapy for participant 4, and the descending trend of the mean score of aggressive behavior after therapy confirmed this claim.
4.8. Externalizing Problems
According to Table 4, which shows the average scores of the participants in the baseline, treatment phase, after treatment, and follow-up, participants 1, 2, and 4 were in a better position in terms of the treatment process and its level in the treatment, post-treatment, and follow-up phases than the baseline. This difference is a reason for the positive effect of treatment in participants 1, 2, and 4. This trend was observed in participant 3 only in the follow-up phase, and no decreasing trend was observed in the treatment phase. The effect sizes on this scale in the treatment phase and follow-up of externalizing problems were 68.33 and 50% for the first participant, 77.74 and 71.51% for the second participant, 12.4 and 47.78% for the third participant, and finally 64.66 and 58% for the fourth participant. That is, the treatment was more effective in participants 1, 2, and 4.
| Participant | Baseline | Treatment | Follow-up | Effect size (Percentage of Recovery) | Significance | ||
|---|---|---|---|---|---|---|---|
| Baseline - Treatment | Baseline - Follow-up | Absolute Value | Significance | ||||
| Participant 1 | 9 ± 0.445 | 2.85 ± 0.293 | 4.5 ± 0.546 | 68.33 | 50 | 11.43 | Significant |
| Participant 2 | 26.33 ± 3.05 | 5.86 ± 1.99 | 7.5 ± 3.73 | 77.74 | 71.51 | 7.46 | Significant |
| Participant 3 | 7.66 ± 1.52 | 6.71 ± 0.993 | 4 ± 1.85 | 12.4 | 47.78 | 0.531 | Not significant |
| Participant 4 | 13 ± 1.25 | 6 ± 0.821 | 9.5 ± 1.54 | 53.84 | 26.92 | 4.654 | Significant |
| Total | 15.17 ± 1.67 | 5.36 ± 1.09 | 6.37 ± 2.05 | 64.66 | 58 | 4.687 | Significant |
Repeated Measurement Results of Externalizing Problems a
5. Discussion
The analysis of the data showed that theraplay had a considerable effect on reducing internalizing and externalizing problems in bereaved siblings. Most participants experienced a high effect size in the internalizing and externalizing problems' subscales.
It appears that this course of treatment has been effective in reducing the internalizing problems and externalizing problems in bereaved siblings by increasing the awareness of emotions, reducing physical tension, and training parents to provide care and contact along with its effects on agitation in children, facilitating the release of negative emotions in children, calming them after emotional release, reducing the feeling of loneliness regarding negative emotions such as remorse, guilt, and anger, accepting the loss, and regaining strength.
In general, the anxiety/depression scores of four participants in the follow-up stage decreased compared to the baseline, and the scores of all participants in the follow-up stage were in the normal range. The results of the study also showed that the present intervention had a significant decrease in the withdrawal/depression scores of participants 1 and 2. The scores of these subjects were in the clinical domain before the intervention, which was in the normal range after participating in treatment sessions. In the participants, three scores of isolation/depression in the intervention and follow-up stages were slightly different from the baseline and were in the normal range in all stages of treatment. Participant 4 scores in this subscale increased relative to baseline in the follow-up phase, but scores were still within the normal range. According to the mean scores of the participants, participants 1, 2 and, 3 were in a better position in the treatment and follow-up periods than the baseline, and this difference was a reason for the positive effect of treatment in participants 1 and 2 and to some extent participant 3. This trend was observed in subject 4 only in the treatment phase and was not observed in the follow-up phase. Also, according to the research findings, physical complaints in participants 1 and 2 significantly decreased, and the scores of this subscale were in the normal range after the intervention, and in the case of participant 3, this decrease was moderate. Participant 4 scores of physical complaints were also in the normal range at all stages of baseline, treatment, and follow-up (Figure 1 and Table 1).
In general, externalized behaviors decreased significantly in three participants, slightly decreased in the third participant in the intervention stage, and increased in the fourth participant in the follow-up stage. According to the results of the research, the rule-breaking behavior of the three participants (first, second, and third participants) in the intervention and follow-up phases significantly decreased, but in the follow-up phase, we saw an increase in the rule-breaking behavior of the fourth participant compared to the baseline. Aggressive behavior also decreased in all four participants (Figure 2 and Table 3).
Mahmoodi-Gharaei et al. (31) used a play therapy model in three- to six-year-old survivors of the Bam earthquake. According to the study, group play therapy focused on the symptoms of bereavement and damage could be effective in reducing depression, behavioral symptoms, and symptoms of posttraumatic stress disorder (PTSD) (31). Ogawa et al. (32) also showed that play therapy is an effective intervention for children with an experience of loss or damage and children with PTSD. These results can be explained by noting that the unexpected death of a child disturbs the parents' life and exposes them to significant challenges (33). Under such circumstances, they may focus on themselves and be less responsive to the needs of the surviving siblings due to their intense preoccupation with the deceased child (34).
Waters et al. (35) explained that life events such as death can affect a child's secure attachment in many ways. Working models may have to be re-evaluated in response to real changes in the caregiver's accessibility and responsiveness. The stress generated by life events can hinder the caregiver’s accessibility and responsiveness. Moreover, they may change the child's expectations from the caregiver's accessibility and responsiveness. Death is a stressful life event that entails varying degrees of emotions for children and consequently activates their attachment-behavioral system. In these situations, children seeking peace and support from their caregivers may find them emotionally less available and may even be rejected by them because the caregivers are trying to manage their own feelings. The changes in the caregivers' availability may cause children to re-evaluate their internal working models and reach the conclusion that they have to manage their feelings alone and without access to caregivers. The ultimate outcome of this complex psychological process is internalizing and externalizing problems (35).
The death of a child with cancer can disintegrate the parent-child relationship, and this disintegration induced by loss is harmful. Theraplay involves the caregivers in the process of therapy, and their broken relationships can thus be mended or new relationships can be developed. Moreover, this intervention creates a safe haven for the bereaved child by creating a fostering parent-child relationship in which the child feels wanted and worthy and enables them to develop their own unique character and personality (23). According to other research findings, the fourth subject's internalizing scores decreased in the treatment phase compared to the baseline, but reached the baseline in the follow-up stage and remained at the same level. Also, the externalizing behaviors of the third subject decreased slightly in the intervention phase and increased in the second and fourth subjects in the follow-up phase. Increasing problems in the follow-up stage and the high variability of some subjects' scores can be explained in two ways. First, we can examine it from the perspective of the family system approach, in which the death of a family member affects the dyad relationships and the role function of members and the family as a whole (36). Thus, the process of bereaved sibling adjustment is directly affected by mourning, but changes in family relationships (mother-child relationship), the role of surviving sibling (parental protection, role reversal), and effects of parenting changes (changes in parenting behaviors) can indirectly affect their adaptability (36). The most important factors affecting adjustment problems of siblings are changes in parenting behaviors (37), severe emotional distress, and internalizing problems such as depression, anxiety, and post-traumatic stress disorder, especially for mothers (38), all of which are listed as challenges for open and warm communication with their bereaved children (4). This condition also reduces mothers' patience, tolerance, energy, and generally speaking, their parenting capacity due to their mourning, making it difficult for them to balance their personal mourning with the needs of their children (39, 40). Thus, to reduce emotional distance, the bereaved siblings get involved in alternative strategies, including externalizing, aggressive, and controversial behaviors (4). Although fathers' internalizing symptoms are not significantly related to parenting behavior changes or parent-children relationships, the bereaved siblings perceive the emotional distance and the least openness to their fathers, and it can play a role in their adaptability problems (41, 42).
The second way of explaining the increase in the scores of the subjects is the relationship of parents. Research shows that families with children with cancer undergo substantial changes after their child dies (4). Some marriages get tighter, and others lose. Bereaved parents report lower marital satisfaction, lower sexual intimacy, greater separation thoughts, and higher divorce rates than non-bereaved parents (43). Due to the characteristics of the families of the third and fourth subjects, the disturbed psychological climate of the family and the parental conflicts that may lead to numerous disputes at home disturbed the stability and peace of these children. The cases highlight the importance of parental adjustment to loss when the target group is bereaved sibling. Decreasing bereaved mothers' distresses, emotional support for parents as the main caregivers of children, and the use of appropriate psychological interventions for the marital conflicts of distressed parents can lead to greater adjustment of bereaved siblings (39-44).
The present study had some limitations. Random sampling was not feasible, and a convenience sampling method was employed, and the sample size was small. Many factors can predict the consequences of bereavement in children, and several causes can lead to prolonged behavioral and emotional reactions in children. Although theraplay had positive results for children and reduced many of the behavioral and emotional problems of children, after the intervention, some problems did not change significantly, and some of the problems that had been reduced during the intervention process has intensified in the follow-up stage again. Factors affecting the persistence of symptoms of mourning in children include the child's gender, length of the absence, the severity of problems, social support, etc., which were not considered in this study. Therefore, the complete and profound recovery of internalized and externalized problems and the long-term grief syndrome of bereaved children requires comprehensive interventions in the set of factors affecting the persistence of grief symptoms. An intervention that can cover the most effective factors at the level of parents and family. Therefore, the use of theraplay as the only treatment for behavioral and emotional problems of these children will face significant limitations. Future studies can address the role of supportive factors such as personal characteristics, family, and lack of issues in Iranian children's grief reactions and design interventions based on the individual and family circumstances of bereaved individuals to determine which treatment is most appropriate and effective.
It is suggested that the study be repeated with a larger sample size and random sampling. Furthermore, the implementation of the current intervention in three groups, one group comprising only mothers, another group comprising only children, and the third group including mothers and children, and comparing the three groups can elucidate the effects of the intervention more accurately.
5.1. Conclusion
In general, theraplay appears to be effective in reducing internalizing and externalizing problems in bereaved siblings, and the therapy protocol used in the present study provides an appropriate model for dealing with these children. Therefore, theraplay can be considered an attachment-based play therapy to help children accept the loss of loved ones and their mourning and can be used for improving children's mental health.