1. Background
Suicide is a critical issue globally, posing significant public health challenges. The 2019 World Health Organization (WHO) report indicates that suicide accounts for approximately 700 000 deaths annually (1). Factors contributing to the underreporting of suicide statistics include societal stigma directed at individuals who have attempted suicide or families of those who have died by suicide (2), the criminalization of suicide and suicide attempts in certain countries (3), and the absence of insurance coverage for individuals seeking treatment after a suicide attempt (4). Consequently, the estimated number of suicide attempts is much higher, believed to be around 20 times the number of completed suicides (2, 3). Suicidality is multifaceted, with social, psychological, cultural, and economic factors playing roles in its onset. Notably, mental illnesses (especially depression and alcohol misuse), a family history of suicide, financial setbacks, or chronic pain significantly increase the risk of suicidal behavior (4-6).
Particularly during severe crises and the COVID-19 pandemic, many individuals refrain from seeking help due to the stigma associated with mental health issues and suicidality (7). Link and Phelan conceptualize societal stigma through interconnected components: labeling those affected as different, applying stereotypes, creating a division between "us" and "them," leading to loss of status and ensuing discrimination, drawing on sociologist Goffman's definition of stigma (8, 9).
In the context of suicide stigma, having suicidal thoughts is perceived as a distinguishing trait, separating affected individuals from others. This label is linked to negatively perceived stereotypes, such as the belief that "suicidal individuals lack willpower," fostering adverse emotional reactions and annoyance towards this group. Such processes underpin the segregation between “us” and “them,” paving the way for discrimination, such as avoiding or disregarding individuals dealing with suicidality (10, 11).
Barriers to suicide prevention are significantly influenced by suicide stigma (negative attitudes and behaviors towards individuals who have attempted suicide) and suicide literacy (general awareness about suicide prevention) (12). Individuals with higher levels of suicide literacy and lower levels of suicide stigma tend to have more positive attitudes towards those contemplating suicide (13). Several studies have highlighted the detrimental effects of suicide stigma, such as increasing the risk of suicide (14, 15), diminishing help-seeking behavior and engagement with professional services (16, 17), and fostering negative perceptions of mental health service utilization (8, 18). These adverse impacts have positioned suicide stigma as a primary target for suicide prevention initiatives. Moreover, inadequate suicide literacy can negatively influence individuals experiencing suicidal thoughts or behaviors. Those harboring misconceptions and incorrect beliefs about risk factors, symptoms, and outcomes of suicide are more prone to suicidal ideation or attempts, particularly in contexts where suicide is glorified and stigma is prevalent. Insufficient literacy also impedes the pursuit of professional services and reduces interactions with mental health professionals (19, 20).
While the link between mental illness and susceptibility to suicide is often underscored, stigmatizing attitudes and suicide literacy also play a critical role in shaping suicidal thoughts and behaviors (13). Consequently, various scales have been developed and validated globally in recent years to specifically address suicide-related stigma and enhance suicide literacy, including the Suicide Stigma Assessment Scale (SSAS) (11), the Stigma of Suicide Attempt Scale (STOSA), the Stigma of Suicide and Suicide Survivor Scale (STOSASS) (21), and the Literacy of Suicide Scale (LOSS) (13).
The trend of suicide deaths in Iran has been on the rise, with recent decades witnessing the most significant increases among countries in the Eastern Mediterranean Region (EMR) and Islamic nations. In Islamic cultures, suicide is considered forbidden. However, the actual rate of suicide attempts might be underreported due to religious or cultural stigma and legal implications (22). Iran's national policies have been insufficiently effective in preventing suicide, necessitating immediate action (16). These circumstances contribute to the taboo surrounding suicide, making it a less discussed topic. In recent years, Iran's healthcare system has initiated a national suicide prevention program primarily focused on education and awareness, yet research on suicide stigma and literacy within Iran has been limited, mostly exploring the experiences of those who have survived suicide attempts (23-25). The availability of reliable and valid instruments to measure these two aspects can enhance the understanding of suicide-influencing factors.
The Stigma of Suicide Scale (SOSS) and LOSS were created to assess these aspects globally (8, 13). The short forms of the SOSS and LOSS scales are straightforward and easily administered within the general population. The brevity of these questionnaires facilitates their use in large-scale screenings by various stakeholders. These questionnaires have been translated into multiple languages, including English, Turkish, Chinese, German, Nepali, and Arabic, with reported high validity and reliability (20, 26-30). These scales were initially validated using a university-based sample.
2. Objectives
This study explored the validity of these scales' short versions within a community sample, aiming to adapt them for use in the Persian language and culture.
3. Methods
A cross-sectional study was undertaken, gathering data as part of an initiative aimed at evaluating suicide literacy, stigma, and associated factors among online social media users from June to August 2022. The finalized Persian short forms of the SOSS and LOSS were distributed via four selected platforms: WhatsApp, Telegram, Instagram, and Twitter. The survey was facilitated by Porsline, an Iranian company specializing in survey administration software. Eligibility criteria included being 18 years or older, possessing the ability to read and write, residing in Iran, and expressing a willingness to participate. The initial page of the survey clearly stated the study's objectives. The subsequent page provided details on the eligibility criteria and consent form. Access to the survey was granted only to those who met the criteria and provided consent. Incomplete questionnaire submissions were excluded. Participants were recruited through convenience sampling. Prior studies indicated that a sample size of at least 250 was necessary for confirmatory factor analysis (CFA) (31). This study's sample size was 240.
3.1. Measures
3.1.1. Demographic Questionnaire
Demographic questions were posed to collect information about the participants, including gender, age, marital status, level of education, occupation, and place of residence, along with inquiries regarding personal history of suicidal thoughts and family history of suicide attempts.
3.1.2. The Literacy of Suicide Scale-Short Form
The original LOSS comprises 26 items. The short form, known as the Literacy of Suicide Scale-Short Form (SOSS-SF), was created by Batterham et al. (13) and applied to a sample from an Australian university. This version of the questionnaire, with 12 items, assesses suicide literacy across four domains: The causes or nature of suicide, risk factors, signs and symptoms, and treatment and prevention strategies. Respondents can answer these items with "true," "false," or "I don't know." Correct responses receive a score of 1, while incorrect or "I don't know" responses are scored 0, leading to a total score ranging from 0 to 12. The validity and reliability of this questionnaire have been established in various studies, with internal consistency deemed acceptable (Cronbach’s α: 0.64–0.78). Additionally, the scale demonstrates strong construct validity (Appendix 1) (26-29).
3.1.3. The Stigma of Suicide Scale-Short Form
The original SOSS contains 58 items. Its short form, devised by Batterham et al. (8), features 16 items that portray individuals who commit suicide. To complete this scale, participants indicate their level of agreement with each statement using a five-point Likert scale, ranging from "completely disagree" (scored as 1) to "completely agree" (scored as 5). This scale includes three subscales: Stigmatization, isolation or perceived depression, and normalization or glorification of suicide. The score for each subscale is the average of responses to its items, with scores spanning from one to five. An average score above three suggests concurrence with the specified concept. The internal consistencies of the original SOSS’s three subscales, as measured by Cronbach’s alpha, are 0.95, 0.90, and 0.88, respectively, with an overall scale consistency of 0.93. Previous research on the SOSS questionnaire indicated an intraclass correlation coefficient (ICC) of 0.90 in repeated measurements, affirming its reliability (P = 0.000). Moreover, the SOSS-SF is recognized for its robust construct validity (Appendix 2) (13).
3.2. Procedure
3.2.1. Translation and Adaptation of the SOSS-SF and LOSS-SF
The WHO guidelines (32) were followed for the translation and cultural adaptation of the two questionnaires. Initially, permission was obtained from the original authors of both questionnaires. Subsequently, the questionnaires were independently translated into Persian by two experts from the project team. Afterward, the Persian version was back-translated into English by a translator proficient in English, who was not aware of the original English version. A panel of five psychiatrists then reviewed all versions alongside the original scale for similarity in meaning, clarity, and ensuring conceptual, semantic, and content equivalence. Any discrepancies were discussed, leading to the compilation of the final version. Both scales underwent qualitative content and face validity checks. To assess face validity, feedback from 10 participants and a group of experts was gathered. The expert team also evaluated qualitative content validity. During this process, for item four of the LOSS-SF, which states, “there is a strong relationship between alcoholism and suicide,” the term “substance and alcohol use” was used instead of “alcoholism” to better reflect concerns in Iran, where substance use is a significant risk factor for suicide attempts (33).
3.3. Ethical Considerations
Authorization to validate the instruments was obtained from the authors (8, 13), followed by ethical approval from the Research Ethics Committee of the University of Social Welfare and Rehabilitation Sciences (approval ID: IR.USWR.REC.1401.097) on September 21, 2022. Potential participants were informed about the study's purpose, and written consents were collected.
3.4. Statistical Analysis
To assess the reliability of the questionnaires, internal consistency and test-retest methods were utilized. Cronbach’s alpha was used to evaluate internal consistency, while intraclass correlation (ICC) assessed stability. Confirmatory factor analysis was conducted to investigate construct validity, employing statistical indices such as goodness of fit index (GFI), adjusted goodness of fit index (AGFI), and comparative fit index (CFI) to evaluate model fit. Descriptive statistical tests, including mean, standard deviation, and frequency tables, were conducted to describe participant characteristics. All analyses were performed using SPSS software (Version 24) and AMOS.
4. Results
The sample included the first 240 respondents: 54.8% were female, with an average age of 35.7 years; 56.9% were married, and 87.6% had a university degree (Table 1). The Kolmogorov-Smirnov test and q-q plots were utilized to check data normality. Outliers were examined prior to statistical analysis, with funnel plots assessing outlier data. The large sample size was chosen to manage missing data effectively, as missing data can reduce sample size, posing issues in CFA; thus, a missing data replacement method using the variable mean was employed.
| Variables and Category | Values a |
|---|---|
| Sex | |
| Female | 131 (55) |
| Male | 109 (45) |
| Marital status | |
| Single | 81 (36) |
| Married | 136 (56.9) |
| Divorce | 3 (1.3) |
| Widow | 2 (0.8) |
| In intimate relation | 13 (5.4) |
| Education | |
| Diploma or above | 29 (13.1) |
| Bachelor | 85 (35.6) |
| Master | 74 (30.5) |
| Ph.D. or above | 52 (21.8) |
| Residentialarea | |
| City | 236 (98) |
| Village | 4 (2) |
| Occupation | |
| Student | 38 (15.5) |
| Housewife | 22 (9.2) |
| Unemployed | 11 (4.6) |
| Governmental sector | 71 (30) |
| Private sector | 98 (32.3) |
| History of suicide thought | |
| Yes | 120 (50) |
| No | 120 (50) |
| Family history of suicide attempt | |
| Yes | 45 (18) |
| No | 195 (82) |
Sociodemographic Variables of Participants (n = 240)
The results indicated good internal consistency and reliability for the scales. Cronbach’s alpha for the suicide literacy scale was 0.76, and for the suicide stigma scale, it was 0.79. The internal consistency for the subscales was as follows: stigmatization (α: 0.75), isolation/depression (α: 0.81), and normalization or glorification (α: 0.78). The ICC, calculated through test-retest after participants completed the questionnaires initially and again two weeks later, was 0.81 for suicide literacy and 0.75 for suicide stigma, confirming the scales' reliability as satisfactory.
The construct validity of the SOSS-SF was assessed through CFA, employing principal component extraction and varimax rotation. Table 2 presents the results of the CFA, indicating that the model predicting the three subscales of the questionnaire fits the sample excellently, with all factor loadings being statistically significant.
| Dimensions and Items | Squared | Factor Load |
|---|---|---|
| Stigma | ||
| Cowardly | 0.52 | 0.76 |
| An embarrassment | 0.52 | 0.76 |
| Immoral | 0.46 | 0.70 |
| Irresponsible | 0.59 | 0.78 |
| Pathetic | 0.50 | 0.71 |
| Shallow | 0.71 | 0.76 |
| Stupid | 0.66 | 0.72 |
| Vengeful | 0.78 | 0.82 |
| Isolation | ||
| Disconnected | 0.48 | 0.73 |
| Isolated | 0.51 | 0.68 |
| Lonely | 0.66 | 0.72 |
| Lost | 0.58 | 0.74 |
| Glorification | ||
| Brave | 0.74 | 0.64 |
| Dedicated | 0.59 | 0.81 |
| Noble | 0.27 | 0.69 |
| Strong | 0.78 | 0.83 |
Psychometric Characteristics of the Stigma of Suicide Scale-Short Form (SOSS-SF)
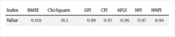
Table 3 displays goodness-of-fit indices, showing CFI, GFI, and RMSEA values at 0.97, 0.98, and 0.021, respectively. These indices validate the model's fit.
| Index | RMSE | Chi-square | GFI | CFI | AFGI | NFI | NNFI |
|---|---|---|---|---|---|---|---|
| Value | 0.021 | 18.5 | 0.98 | 0.97 | 0.96 | 0.97 | 0.96 |
Confirmatory Factor Analysis of Fit Indices of the Stigma of Suicide Scale-Short Form (LOSS-SF)
For the LOSS-SF, Table 4 outlines the CFA results and the goodness-of-fit indices. The analysis aimed to verify if the 12 items corresponded to 3 dimensions. The findings, detailed in Table 4, confirm the model's appropriateness for the sample under study.
| Index | RMSE | Chi-square | GFI | CFI | AFGI | NFI | NNFI |
|---|---|---|---|---|---|---|---|
| Value | 0.03 | 22.5 | 0.91 | 0.91 | 0.86 | 0.91 | 0.88 |
Confirmatory Factor Analysis of Fit Indices of the Literacy of Suicide Scale-Short Form (LOSS-SF)
5. Discussion
This study's goal was to translate the SOSS-SF and LOSS-SF into Persian and assess their validity and reliability within the Iranian general population, noting the need for shorter instruments to swiftly screen for suicide stigma and literacy. To our knowledge, this is the first examination of the validity and reliability of SOSS-SF and LOSS-SF in an Iranian context. The original LOSS underwent modification by Jafari et al. (34) in Persian, removing one item, resulting in a 25-item final questionnaire common to both the original and shortened LOSS forms. In our study, this item was retained, with only a minor modification to one question in the LOSS-SF. Factor loading values for all items exceeded 0.4, affirming the LOSS-SF's reliability, comparable to the adapted 25-item LOSS in Persian. The findings suggest that the short forms of these two scales exhibit commendable psychometric properties. The factor structure was validated within a representative sample of Iran's adult population.
In this sample, the SOSS-SF and LOSS-SF subscales demonstrated acceptable internal consistency, with Cronbach's alpha values of 0.79 and 0.76, respectively. A related study in Jordan, a predominantly Muslim country, explored the psychometric responses of university students to the Arabic versions of the SOSS-SF and LOSS-SF. This research identified a general lack of literacy in identifying signs, symptoms, and risk factors of suicide. Jordanian students scored the isolation subscale of the SOSS-SF highest, indicating a tendency to associate suicide more with depression or social isolation than with glorification or stigmatization (26).
This study confirms that both scales are suitable for use in the general population, aligning with findings from a telephone survey in Germany (20). While the participants predominantly consisted of university-educated individuals, these results can likely be extrapolated to an educated demographic as well. This is supported by similar studies conducted with university students in Australia (13), Jordan (26), and Nepal (30). The reliability analysis using Cronbach's alpha revealed acceptable consistency across all three SOSS-SF subscales (stigma, isolation, and glorification), indicating appropriate inter-variable relationships within the scale. For the LOSS-SF, all four subscales (causes, risk factors, signs, and symptoms, treatment, and prevention) displayed satisfactory Cronbach's alpha values. Confirmatory factor analysis validated the construct validity of both scales, with both demonstrating acceptable fit indices. A similar methodology was employed in the study of the Arabic version (26), which also achieved acceptable levels of construct validity.
This study evaluated the psychometric properties of the short forms of the SOSS and the LOSS, establishing norms for their application within the Iranian general population. Despite its contributions, the study faced several limitations. Firstly, the use of convenience sampling might affect the generalizability of the findings and compromise sample representativeness. Given the relatively small sample size, future research should consider larger participant groups to enhance the robustness of findings. Secondly, due to restrictions in Iran at the time of the study, only WhatsApp and Instagram were accessible, potentially overlooking individuals with limited social media literacy or access. Efforts were made to include a wide range of demographic characteristics to mitigate this limitation. Future studies could focus on specific groups, such as healthcare workers or individuals with certain mental health conditions since this study's sample consisted of the general population. Additionally, the cross-sectional design limits the ability to assess various reliability aspects, including test-retest reliability.
5.1. Conclusions
This research aimed to validate the Persian short forms of the SOSS and LOSS within a general population context, successfully demonstrating their acceptable psychometric properties. The LOSS-SF and SOSS-SF scales can be utilized by healthcare professionals, including doctors, psychiatrists, psychologists, and social workers, to measure suicide stigma and literacy among patients and their families and to tailor educational interventions for those harboring stigmatized beliefs or possessing insufficient literacy. Investigating stigmatizing attitudes and suicide literacy at the community level enables researchers and policymakers to implement evidence-based, macro-level strategies and develop comprehensive plans aimed at eradicating stigmatizing attitudes and correcting misconceptions.