1. Background
Body image is a multidimensional construct, encompassing how an individual perceives, thinks, feels, and acts toward one’s own physical appearance (1). Body image dissatisfaction has dramatically increased in modern society due to emphasis on physical appearance (e.g., slender female bodies and muscular male bodies) as a criterion of physical attractiveness and social acceptance. Many compensatory measures (e.g., cosmetic surgeries) attempt to create an ideal mental image (2). High perceptual dissonance with sociocultural ideals and negative attitude toward oneself causes shame of one’s physical appearance and, consequently, results in mental and physical disorders (3, 4).
Shame is a multifaceted and self-conscious emotion that has a significant impact on a sense of self, well-being, and vulnerability to mental disorders (4-7). The painful feelings of shame are strongly associated with social and health problems (8). Research shows that shame considerably contributes to the development and persistence of some disorders, such as body dysmorphic disorder and eating disorders (9-11).
Although there is no consensus on the definition of shame, it involves two components of internal and external shame. Internal shame originates from inside the self and negatively evaluates oneself as a bad, defective or deficient person. It encompasses self-criticism and negative self-evaluation (12). External shame relates to feelings and thoughts about what others think. In the external shame, a person wants to know how he looks like in the others’ mind. It perceives an unattractive self who is more likely to be rejected by others or is vulnerable to attacks by others (13).
Body Image Shame (BIS) encompasses perceptions of being negatively judged and evaluated by themselves and others for their physical appearance (4, 14). BIS stems from internal or external sources. Internal BIS arises in response to negative self-evaluations of physical appearance (4). External BIS arises from the anticipation of social evaluation and rejection of one’s appearance (4, 15). Internal BIS has a central role in some people with body dysmorphic disorder (BDD), especially in those cases with BDD that deformed organs are not visible (e.g., genitalia) (11). External body image in cases with BDD typically causes social isolation (16). Body image shame seems to be more associated with eating and body image disorders than general shame (14, 17).
Given the role of shame in body image-related problems, various measures were used for the assessment of BIS, including body-focused guilt and shame scale (18), body image guilt and shame scale (BIGSS) (19), the experience of shame scale (subscale of body image shame) (20), the objectified body consciousness scale (body shame subscale) (21), Weight-and Body-Related Shame and Guilt Scale (WEB-SG) (22), and the Derriford Appearance Scale (23). These measures are used in certain populations. Some tools are not just about shame; they also measure other conscious emotions. These measures do not assess the internal and external body shame separately. The Body Image Shame Scale (BISS) was designed by Duarte et al. (4). It only measures BIS. Also, BISS measures both internal and external shame compared to the other scales. The BISS has been used in past studies (17, 24-26).
Given the role of body image shame in body-related psychological problems, high prevalence of body image dissatisfaction and high rate of plastic and cosmetic surgery in Iran (27), the absence of a standardized and short-form scale for assessment of body image shame and its components are highlighted in research and clinical projects in Iran.
2. Objectives
The present study aimed to assess factor structure and psychometric properties of the body image shame scale in the individuals visiting cosmetic surgery clinics.
3. Methods
3.1. Participant
In this study, we included the individuals that visited cosmetic surgery clinics in Tehran in 2019. The required sample size for the confirmatory factor analysis is about 200 samples (28). Thus, the participants were considered 409 (136 men, 33.3 %, and 273 females, 66.7%) among the individuals that visited cosmetic surgery clinics in Tehran via convenience sampling. The age range of the study participants was 15 to 54, with a mean ± standard deviation (SD) of 25.88 ± 6.42 years old. The marital status of the participants was as follows: single 317 (77.5 %) and married 92 (22.5 %).
3.2. Procedure
In order to conduct the research, the BISS was initially prepared based on the guidelines for cross-cultural adaptation of measures (29, 30). Accordingly, firstly, the original version of the BISS was translated from English into Persian language by three professors in clinical psychology. Then the items were translated from Persian to English by two other mental health professionals who were fluent in English and Persian. In the next step, the final translation was reviewed by the authors and to check that the scale is acceptable and understandable. Furthermore, in a pilot study, the scale was performed on a sample of 20 individuals who referred to cosmetic surgery clinics to examine if the scale was understandable for them, afterwards problems in the questions were corrected. After preparing the scale, we went to cosmetic surgery clinics in Tehran, and each sample was selected based on the inclusion and exclusion criteria. The inclusion criteria were the individuals visiting cosmetic surgery clinics, 15 years and older, and at least the third grade of middle school, and the exclusion criterion was cosmetic surgery due to appearance defects, according to the opinion of cosmetic surgeons in the study. Before filling out the research tools, the participants were provided with both oral and written explanations (attached to the questionnaire) to highlight the importance of research. Then, the participants were asked to complete the research instruments.
3.3. Measure
3.3.1. Body Image Shame Scale
BISS was designed by Duarte et al. The BISS contains 14 items that measure body image shame and consists of two sub-scales: a) external body shame that measures the perceptions, according to which the individuals are negatively evaluated and judged by others with regard to their physical appearance (e.g., I avoid social situations (e.g., going out, parties) because of my physical appearance.); b) internal body shame measures negative self-evaluations of physical appearance (e.g., my physical appearance makes me feel humiliated in communicating with others). Each item was scored based on a five-point Likert scale (from 0 = never to 4 = almost always). The mean score of this scale ranged from 0 to 4. The BISS was validated in nonclinical samples of women in the general population. The construct validity of the scale was acceptable. Cronbach’s alpha was reported as 0.96 (4).
3.3.2. Body Compassion Scale
The Body Compassion Scale (BCS) designed by Altman et al. is a 23-item measure. It has three subscales of defusion, common humanity, and acceptance. The items were scored based on a five-point scale from 1 (almost never) to 5 (almost always). The statements included “I try to accept my body defect as something that many people also experience” and “I have accepted my appearance as it is”. The scores for internal consistency of the three subscales of defusion, common humanity and acceptance were 0.92, 0.91, and 0.87, respectively. Cronbach’s alpha of 0.92 is acceptable for 23 items and supports the use of a total score (31). In the study, Cronbach’s alpha was 0.88.
3.3.3. Dysmorphic Concern Questionnaire
The Dysmorphic Concern Questionnaire (DCQ) designed by Oosthuizen is a 7-item self-report tool that measures concern about physical appearance. The items were scored based on a four-point Likert scale (0 - 3) in which point 3 shows the most common concerns. The items measured in this questionnaire are concerns about physical appearance, belief in being malformed; belief in bodily malfunction (such as foul, consulting with cosmetic surgeons, devoting so much time to concerns about physical appearance and concealing imperfections). The DCQ is a dimensional scale of appearance concerns. It was used in many clinical settings (32, 33). In Iran, research results supported the single-factor structure of concern about BDD in a national sample (RMSE = 0.07, NFI = 0.94, and CFI = 0.97) (34). In the study, Cronbach’s alpha was 0.77.
3.3.4. Appearance Anxiety Inventory
The Appearance Anxiety Inventory (AAI) developed by Veale et al. is a 10-item self-report inventory. It focuses on cognitive processes and safety-seeking behaviors of people with BDD. Each item was scored based on a scale from 0 (no) to 4 (always). The total score of AAI ranged from 0 to 40. Scores ≥ 19 showed the likelihood of BDD (35). In Iran, Cronbach’s alpha and test-retest reliability were 0.86 and 0.92, respectively (36). In the study, Cronbach’s alpha was 0.82.
3.3.5. Forms of Self-Criticizing/Attacking and Self-Reassuring Scale
The Forms of Self-Criticizing/Attacking and Self-Reassuring Scale (FSCRS) was developed by Gilbert et al. It is a 22-item self-report instrument that evaluates thoughts and reactions to failure and inadequacies. The FSCRS has two forms of self-criticism (self-hatred and self-inadequacy) and self-reassurance. The items were scored based on a five-point Likert scale (from 0 = not at all like me to 4 = extremely like me). Cronbach’s alpha was 0.90 for self-inadequacy, 0.86 for self-hatred, and 0.86 for self-reassurance (37). Internal consistency was reported acceptable in the Portuguese version of the scale (0.62 < Cronbach’s alpha < 0.89) (38). In the study, Cronbach’s alpha was 0.87.
3.4. Analysis Strategy
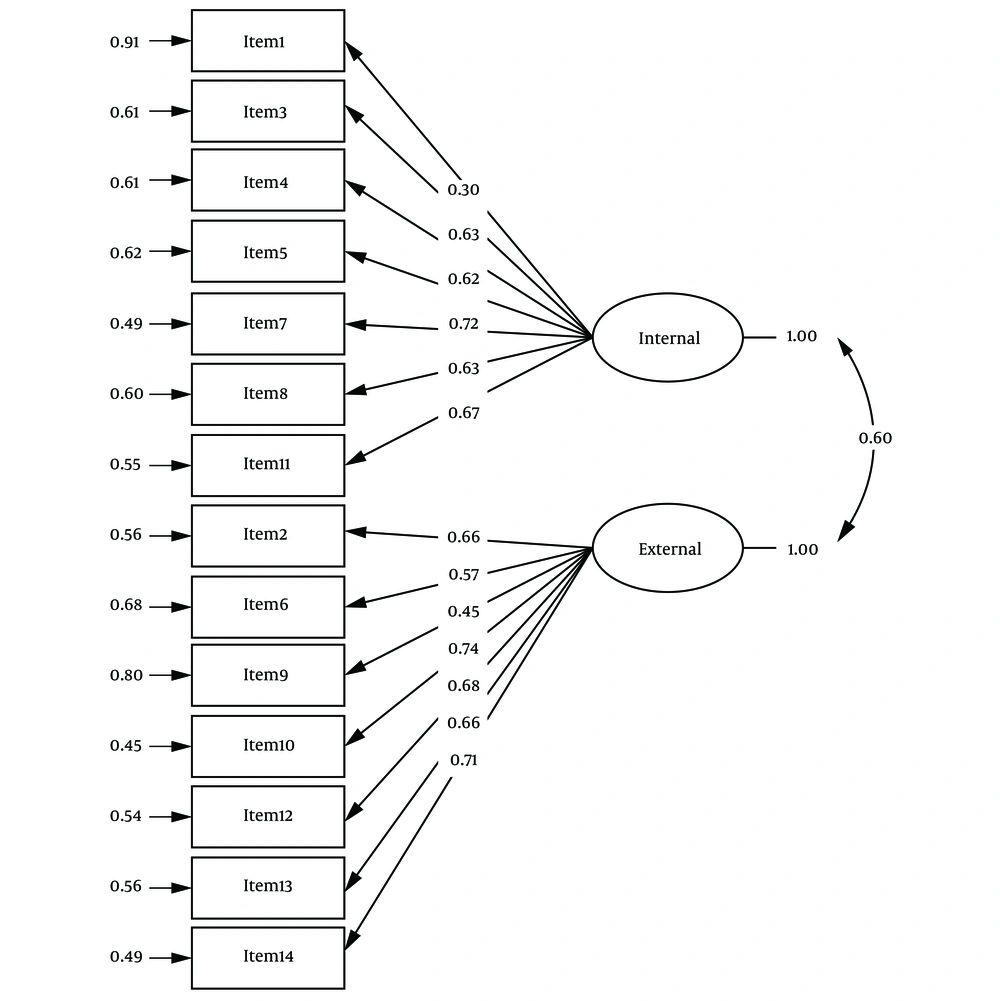
The data were cleaned and screened. Missing data were < 5% of the data-set. Thus, list-wise deletion with no imputation of data was used in the present analyses. The construct validity of the BISS was examined, using confirmatory factor analysis (CFA) and divergent and convergent validity. The CFA was selected to examine the fitness of the two-factor model of BISS (Figure 1). The divergent and convergent validity was investigated by examining the Pearson correlations between the BISS scores and body compassion, appearance anxiety, dysmorphic concern, self-criticism. Internal consistency and test-retest reliability (4 weeks’ interval, n = 50) were used to evaluate the reliability of the body image shame scale. Cronbach’s alpha was used to calculate the internal consistency of body image shame and its subscales. Interclass correlation coefficients were calculated for the test-retest reliability of the body image shame and its subscales. The data were analyzed using SPSS version 20 and LISREL version 8.80.
3.5. Ethical Considerations
This study was approved by the Iran University of Medical Sciences, and the ethical code of this study was IR.IUMS.REC.1398.555. The participants were informed that their participation was voluntary and they could leave the study at any time. They were also informed about confidentiality, and written informed consent was obtained from all participants.
4. Results
The mean ± SD BISS for all samples was 16.86 ± 9.29. The results of multivariate analysis of variance showed that there was no significant difference between males and females in the subscales of body image shame: Hotelling’s Trace F (2, 406) = 0.62, P = 0.54, partial Eta squared = 0.01. Also, the results of the independent t-test showed that there was no significant difference between males and females in terms of BISS total score: t (407) = -1.11, P = 0.27.
4.1. Reliability
The reliability of the body image shame was assessed using the following two ways:
Internal consistency: Cronbach’s alpha coefficient for internal body image shame, external body image and total score of body image shame were 0.79, 0.82, and 0.85, respectively.
Test-retest reliability: Interclass correlation coefficients of external body image shame, internal body image shame, and total score of body image shame were 0.90, 0.89, and 0.91, respectively.
4.2. Validity
The validity of the scale was assessed using the following two ways:
4.2.1. Confirmatory Factor Analysis
The fit of the two-factor model of the scale was evaluated using the Comparative Fit Index (CFI), Normed Fit Index (NFI), Non-Normed Fit Index (NNFI), Goodness of Fit Index (GFI), Adjusted Goodness of Fit Index (AGFI), Incremental Fit Index (IFI), Root Mean Square Error of Approximation (REMSEA), Root Mean Square Residual (RMR), and χ2/df indices. The results of the model fit indices are presented in Table 1. As you can see in Table 1, indices confirm the suitability of the model.
| Fit Indices | Body Image Shame |
|---|---|
| χ2 | 234.35 |
| P | 0.001 |
| χ2/df | 3.08 |
| RMR | 0.06 |
| GFI | 0.92 |
| AGFI | 0.90 |
| NFI | 0.94 |
| CFI | 0.96 |
| IFI | 0.96 |
| NNFI | 0.95 |
| RMSEA | 0.07 |
4.2.2. Convergent and Divergent Validity
The correlation between BISS and appearance anxiety, dysmorphic body, and self-criticism was positive and significant (P < 0.05), indicating good convergent validity, but has a negative and significant correlation with body compassion (P < 0.05), indicating good divergent validity (Table 2).
| Variable | Mean (Standard Deviation) | 1 | 2 | 3 | 4 | 5 | 6 | 7 |
|---|---|---|---|---|---|---|---|---|
| 1. Body image shame | 16.86 (9.29) | - | ||||||
| 2. Internal body image shame | 9.92 (5.37) | 0.86a | - | |||||
| 3. External body image shame | 6.94 (5.37) | 0.86a | 0.49a | - | ||||
| 4. Body compassion | 76.23 (14.66) | -0.57a | -0.40a | -0.60a | - | |||
| 5. Appearance anxiety | 13.62 (6.83) | 0.69a | 0.52a | 0.68a | -0.57a | - | ||
| 6. Dysmorphic concern | 13.09 (3.45) | 0.46a | 0.33a | 0.46a | -0.49a | 0.46a | - | |
| 7. Self-criticism | 33.78 (13.41) | 0.63a | 0.49a | 0.60a | -0.54a | 0.58a | 0.39a | - |
aP < 0.01.
5. Discussion
The current study investigated the psychometric properties of BISS in cosmetic surgery clinics. The results of confirmatory factor analysis showed that the two-factor model (internal and external body image shame) fitted the data (GFI = .92, NFI = .94, RMSEA = .07). The results of this study were consistent with the results of the study by Duarte et al. (4) that showed a body image shame scale consisted of two subscales of internal and external shame. The results of this study were also consistent with the results of the studies that considered two components of shame, namely internal shame (self-directed) and external shame (focused on judgments and evaluations of others) (7, 12, 13). Seven items of internal body image shame focus on negative self-evaluation and tendency to hide body parts (e.g., covering some body parts or avoiding wearing some cloths). Seven items of external body image shame focus on body image in the view of the outside world. It measures how one may be negatively evaluated and judged by others for physical appearance. In total, body image shame is a negative self-evaluation and social assessment of physical appearance (e.g., weight, size, and shape). The individual is perceived by others as an unattractive, inferior, and defective person (13). According to the bio-psycho-social model of shame, humans have an inherent tendency to show an ideal image of themselves and promote positive feelings about themselves in others’ minds (13, 39, 40). According to Gilbert, shame is a kind of warning signal, which works as a defensive function. By considering this issue, it may that others evaluate the person in a negative way and this can lead to rejection and deprivation from social rights. Therefore, shame may trigger a set of dysfunctional defensive behaviors (masking, avoidance, or excessive self-monitoring) to reduce perceived negative outcomes. It also triggers self-protection (40). The BISS assesses these inefficient defensive behaviors, including covering body parts, avoiding social situations, or feeling so uncomfortable for attending in social situations and excessive focus on body.
The reliability of the scale was assessed using test-retest and internal consistency. The test-retest coefficient of the BISS and the two subscales was above 0.70, which indicated suitable consistency of the scale in a four-week period. This finding was in line with the findings of the study by Duarte et al. Internal consistency was assessed by calculating Cronbach’s alpha for the scale and the two subscales (α > 0.70), which indicated suitable internal consistency of the instrument.
The results of divergent and convergent validity showed that the BISS had positive and significant relationships with appearance anxiety, dysmorphic concern, and self-criticism, while it had a negative and significant relationship with body compassion. These findings are consistent with the results of previous studies that found a relationship between shame and concerns about body image and determined shame as a risk factor for body image problems (9, 11). Shame was also associated with body image problems and greater vulnerability to eating disorders (10). Other studies also showed that self-criticism had a significant and positive relationship with body image shame (17, 25, 41, 42). Shame is considered to be the underlying trigger of self-blaming so that people may use self-criticism as a defensive strategy in order to avoid feelings related to it (43). Therefore, self-criticism is an inefficient defensive strategy originating from shame (44, 45) that aims to modify and improve personal characteristics or behaviors in order to promote self-protection (44). Studies have also shown that shame had a negative relationship with compassion (9, 46). Compassion-based skills can protect against body dissatisfaction and body shame (10, 47-50). The people who have a mindful attitude about their physical inadequacies rather than over-identification them, perceive body image-related negative experiences as shared human experiences and kindly deal with their painful feelings and thoughts. They experience less body shame and are more satisfied with their body image.
Limitations of the study should be resolved in future studies. These limitations were: a) other shame scales were not used to assess convergent validity; therefore, it is suggested that future research use other tools to measure shame as a convergent validity.; b) most of the participants were single and women that can limit generalization of the findings to men and married people, Given this limitation, it is recommended that future research should be conducted on a more balanced sample in terms of gender and marital status; c) the research sample was selected from individuals visiting cosmetic surgery clinics. It is necessary to conduct this study on nonclinical and general populations.
5.1. Conclusion
The results of this study showed that the Persian version of the BISS had a relatively suitable factor structure, validity, and reliability in the sample population referred to cosmetic surgery clinics. Therefore, it can be used as a valid instrument in research and clinical works in populations with concerns about body image.