1. Introduction
Spontaneous intramural small bowel hematoma is reported with increasing frequency in adults (1). However, intraluminal small bowel hematoma has been rarely reported in children (2), and it can be a rare cause of small bowel obstruction. The imaging features of small bowel hematomas may vary depending on the age and location of the hematoma, and these features may mimic those of cystic or solid masses. We present the ultrasonography (US) and computed tomography (CT) features of a large intraluminal ileal hematoma that caused small bowel obstruction in a child.
2. Case Presentation
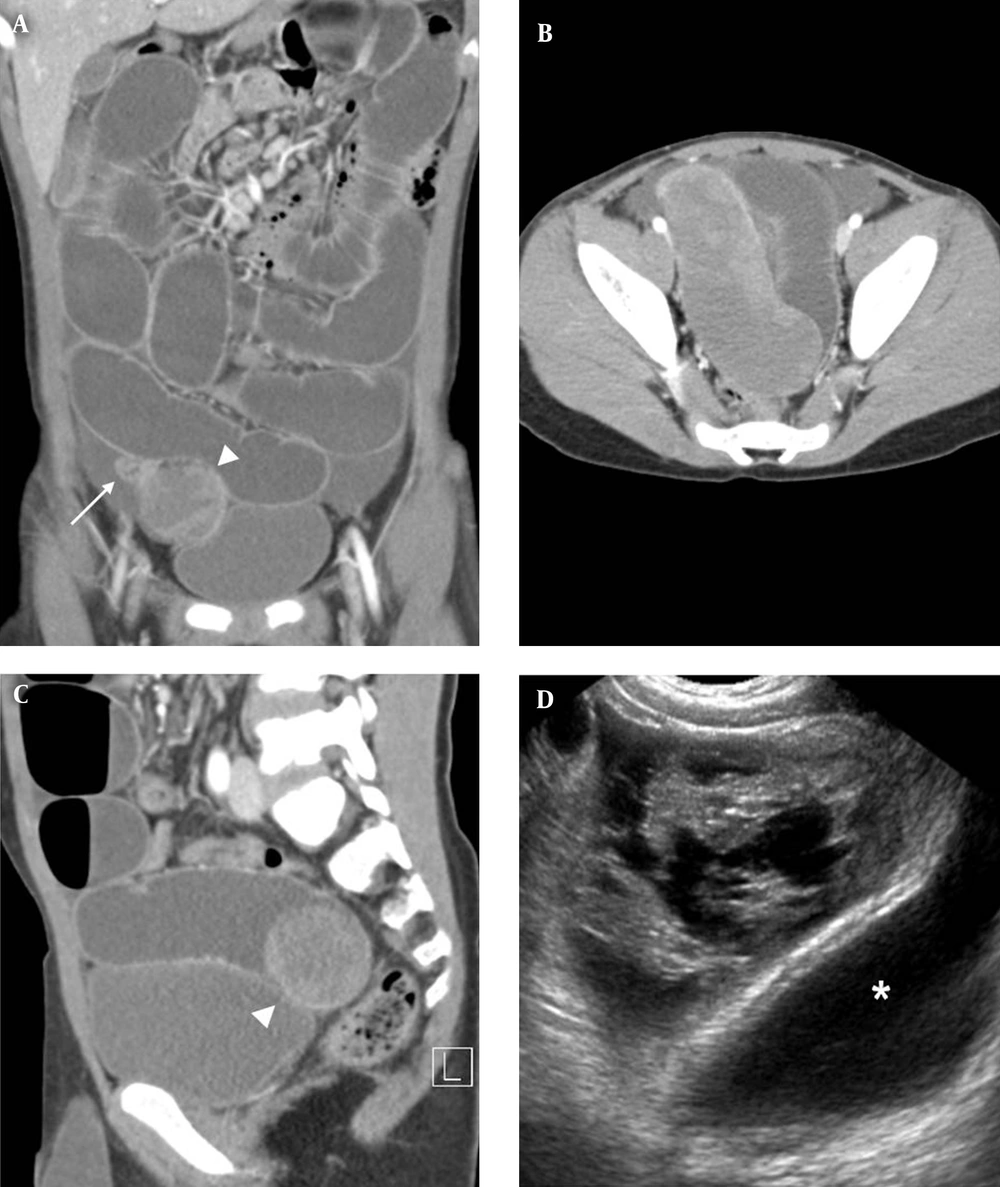
An eight-year-old boy presented to the emergency department with a five-day history of abdominal pain and a three-day history of bilious vomiting. His medical record was unremarkable otherwise and he had no history of abdominal surgery, except for right hydrocelectomy. The results of laboratory values, including coagulation laboratory tests, were unremarkable. His abdomen was slightly rigid and distended. Erect and supine abdominal radiographs showed multiple dilated small bowel loops with multiple air-fluid levels, suggesting mechanical ileus. Computed tomography (CT) showed fluid- and gas-filled distension of the small bowel loops and a transition point was observed at the distal ileum in the right pelvic cavity (Figure 1A). An intraluminal tubular mass-like lesion was observed at the transition point, measuring approximately 10.5 × 3.8 × 3.6 cm (Figure 1 B, C). The lesion was heterogeneously hyperdense without enhancement or visible septa, suggesting a complicated cystic lesion. The distal ileum was collapsed in the region distal to the transition point. There was no evidence of intussusception or volvulus. Small bowel obstruction due to a complicated cystic mass was provisionally diagnosed. The US examination revealed a multiloculated cystic mass with fine septation in the distal ileum at the transition point (Figure 1D). The mass comprised an echogenic portion, which was probably a hemorrhagic portion.
Laparoscopic exploration was performed for suspected small bowel obstruction caused by a complicated cystic mass. A large dark-bluish and reddish tubular cystic mass was detected at the transition point in the distal ileum (Figure 2). Segmental resection of the small bowel and end-to-end anastomosis were performed. Histopathologic examination indicated a submucosal cystic mass filled with blood; these findings suggested submucosal organizing hematoma in the distal ileum. Focal dilated lymphatic spaces were observed in the mucosa and submucosa, suggestive of focal lymphangiectasia secondary to organizing submucosal hematoma. The patient did not have bleeding disorder and the patient and his parents could not recall any episode of abdominal trauma. However, blunt trauma can be a tentative cause of ileal hematoma because he was scatter brained and reckless. Recovery was uneventful.
A eight-year-old boy with acute abdominal pain and bilious vomiting. A, Diffuse distension of the small bowel and a transition point with the mass (arrowhead) in the right pelvic cavity in coronal computed tomographic image. The distal ileum (arrow) was completely collapsed in the region distal to the transition point. B, A 10.5-cm long intraluminal tubular mass with heterogeneous hyperdensity in the distal ileum in computed tomographic image at the level of the pelvic cavity. C, the intraluminal nature of the mass (arrow head) in sagittal computed tomographic image. D, A multiloculated cystic mass in the right pelvic cavity, superior to the urinary bladder (asterisk) in an ultrasonographic image. The echogenic portion within the mass was suspected to be the hemorrhagic portion.
3. Discussion
Small bowel hematoma in children is generally caused by trauma, anticoagulation therapy, bleeding disorders, vasculitis, and tumors (1-5). Because of the rich submucosal vascular supply, hemorrhage usually originates in the submucosal layer of the bowel (1). As the bleeding continues slowly, intramural, intraluminal, mesenteric, and retroperitoneal hemorrhage may occur (1). It may also be associated with hemorrhagic ascites (1).
The imaging features of small bowel hematoma vary depending on its location and age. For acute intramural small bowel hematoma, US may show circumferential thickening of the bowel wall with hyperechogenicity (1). An acute intraluminal hematoma may appear as an avascular mass with diffuse or inhomogeneous echogenicity (6). As liquefaction occurs, the hematoma shows mixed echogenicity with internal septation, thickened hyperechoic walls, or mural nodules (6), and eventually becomes anechoic. The US or magnetic resonance imaging can reveal the multilocular nature of the mass with fine septation. On CT images, an acute small bowel hematoma appears as a thickened bowel wall or mass with hyperdensity (7). The hyperdense area can be observed during the first ten days and subsequently evolves into a hypodense area (7).
The differential diagnosis of a bowel-related cystic mass in children should include duplication cyst, Meckel’s diverticulum, lymphangioma, and small bowel hematoma, which may present with intussusception or volvulus. Lymphangiomas are usually multilocular and infrequently located in the bowel (8). Occasionally, a duplication cyst might be multilocular.
Traumatic small-bowel hematomas most commonly involve the duodenum, whereas nontraumatic ones most commonly affect the jejunum, followed by the ileum and duodenum (1, 3, 5). Abbas et al. reported that nontraumatic spontaneous small-bowel hematomas appear longer than traumatic hematomas (4). Gaines et al. reported that traumatic injury of duodenum is unusual in children and child abuse should be suspected in a young child with duodenal injury (5). Although traumatic ileal hematoma is uncommon, a tentative cause in our case was blunt trauma. Several imaging features are helpful in distinguishing spontaneous small-bowel hematomas from other types. However, the differential diagnosis is challenging and blunt trauma in children can be unwitnessed.
In conclusion, although intraluminal small bowel hematoma is rare in children, it can present as an intraluminal cystic mass and should be considered as a rare cause of small bowel obstruction. The US and CT findings of submucosal ileal hematoma could be useful for the diagnosis of such cases in the future.