1. Background
Premaxilla is one of the most common regions exposed to trauma and loss of teeth (1, 2). In this region, the most important anatomical landmark is the nasopalatine canal (NPC) (1). Stenson offered a definition of NPC for the first time in 1683 AD (3). This canal is located in the midline of the maxilla, behind the central incisor teeth (4-6). The orifice of the canal in the mouth is called the incisive foramen (IF) and it is located beneath the incisive papilla (4, 6-8). The openings of this canal in the nose are called Stenson’s foramina (SF) (3, 9).
NPC, also known as the incisive canal or anterior palatine canal (9, 10), plays an important role in the surgery of the premaxillary region. The canal includes the neurovascular bundle (1, 2). Since it is important to know the anatomical appearances and variations of important landmarks prior to surgical procedures, such as implant placement (6, 10), recognition of NPC morphology is necessary (3), especially because of the higher esthetic expectations in the anterior region of the maxilla and the increasing use of implants in dentistry (1, 5). Therefore, observing the features of NPC imaging is useful in achieving the optimal surgical treatment plan while avoiding implant contact with the canal neural tissue, which may lead to lack of osseointegration or result in sensory dysfunction (6, 9, 11).
In addition, there is a possibility of cyst formation in the mentioned canal, which is sometimes difficult to be distinguished from a normal canal in two dimensional (2D) routine images (10). Despite many published studies related to the pathology of NPC (12-14), studies that show anatomical variations in size and morphology, and also its relation with adjacent structures, are limited in different nations (5).
Although radiography is an important diagnostic tool, conventional imaging is not useful enough to evaluate these anatomical landmarks due to the limitations in revealing the third dimension (5). Nowadays, use of cone beam computed tomography (CBCT) technology provides new diagnostic facilities.
2. Objectives
In this study, with access to the required diagnostic imaging tool and sufficient samples, we were encouraged to evaluate the morphological and anatomical variations of NPC. In addition, the dimension of the canal and its relationship with age, sex, and the presence of central incisor teeth in a sample of Iranian population were also evaluated.
3. Materials and Methods
The study was performed on CBCT images of 326 Iranian patients aged between 18 and 80 (mean ± SD age 48.5 ± 15.4) years, referred to four maxillofacial radiology centers in Tehran. The images were already provided for a variety of diagnostic and therapeutic purposes. Samples were selected randomly from each center. Inclusion criteria were patients 18 years and older and image voxel size = 0.200 mm. Exclusion criteria were severe maxillary ridge atrophy, pathologic lesions or impacted teeth in the anterior maxilla, implant or graft in the premaxilla, palatal cleft or syndromic diseases, and remaining roots.
CBCT images were obtained using two CBCT units: Scanora 3D (Sordex, Tuusula, Finland) with a voxel size of 0.200 mm and NewTom VGI (QR SRL Co, Verona, Italy) with a voxel size of 0.200 mm. Scanora 3D’s operating parameters were set at 8 mA and 90 kvp, with an exposure time of 3.5 s, while for Newtom VGI, parameters were set at 110 kvp and exposure time was 3.6 s. For all CBCT images, limited field of view (FOV) of 7.5 × 10 or 8 × 12 was selected.
CBCT images were analyzed using a MFCD-1219, 19-inch medical monitor (Barco, Belgium) with a resolution of 1280 × 1024 pixels.
DICOM file of all samples were imported into On Demand 3D application software (ver.7), and all analyses and measurements described were performed using the aforementioned software in all three sagittal, coronal and axial plans by an experienced oral and maxillofacial radiologist. All data was entered and analyzed by using SPSS ver.19 for windows (SPSS Inc, Chicago, Ill, USA). The Chi-square test was used to determine the relationship between NPC classification, age, gender, and dental status. Differences in measurements between genders were compared using independent t-test. Differences of parameters in patients of varied age and dental status groups were analyzed using analysis of variance (ANOVA). In order to check the intraobserver reliability, one month later, the same observer assessed the parameters and repeated the measurements in 30 CBCTs. The Pearson correlation coefficient > 0.7 was achieved.
For 3D imaging, the anteroposterior dimension of IF at mouth opening and SF at nasal opening were recorded by connecting two anterior and posterior walls in 3D images (Figure 1B).
A, The selected landmarks in the sagittal plane: Anteroposterior diameter of Stenson’s foramen at nasal opening, antero posterior diameter of the incisive foramen at the mouth opening, canal length was measured by drawing a line from midpoint of the incisive foramen towards the midpoint of Stenson’s foramen, angle of canal curvature was measured by recording the angle between the long axis of the canal (canal length) and the nasal floor to the ANS (from ANS to PNS). B, The size of the incisive foramen in 3D reconstruction is demonstrated. C, The effect of another measuring method exactly parallel to the horizon on the anteroposterior dimension of the incisive foramen and canal length (incisive foramen was measured parallel to the horizon).
In the sagittal plane the following assessments were done:
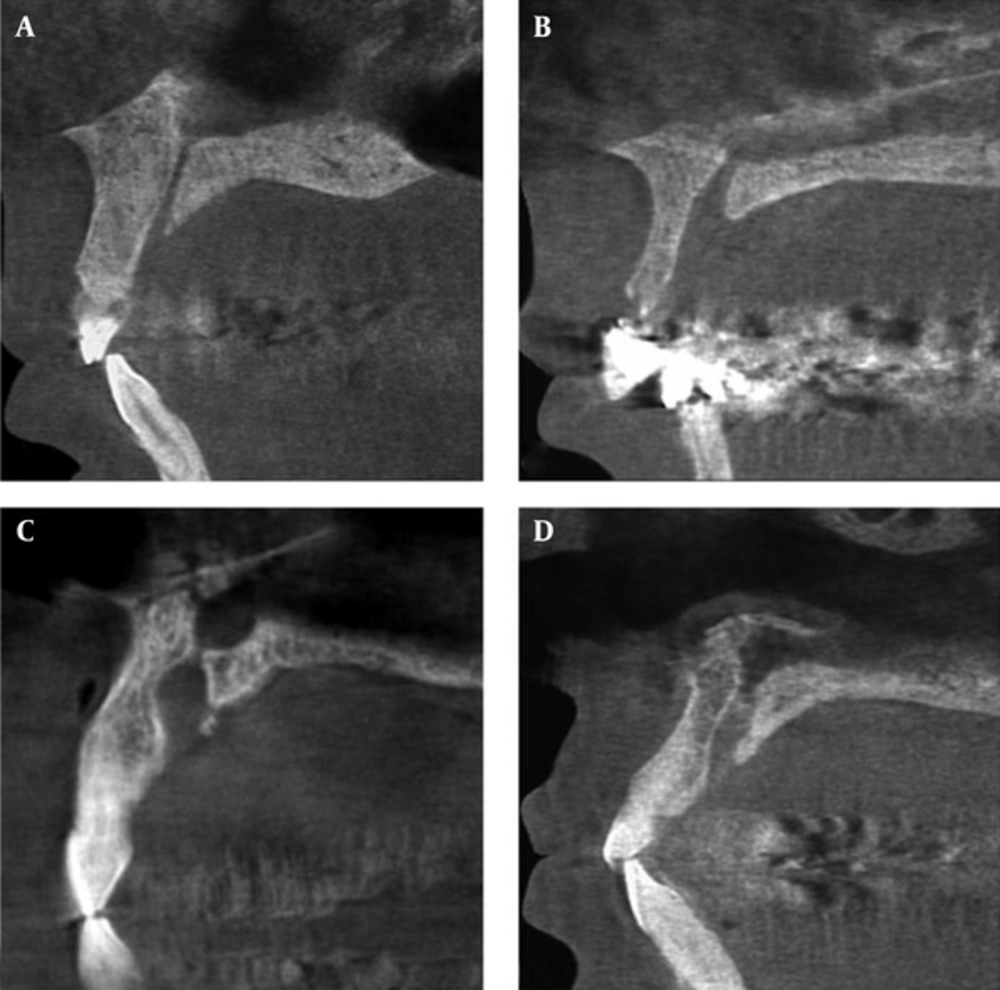
1. Shapes of NPC were classified into four groups: cylindrical (Figure 2A), funnel-shaped (Figure 2B), hourglass (Figure 2C), and spindle (Figure 2D) (10).
2. The end part of the canal at the palatal level, especially in the buccal wall of the canal, is often indistinct in the sagittal plane. So, the usage of 3D image as a complement is very helpful for precise measurement of the actual size of the canal entrance. In fact, we used 3D images for these measurements. Since the opening slope of the foramina affects the recorded canal length and opening dimension, the index lines in the sagittal plane were determined in accordance with the size of these orifices in 3D reconstruction (Figure 1A and B).
3. Canal length was measured using the drawn midpoint of the IF in front of the midpoint of the SF (Figure 1A) (1, 3, 5).
4. Angle of canal curvature was measured by recording the angle between the long axis of the canal (canal length) and the nasal floor to the ANS (from ANS to PNS) (Figure 1A) (10).
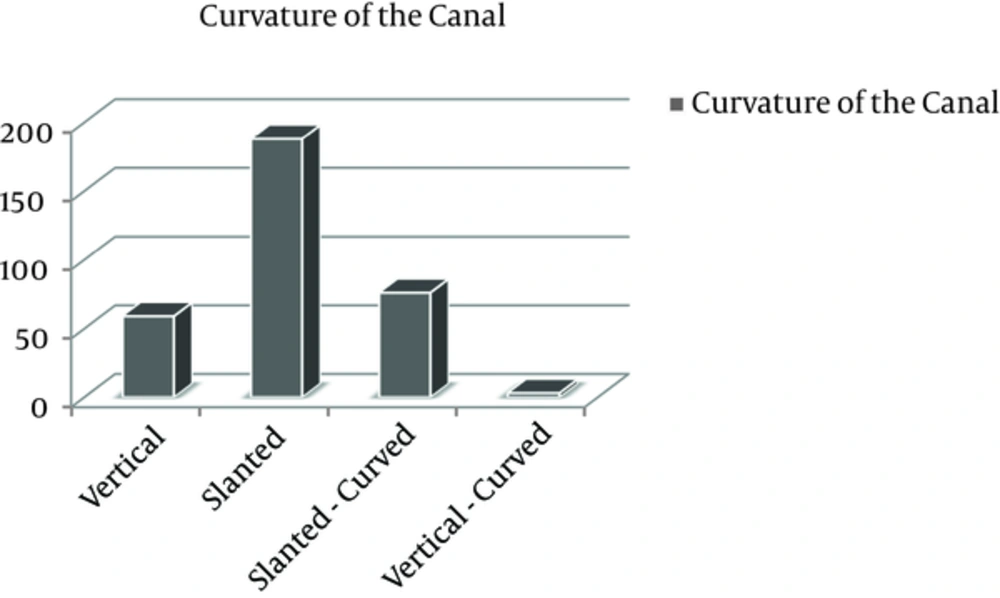
5. Curvature of the canal was classified as vertical curved, vertical, slanted, and slanted curved (10).
The nasal floor was considered as a horizontal index. If the canal axis had an angle of 10° or more with the perpendicular line (> 10), it was considered as slanted. An angle below 10° (< 10) was considered as vertical. Straight or curved canals were determined based on the curvature of the palatal canal wall (10).
In the axial plane the following assessments were done:
1. The dimension of mediolateral openings of IF and SF were obtained by measuring their diameter on the axial plane (10) and 3D reconstruction. In cases with more than one orifice, the diameters of the foramens were added together (1, 3).
2. The number of entries at the nasal and palatal level was also recorded.
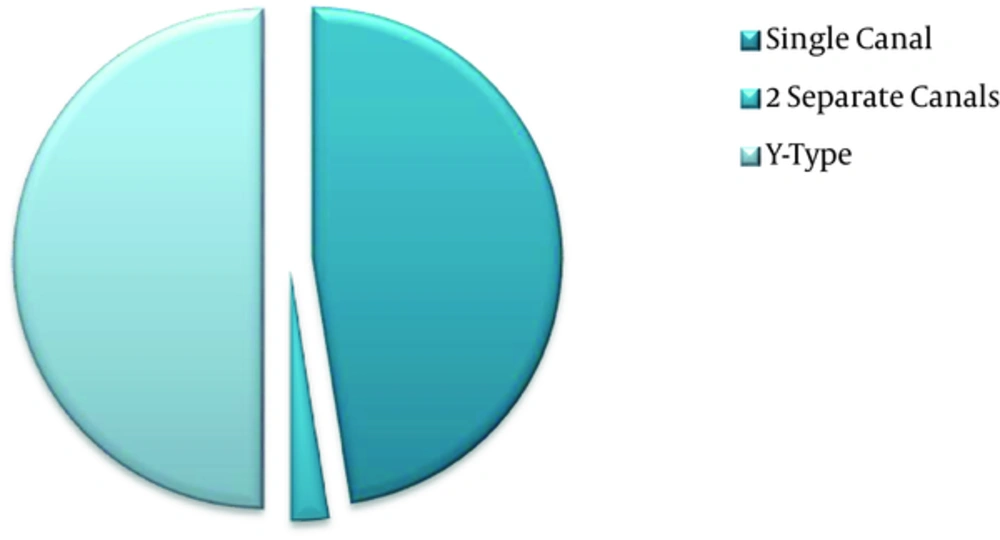
In the coronal plane, the furcation level of the canal was categorized into upper, middle and lower third after reorientation of the skull as the coronal axis was located along the NPC (10). Anatomic variations of canal forms in the coronal plane were divided into three groups: 1) single-canal, 2) two separate parallel canals and 3) a variety of Y-type forms of NPC (regardless of the split location) (3).
4. Results
In this study, anatomic variation of NPC was studied among 326 patients with an average age of 48.5 ± 15.4 (aged 18 to 80 years old). Totally, 41.7% were males and 58.3% percent were females. In terms of dental status, 7.3% were edentulous, 8.6% had one incisor, 75.5% had two incisors, and 8.6% had two missing incisor teeth. Anatomical variations of NPC are shown in the tables with respect to age, gender, and condition of the teeth (Tables 1 - 3). Parameter normality was accomplished by Shapiro-Wilk test and according to the test, all quantitative variables in this study had a normal distribution.
| Parameters | 18 - 39 years | Lower Limit | Upper Limit | 40 - 59 years | Lower Limit | Upper Limit | 60 - 80 years | Lower Limit | Upper Limit | Mean±SD | P Value |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Angulation of NPC/angle of curvature, ° | 106.8 ± 9.69 | 104.8 | 109 | 108.2 ± 9.02 | 106.68 | 109.7 | 109.7 ± 8.90 | 108 | 111.5 | 108.3 ± 9.22 | 0.09 |
| Length of the canal in the sagittal plane, mm | 13.28 ± 2.76 | 12.72 | 13.8 | 12.61 ± 2.47 | 12.19 | 13.02 | 12.78 ± 2.69 | 12.2 | 13.31 | 12.85 ± 2.63 | 0.16 |
| Anteroposterior dimension of the Incisive foramen, mm | 7.23 ± 2.04 | 6.81 | 7.64 | 7.58 ± 1.78 | 7.28 | 7.87 | 7.66 ± 2.08 | 7.24 | 8.07 | 7.51 ± 1.95 | 0.43 |
| Anteroposterior diameter at the foramina of Stenson, mm | 3.33 ± 1.03 | 3.12 | 3.53 | 3.30 ± 1.15 | 3.1 | 3.49 | 3.33 ± 1.29 | 3.07 | 3.58 | 3.32 ± 1.16 | 0.3 |
| Mediolateral dimension of thedio-laterae incisive foramen, mm | 3.80 ± 0.95 | 3.6 | 3.99 | 4.24 ± 0.86 | 4.09 | 4.38 | 4.28 ± 1.07 | 4.06 | 4.49 | 4.12 ± 0.97 | P < 0.05a |
| Mediolateral diameter at the foramina of Stenson, mm | 4.36 ± 1.37 | 4.08 | 4.63 | 4.65 ± 1.64 | 4.37 | 4.92 | 4.49 ± 1.31 | 4.22 | 4.75 | 4.52 ± 1.47 | 0.3 |
Abbreviations: NPC, nasopalatine canal; SD, standard deviation.
aP value < 0.05 which is significant.
| Parameters | Male | Lower Limit | Upper Limit | Female | Lower Limit | Upper Limit | Mean±SD | P Value |
|---|---|---|---|---|---|---|---|---|
| Angulation of NPC/angle of curvature, ° | 109 ± 9.37 | 107.42 | 110.57 | 107 ± 9.06 | 105.71 | 108.28 | 108.3 ± 9.22 | 0.078 |
| Length of the canal in the sagittal plane, mm | 13.70 ± 2.52 | 13.27 | 14.12 | 12.25 ± 2.54 | 11.88 | 12.61 | 12.85 ± 2.63 | 0.002a |
| Anteroposterior dimension of the incisive foramen, mm | 7.52 ± 2.08 | 7.17 | 7.86 | 7.49 ± 1.85 | 7.22 | 7.75 | 7.51 ± 1.95 | 0.9 |
| Anteroposterior diameter at the foramina of Stenson, mm | 3.55 ± 1.29 | 3.33 | 3.76 | 3.15 ± 1.02 | 3 | 3.29 | 3.32 ± 1.16 | 0.002a |
| Mediolateral dimension of the incisive foramen, mm | 4.41 ± 1.00 | 4.24 | 4.57 | 3.92 ± 0.9 | 3.79 | 4.04 | 4.12 ± 0.97 | 0.001a |
| Mediolateral diameter at the foramina of Stenson, mm | 4.75 ± 1.59 | 4.48 | 5.01 | 4.36 ± 1.37 | 4.16 | 4.55 | 4.52 ± 1.47 | 0.016a |
Abbreviations: NPC, nasopalatine canal; SD, standard deviation.
aP value < 0.05 which is significant.
| Parameters | Edentulous | 1 Incisor | 2 Incisors | Loss of 2 Incisors | Mean±SD | P Value |
|---|---|---|---|---|---|---|
| Angulation of NPC/angle of curvature, ° | 109.7 ± 9.73 | 108.5 ± 7.20 | 107.4 ± 9.04 | 114.2 ± 10.17 | 108.3 ± 9.22 | 0.002a |
| Length of the canal in the sagittal plane, mm | 12.85 ± 1.97 | 13.60 ± 2.73 | 12.82 ± 2.63 | 12.41 ± 2.98 | 12.85 ± 2.63 | 0.2 |
| Anteroposterior dimension of the Incisive foramen, mm | 7.71 ± 1.95 | 6.73 ± 1.95 | 7.64 ± 1.94 | 6.87 ± 1.81 | 7.51 ± 1.95 | 0.003a |
| Anteroposterior diameter at the foramina of Stenson, mm | 3.65 ± 1.84 | 2.82 ± 1.06 | 3.31 ± 1.09 | 3.60 ± 1.04 | 3.32 ± 1.16 | < 0.05a |
| Mediolateral dimension of the Incisive foramen, mm | 4.37 ± 1.29 | 4.01 ± 0.96 | 4.08 ± 0.91 | 4.46 ± 1.11 | 4.12 ± 0.97 | 0.12 |
| Mediolateral diameter at the foramina of Stenson,mm | 4.79 ± 1.26 | 3.83 ± 1.61 | 4.52 ± 1.47 | 4.99 ± 1.32 | 4.52 ± 1.47 | < 0.05a |
Abbreviations: NPC, nasopalatine canal; SD, standard deviation.
aP value < 0.05 which is significant.
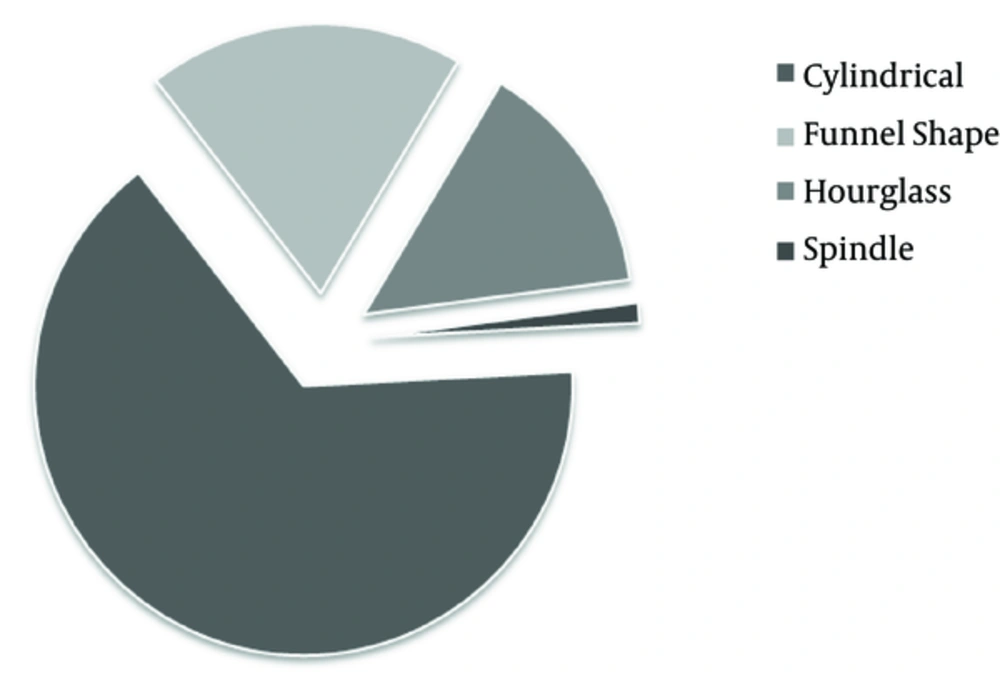
Regarding canal shape, morphological analysis of the canal in the sagittal plane showed that the cylindrical type recorded in 213 cases (65.33%) was the most common shape of canal. Funnel-shaped, with a 19.01% frequency was recorded as the second most common, while hourglass was seen in 14.41% and spindle in 1.22% of the cases (Figure 3). It should be noted that spindle was only found in four cases, among three men and one woman with two incisor teeth situation. Due to lack of sufficient samples for analyses, they were excluded.
In terms of canal anatomic variation in the coronal plane, 163 cases (50%) were Y-type and 155 cases (47.5%) had a single canal while only six cases (2.5%) showed two separate canals (Figure 4). Chi-square exact test showed no correlation between NPC anatomic variation and age, gender and dental status in the coronal plane.
By statistical analysis, the effect of gender on the canal length, anteroposterior dimension of SF, and mediolateral dimension of SF and IF and the number of orifices at the nasal floor were significant. The canal length was recorded with a minimum of 6.74%, a maximum of 20.61%, and an average of 12.85 ± 2.63 mm (Table 2). The average canal length for men was (13.70 ± 2.52 mm) more than that of women (12.25 ± 2.54 mm) (Table 2).
The average anteroposterior dimension of NPC at the nasal level was 3.32 ± 1.16 mm (SF) (Table 2). The anteroposterior diameter of SF opening in men (3.55 ± 1.29 mm) was wider than in women (3.15 ± 1.02 mm) (Table 2). The mean value of mediolateral size of NPC was 4.12 ± 0.97 mm (IF) at the palatal level and 4.52 ± 1.47 mm (SF) at the nasal level (Table 2). The recorded value in these two openings was also wider in men (4.41 ± 1.00 mm and 4.75 ± 1.59 mm in men vs. 3.92 ± 0.90 mm and 4.36 ± 1.37 mm in women, respectively) (Table 2).
One orifice at the nasal level in 171 (52.8%) cases had the highest prevalence, while two openings in 143 cases (44.1%) and three openings in ten cases (3.1%) were also recorded. Four openings of NPC at the nasal level were seen only in two cases in women under 40 years who had two incisor teeth. Due to lack of samples, these two cases were excluded from the study in order to avoid problems in the analysis. At the palatal level, most cases had one orifice (323 cases or 99.1%), and two openings were found in just three cases (0.9%).
In this study, patients were divided into three groups according to age range; ≤ 39, 40 to 59 and ≥ 60 years (10). Analysis demonstrated a significant relationship between age and the curvature in the sagittal plane, mediolateral average size in IF in the axial plane, and the number of openings at the nasal level in the axial plane (Table 1). Slanted canal reported in 188 cases (58.2%), was the most prevalent form. The slanted-curved was seen in 76 cases (23.5%), and vertical in 59 cases (18.3%). The vertical-curved was evident in only three cases, in two men and one woman under 40 years, who had two incisor teeth and were not included in the study due to lack of adequate samples (Figure 5). Analysis of variance (ANOVA) showed that the average of mediolateral dimension of NPC varied in the IF in the axial plane of various groups (P = 0.001). Posthoc test (LSD) showed that this difference was between the age groups over 60 years and the others (P < 0.05).
Based on dental status, patients were classified into four groups: edentulous, with one incisor, with two incisors, and missing incisors (1). In analyzing the parameters based on dental status, it was discovered that the presence of incisors had a significant impact on the canal angle in the sagittal plane (Table 3), the anteroposterior dimension of SF and IF, and also the location of canal division into two or more branches in the coronal plane. In the samples survey, the average angle of the canal was 108.3° ± 9.22 (Table 3). ANOVA showed that the average angle of curvature in the sagittal plane of NPC was distinct in people with different dental statuses (P = 0.002). Posthoc test (LSD) demonstrated a difference between the group without incisors and other groups (all three other groups) (P < 0.05). The average angle of the canal in the group without incisors was 114.2° ± 10.17 (Table 3).
The average of SF and IF anteroposterior dimension were 3.32 ± 1.16 and 7.51 ± 1.95, respectively, while in the fully edentulous group, the mean of the anteroposterior dimension was 3.60 ± 1.04 and 6.87 ± 1.81, respectively (Table 3). In the coronal plane, the division point of the canal was statistically higher in the middle third in 88 cases (51.5%), with little difference in the upper third in 80 cases (46.8%) and in the lower third in only three cases (1.7%).
5. Discussion
In the present study, in line with previous studies, it was shown that NPC had different anatomic and morphologic variations. Despite numerous studies published on the evaluation of canal pathology (12-14), available literature about its size, morphology and anatomical variations is inadequate (1). Considering the fact that premaxilla is very important in terms of esthetics (1, 5) and it is important regarding implant site preparation, knowledge about its anatomy seems to be essential (5).
In recent years, CBCT imaging system became popular in the evaluation of anatomic structures, such as the IF, NPC, mandibular canal, and mental foramen. CBCT is less costly with lower radiation dose compared to CT, while providing valuable images. CT (15-17), spiral CT (2, 18), micro CT (19) techniques, and endoscopic examination (20) have been used in previous studies (1).
In this study, NPC with CBCT was investigated among a group of Iranian population.
Various classifications were seen for NPC in previous studies. Etoz et al. classified the canal shape into six groups: tree branch, cylindrical, banana-like, funnel-like, cone-like, and hourglass (1). Guncu et al. and Mardinegar et al. considered four categories (hourglass, funnel, banana, and cylindrical) (16, 17), while Liang noted only two categories: conical and cylindrical (2). As the distinction between funnel-like and cone-like shapes, due to similarity of these two, was highly affected by the observer’s opinion, and the banana-like canals could be defined as a curved cylindrical canal, in this study, NPC was classified into four groups with obvious different shapes: cylindrical, funnel-shaped, hourglass, and spindle.
The current study results showed that cylindrical canals had the highest percentage; the results were in consistency with most studies (2, 6, 7, 10, 17). Cylindrical canal was observed in 213 cases (65.33%), funnel in 61 cases (19.01%), hourglass in 47 cases (14.41%), and spindle in four cases (1.22%). These findings were different from the results reported by Etoz et al. and Sekerci et al. in which hourglass (38.8%) and funnel (26.9%) were the most common shapes (1, 3). Since both of these studies were conducted on a Turkish population, these differences can be justified by normal racial variations. The canal shape has no significant relationship with age, gender and dental status, which was in accordance with the findings of previous studies (3, 6, 10).
Unlike Song et al. who introduced the vertical type as the dominant feature (19), in this study slanted was the most common form in 188 cases (58.2 %), while the vertical curved was seen only in two men and one woman of less than 40 years of age who had two incisor teeth and showed a low incidence, and this was confirmed by the findings of Fernandez et al., Thakur et al., and Al-Amery et al. (7, 10, 11). Through the statistical analysis, the curvature of NPC in the sagittal plane had a significant relationship with age.
Liang et al. reported the mean curvature of the NPC as 77.4 ± 8.9 (2), while in the study conducted by Thakur et al. an angle of 63 ± 8.03 degrees from the horizon was reported (10). Fernandez studied the supplement angle of the one calculated in this study, and reported the mean angle of 73.33 ± 8.11 (7). In the present study, the mean was 108.3 ± 9.22 (80.30 - 142.30), which was closer to the average angle derived from the study of Fernandez et al. (7) than the other studies (2, 10). ANOVA showed that the curvature angle of canals in the sagittal plane among people with different dental statuses was different. The differences were observed between groups without any incisor and other groups. The NPC angle was higher in men, but this difference was not statistically significant, which is consistent with the findings of Fernandez et al. (7).
The reported average length-range of the canal in previous studies was 8.1 - 16.33 (1-3, 7, 10, 11, 18, 19). In some studies, IF was measured parallel to the horizon (10); therefore, the canal length was recorded shorter than its actual size. In these circumstances, the width of IF was also calculated less than normal. In this study, in order to avoid such an error, the opening of IF was determined by considering its slope in the palate. (Figure 1A) Based on the type of measurements described in the articles, measuring methods in the majority of previous studies were closer to our approach (1, 3, 5-7, 11). In the current study, the average length of the canal was 12.85 ± 2.63 (6.74 - 20.61). According to the statistical findings, age and dental status showed no relationship with the canal length, but the difference in canal length between men and women was significant. It was reported as 13.70 ± 2.52 in men and 12.25 ± 2.54 in women. These findings are consistent with previous studies (3, 5-7, 10, 11).
Regardless of racial differences, the kind of measurement technique can be a determinant factor in the registered length. The employed method in this study in determining the size of the anteriorposterior dimension of IF resulted in a greater diameter in this opening, and also a higher canal length. (Figure 1A vs. Figure 1C)
The mean anteroposterior dimension of IF and SF opening were registered as 7.51 ± 1.95 and 3.32 ± 1.16 mm (0.91 - 8.38), respectively. However, the average obtained in previous studies reported a lower mean, especially in IF (1, 3, 5, 10).
The study performed by Thakur et al. was based on cases with the size of IF recorded in the axial plane and exactly parallel to the horizon (10). As a result, the opening was estimated smaller than the actual size. The effect of age and gender on the opening size of IF and SF were not consistent in different studies. Some were not significant (10) while some were significant (1, 3). One of the reasons behind larger average and the recorded range of anteroposterior dimension of IF was its different registration method in the present study. This parameter was obtained not only in the sagittal plane considering the opening slope, but also by measurement in the 3D image. The end part of the canal in the palatal level, especially in the buccal wall of the canal, is often indistinct in the sagittal plane. So, usage of 3D image as a complement is very helpful for precise measurement of the actual size of the canal entrance. The longer length and wider entries of the canal in men (the impact of gender on parameters) seems to be due to the larger size of skulls and larger dimensions of cranio-caudal anatomy in men (10).
Since IF diameter is generally less than 6 mm, in cases in which this dimension exceeds 10 mm, pathologic circumstance may be considered (3, 18). In this study, according to the measurement method and the usage of 3D images, some were recorded larger than 10 mm. Although the differences with previous studies (3, 10) were due to measurement methods, patients with anteroposterior diameter openings larger than 10 mm were followed up in order to rule out the presence of any kind of pathologies. There was no evidence of increased size of the orifice due to pathologic factors.
Mardinegar et al. theorized that canal width increased after tooth extraction (similar to what occurs in the maxillary sinus) (17). Although the findings of Liang et al. and Guncu et al. did not support this theory (2, 16), the present study has confirmed Mardinegar’s theory (17). Antero-posterior dimensions of SF and IF showed significant differences between edentulous groups and others, which emphasized the influence of the absence of central incisors.
Through this study, up to four entries in the axial plane were found at the nasal level, this finding is in accordance with reports of Liang et al., Thakur et al., and Mraiwa et al. (2, 10, 18). Sicher reported six separate entrances (21). Additional foramen is known as foramina of scarpa. However, Song et al. and Jacob et al. reported only two foramens and questioned foramina of scarpa as real additional nasopalatine foramina (19, 20). In this study, the frequency of openings at the nasal level showed significant differences by age and sex. The most common type with one opening was in 171 cases (52.8%), second was two openings in 143 (44.1%) and three openings in 10 cases (3.1%). Therefore, this finding agrees with previous studies (1, 3, 5). In contrast to these studies, Song et al. believed that there was always one IF and two SF (19). Fernandez et al. also reported an IF and two SF as the most common (7). These anatomical differences seem to be mostly due to racial differences. The number of orifices of NPC in the palate in this study was one entry in 323 cases (99.1%) and two entries in three cases (9%). Kajan and her colleagues showed similar results among the Iranian population (6).
The most common anatomic variation type of canal in the coronal plane through this study was Y-type in 163 patients (50%), with a slight difference. Single-canal with 155 patients (47.5%) was the second and two separate parallel canals were found in only eight cases (2.5%). The result of a study conducted by Fernandez et al. (7) was similar to our study, but Sekerci et al. and Bornstein et al. reported single canal at a higher degree of prevalence (3, 5). However, in all these papers, the difference in the prevalence of single-canal and Y-type was very small which could be negligible. The study of Etoz et al. determined only two single canal modes and two canals mode separately (1).
Thakur et al. mentioned the division at the middle third as the most frequent form (51%), and 47% were found in the upper third. Only two canals division points were in the lower third (10). Their findings were compatible with ours. In the current study, middle third was the most common form with a diversity of 51.5% in cases, while the upper third was the second with 46/8% and the lower third was in the third degree of prevalence with 1.7%. Based on Chi-square test, statistically significant relationship existed between dental status and the location site of NPC furcation.
This study and measurements showed significant anatomical variations in the size, morphology and location of NPC Cylindrical was the most common shape followed by funnel-shape, hourglass, and spindle. It also presented the important role of 3D imaging and anatomic landmark evaluation in different treatment plans, including implants, and removal of pathology in the region. The results suggest significant relationship between NPC, and gender and dental status. The effect of age was not as significant as gender and dental status.