1. Introduction
Hyperparathyroidism is an endocrine disorder, characterized by increased level of circulating parathyroid hormone (PTH). Increased serum PTH leads to excessive bone resorption by osteoclasts that in turn wash out calcium from the skeleton. Primary hyperparathyroidism (PHPT) is usually due to a benign tumor (adenoma) of one of the four parathyroid glands that secretes excessive PTH (1).
The PHPT occurs two to three times more commonly in women than in men, and mainly in those of 30 to 60 years of age (1). The most common complaints of these patients are weakness, anorexia, nausea, vomiting, constipation, abdominal pains, muscular and joint pains, polyuria, polydipsia, and emotional instability (2). Furthermore, a variety of osseous changes may be present that include metastatic calcification, subperiosteal erosion, brown giant cell lesion, and rarely osteosclerosis (2). Considering the rarity of osteosclerosis in PHPT, we report this case with osteosclerosis in the jaws and skull.
2. Case Presentation
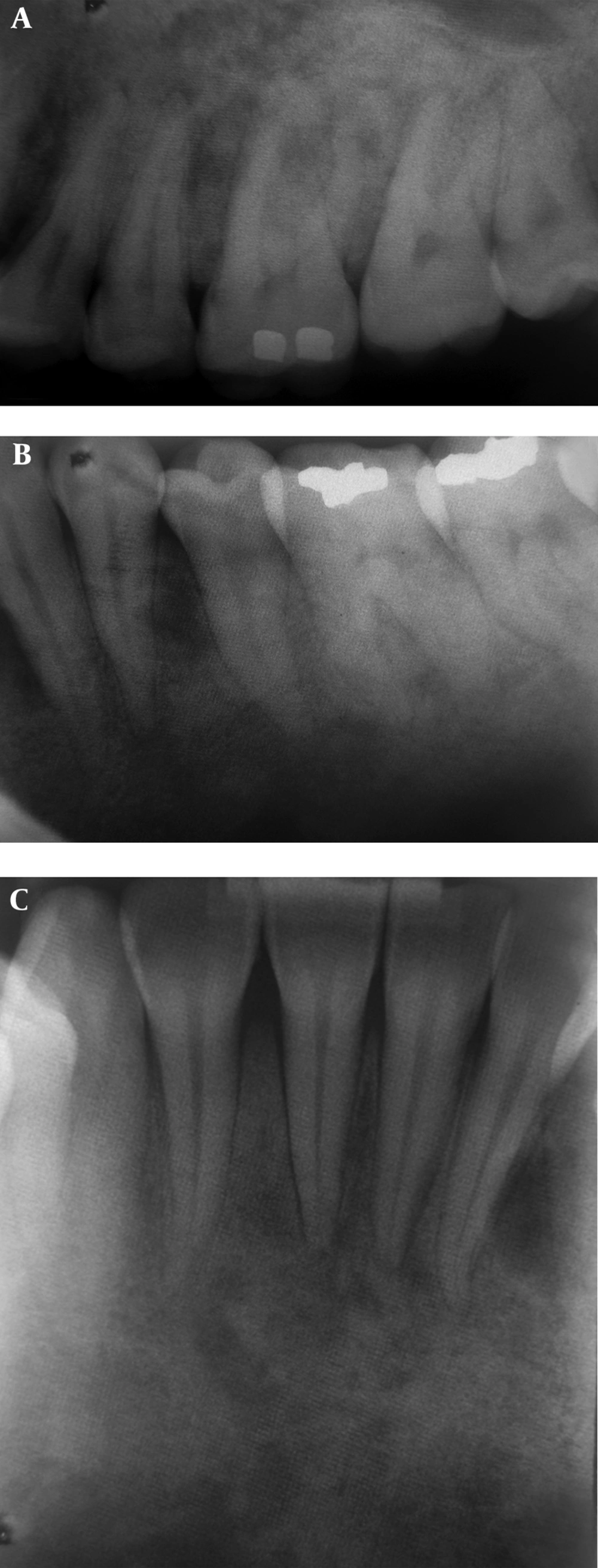
A 34-year-old woman was referred to our dentomaxillofacial radiology center in order to perform a panoramic radiography for dental treatment in March 2012. In panoramic view, we found diffuse sclerosis with a flocculent appearance in the jaws. The width of the mandibular canal was normal; however, the cortical border of the canal was not apparent. In addition, the roots of the teeth were obscured by sclerosis to some extent (Figure 1). Therefore, we undertook further periapical radiography for greater evaluation of this area and found diffuse sclerosis in these views, too. There was also obscured lamina dura and normal periodontal ligament (PDL) space. No caries or periapical lesions were detected (Figure 2A - C). In the posteroanterior skull view, increased density with flocculent appearance was found (Figure 3).
Sclerosis in periapical views. A, Sclerosis in the posterior area of the maxilla and less evident lamina dura of the teeth with normal PDL. B, the posterior area of the mandible and less evident lamina dura of the teeth with normal PDL. C, Sclerosis in sclerosis in the anterior area of the mandible.
In order to make an accurate diagnosis, the patient’s complete medical history was taken, and it was determined that the patient had been diagnosed by PHPT since two years ago. She had had severe pain in her lower back and lower extremities for a long time. Her family physician had referred her to a rheumatologist to perform proper diagnostic laboratory tests in April 2011.
Her serum levels of calcium (Ca), PTH, and alkaline phosphatase (ALP) were significantly higher than normal limits; however, the results of other blood tests, including renal function tests, were in normal range. Hence, with suspicion of hyperparathyroidism, ultrasonography of the neck region was performed. Ultrasonographic evaluation revealed a 34×22×17 mm mass in the right lower parathyroid gland, and parathyroid adenoma was considered as the first differential diagnosis. Bone mineral density (BMD) was measured in September 2011, and the patient’s T-score and Z-score for the lumbar spine and the femoral neck region were reported to be -3.3 and -3.8, respectively, which were consistent with osteoporosis in both regions. In October 2011, excisional surgery of the mass was performed and, after histopathologic examination, a diagnosis of parathyroid adenoma was confirmed.
After surgery, she had hypocalcemia and medical treatment with calcium and vitamin D supplements (3-4 tablets per day) and calcitriol (1 tablet per day) was started. In addition, serum levels of Ca, ALP, and PTH were measured monthly and showed a gradual decremental pattern while the dose of calcium was tapered gradually (to one tablet per day) and calcitriol was stopped after ten months. The patient’s back and lowers extremities pain decreased, too. In March 2012, the BMD measurement was repeated, and the T-score was -0.9 in the lumbar spine region, which was in the normal range, while the Z-score was -1.4 in the femoral neck region, consistent with osteopenia. This examination indicated a significant improvement in bone density compared with the pretreatment phase.
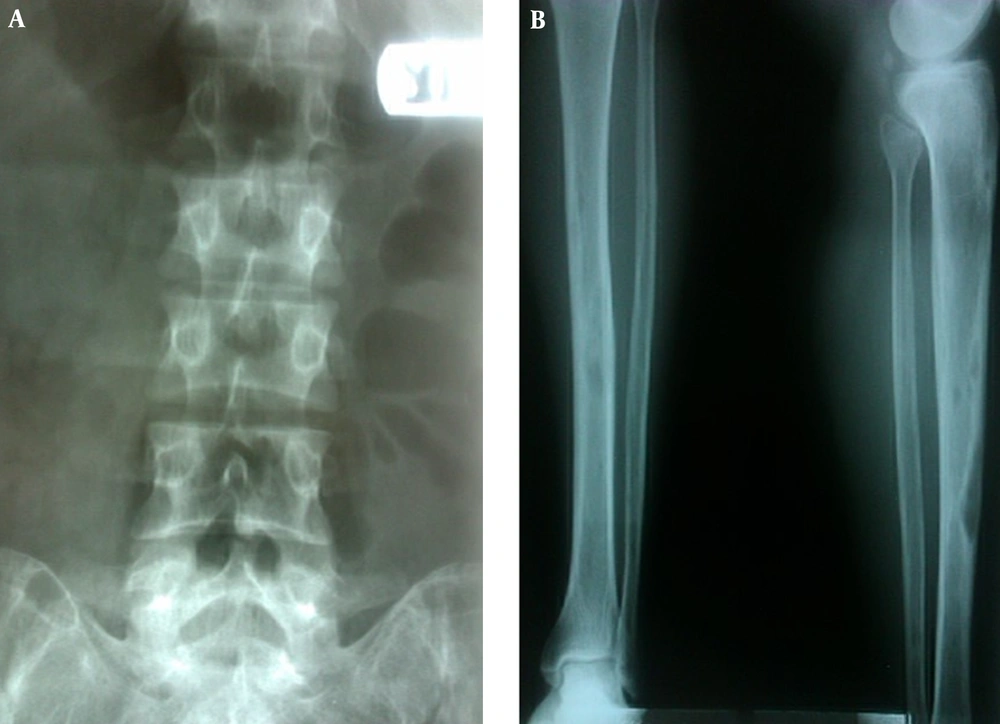
Unfortunately, a panoramic view before diagnosis and treatment of this patient was not available, and therefore, we could not compare the bone density of the jaws before and after treatment. However, we found osteoporosis in her pretreatment radiographies of spine and leg (Figure 4 A, B). The importance of this case report is that regarding osteoporosis of patient previous to treatment of PHPT, the best expected response will be a normal bone density while the patient showed sclerosis in the panoarmic and skull X-rays after treatment which is a rare and unusual phenomenon.
3. Discussion
The PHPT is a relatively common endocrine disorder, which is usually presented by incidental detection of hypercalcemia (1, 3). Although osteitis fibrosa is the characteristic presenting abnormality, in recent years, this skeletal disorder has become rare as the first presenting feature. However, osteopenia is still a common and important feature of PHP, and histopathologic studies and measurements of BMD have demonstrated stimulated bone resorption and a high-turnover bone loss, which is more dominant in cortical bones than in cancellous bones (3).
The PHPT is characterized by decalcification of the bone and is especially prominent in the subperiosteal region, leading to a granular appearance of the calvarium due to the loss of central (diploic) trabeculae and thinning of the cortical tables in more advanced cases. This change in the normal trabecular pattern results in the classic homogeneous ground glass-like or salt-and-pepper appearance (1, 4).
In jaws, demineralization and thinning of the cortical tables leads to decreased density and the consequent radiolucent appearance of the jaws that contrasts with the density of the teeth. This demineralization and thinning often occur in cortical boundaries such as the inferior border of the mandibular canal and the cortical outlines of the maxillary sinuses (1).
As mentioned earlier, the usual skeletal manifestation, when present, is diffuse osteopenia; osteosclerosis is rare in adults with PHPT (5). On the other hand, in secondary hyperparathyroidism associated with renal osteodystrophy, diffuse osteosclerosis is not uncommon (5).
In children, PHPT has been frequently associated with intense osteosclerosis of the metaphyseal regions, particularly in rapidly growing bones. Localized osteosclerosis mixed with lytic deposits in the skull and in the vertebral bodies adjacent to the endplates, and also increased trabecular bone in the metaphyses of the long bones, has been reported in rare occasions in adults with PHPT; however, the exact mechanism of bone sclerosis in PHPT has not been clearly defined (5). An experimental study has demonstrated the production of dense metaphyseal bone in rats given small doses of PTH over an extended period, which was confirmed quantitatively by BMD measurement. In addition to stimulating osteoclastic activity and bone resorption, PTH has been shown to stimulate osteoblastic activity and to increase bone-forming surfaces (5).
Very rare cases of focal hyperostotic lesions (or focal osteosclerosis) have been described in patients with PHPT, and its mechanism has remained unknown (6). Although focal osteosclerosis was observed in the skull of some patients with PHPT on plain films in the days when diagnosis of PHPT was difficult, osteosclerosis in patients with PHPT has been unusual recently, since diagnosis of PHPT has become increasingly easy (4).
The diseases that can be found in differential diagnosis with sclerosis in hyperparathyroidism are osteopetrosis, renal osteodystrophy, Paget’s disease, and florid cemento-osseous dysplasia (FLCOD).
Osteopetrosis or "marble bone disease" is a congenital condition characterized by a diffuse, bilateral, and symmetric significant increase in the density of all bones. This increased density throughout the skeleton is homogeneous and diffuse (1, 2, 7). However, only the mandible and skull bones showed sclerosis in our patient, and other bones in the skeleton had almost normal or evenly decreased density.
Bone changes in renal osteodystrophy result from secondary hyperparathyroidism due to chronic renal failure (1). Affected patients often have increased levels of PTH secondary to a prolonged low serum level of calcium as a result of impaired calcium absorption and a high serum level of phosphor, resulting from a reduction in renal phosphorus excretion. Skeletal changes include generalized loss of bone density, thinning of bony cortices, and occasionally, an increase in bone density (1). In our case, laboratory data revealed no renal disease.
Paget’s disease is seen most frequently in Great Britain and Australia, whereas it is rare in Africa and Asia (1, 7). The affected bones become enlarged and commonly deformed, resulting in bowing of the weight-bearing bones, such as the legs, curvature of the spine, and enlargement of the skull and the jaws (monkey-like) (7).
Malocclusion may occur due to the separation and movement of teeth. Serum levels of ALP are severely increased in most cases (1). Our patient did not have enlargement and deformity of the bones, as seen in Paget’s disease. She had a mild increase in serum levels of ALP (up to three times the upper limit of normal), but it was not as severe as the increase in ALP seen in Paget’s disease.
Florid osseous dysplasia lesions are usually bilateral and present in both jaws. However, the mandible is the more common location when the lesions are present in only one jaw. The lesions occur above the inferior alveolar canal of the mandible. They usually have well-defined peripheries and sclerotic borders that can vary in width, and also a soft tissue capsule, which may not be apparent in mature lesions (1, 2, 8). In our case, not only the area above the inferior alveolar canal, but also the area under this canal was involved. In addition, there was no lesion with a well-defined border or soft tissue capsule because the sclerosis had a more disseminated pattern. Furthermore, FLCOD only involves the jaw, but our patient had skull involvement, too.
In this case, the development of sclerosis in the jaws and skull radiographs has been demonstrated in a patient with PHPT. Although the association is rare, a causal relationship between parathyroid hormone excess and osteosclerosis has been suggested due to clinical and radiographic findings.