1. Background
Radiographers understand the importance of getting the most diagnostic information from as few radiographs as possible. In the world of pediatric scoliosis imaging, pediatric orthopedic surgeons, radiologists and orthotists must obtain more than just spine data from each and every radiograph.
Scoliosis is a lateral curvature of the vertebral column in the coronal plane. Until the end of the 19th century, scoliosis was studied and measured by photography and scoliometer systems (1). After X-rays were discovered, their medical uses soon followed and the technique of radiography evolved (2). Radiology is a standard modality for the evaluation of pre-screened individuals and for following the progress of curves in individuals with scoliosis (3).
Whole spine scanography (WSS) is a radiological examination that exposes the whole body to x-ray radiation. WSS is often repeated during the treatment period, which results in a much greater radiation exposure than that in routine x-ray examinations (4). Scoliosis patients routinely undergo sequential studies, and it is estimated that the typical patient with scoliosis will have approximately 22 radiological examinations over a 3-year treatment period (5). Whole spine image is taken using 14 × 36 inch grid cassettes with film in the film-screen processing system, but digital radiographic system uses auto image paste methods. The auto image paste method (AIPM) establishes the top-to-bottom height before scanning, acquires images by moving the detector and X-ray tube, and then pastes together the acquired images. On analog devices, the film-screen method projects the whole body on a sheet of film. Conversely, the digital method involves the use of a detector, and applies AIPM, which assembles multiple images of each body part in order to overcome the size limitations of the detector.
2. Objectives
The aims of the current study were to evaluate the effective dose of WSS using AIPM, and to confirm the effectiveness of the method by comparing the effective dose (ED) in AIPM with the effective dose resulting from the film-screen method. In addition, this study will extract the DAP-ED conversion factor which is easily available for patient dosimetry by analyzing the correlation of DAP with ED.
3. Patients and Methods
WSS is a radiological examination that observes the postero-inferior and antero-superior displacement of the pelvis, the internal and external rotation of pelvic bones, supero-inferior rotation of scapular bones and analyzes the asymmetric shape of the whole body. This study was carried out with 50 patients who underwent examinations for diagnosis of scoliosis at the hospital from November 2012 to January 2013. It evaluated organ dose and ED to the patients. This study evaluated all the patients who visited the clinic to diagnose scoliosis during the study period.
The patients consisted of 28 males and 22 females. The average age of the patients was 55.5 years, the average patient weight was 64.1 kg, and the average BMI was 22.89 kg/m2 (Table 1).
| Patients’ Characteristics | Height, cm | Weight, kg | Age, y | BMI, kg/m2 |
|---|---|---|---|---|
| Mean | 166.7 | 64.1 | 55.5 | 22.8 |
| Standard deviation | 7.4 | 11.4 | 11.8 | 2.8 |
| Minimum value | 151.5 | 43.6 | 26 | 17.4 |
| Maximum value | 180.2 | 88.7 | 74 | 30.3 |
aAbbreviation: BMI = body mass index.
A Definium 6000 digital radiography system (GE medical systems, Milwaukee, US) was used to scan the entire backbone of each patient from the cervical spine to the coccyx. The radiography system was composed of a non-tiled 41 × 41 cm amorphous silicon photodiode with a cesium iodide scintillator and a thin film transistor array (2048 × 2048 pixels and 0.2 mm pixel pitch) (6). Auto exposure control (AEC) was used for AP projections, with a tube voltage of 80 kVp, while lateral projections used both the AEC mode at 85 kVp and the manual exposure control mode at 92, 93, and 95 kVp. All of the antero-posterior projections were acquired in AEC mode, while 60% of lateral projections were acquired in AEC mode. In AEC mode, the exposure dose is determined by automatic process of the diagnostic medical equipment. However, in manual mode, the radiographer set up the exposure parameter of C-spine, T-spine and L-spine lateral projection regarding the thickness of the patients.
In LAT projection of WSS, for obese patients, it may not generate enough exposure to make adequate diagnostic information. This is because the considerable difference between C-spine thickness and L-spine thickness in obese patients makes an uneven density image in digital image processing.
This error of system is the reason why some obese patients have to retake the X-ray image in examinations. Since obese patients have bigger thickness difference between C-spine and L-spine in lateral projection than AP projection, manual mode was used to prevent the retakes for obese patients especially in lateral projection based on the radiographer’s judgment.
Before the WSS examination, the radiographer checked the patient’s spine length from the cervical spine to the coccyx. They decided how many raw images should be taken for each patient. Once they set up the range from starting point to end point, including the patient’s C-spine and pelvic bone prior to exposure, the equipment determines the number of shot image by dividing the total length of scan range. The starting point should be at the level of about 10 cm superior to the external auditory meatus covering all seven cervical spines and the end point should be at the level of pubic symphysis covering the coccyx.
Scanning parameters were as follows: X-ray target angle, 12.5°; Anode Rotation Speed, 10,800 rpm; and focal spot size, 0.6 mm/1.25 mm; original filter, tube insert 0.8 mm Al equivalent and tube housing 0.3 mm Al equivalent.
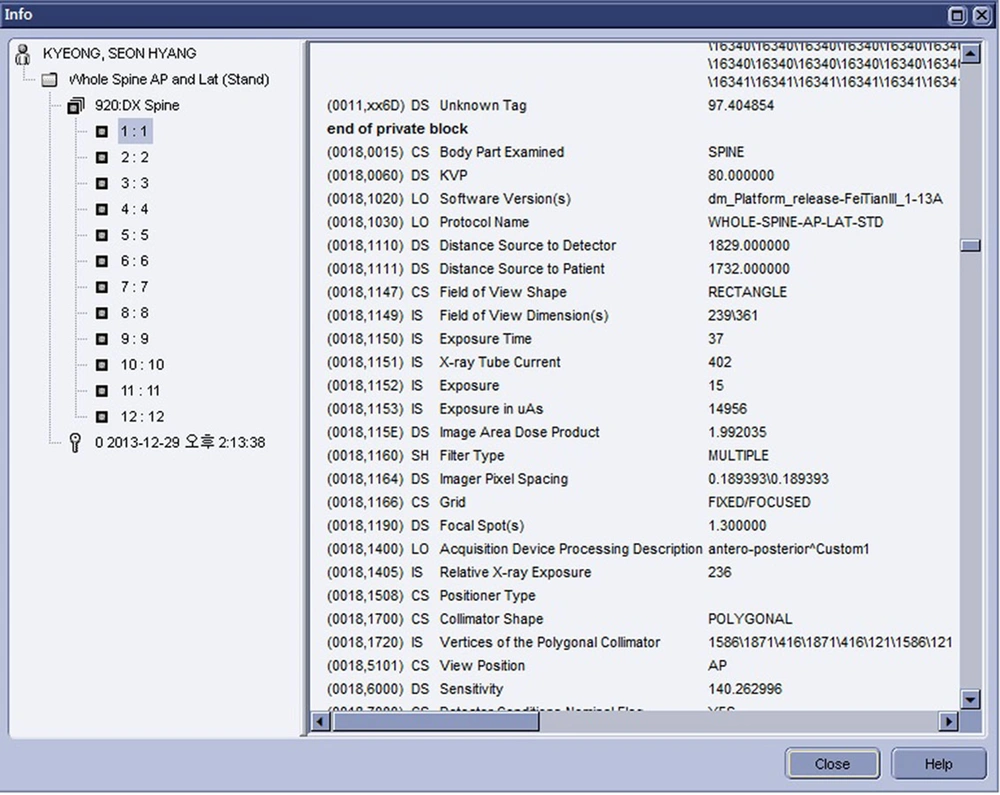
Prior to applying AIPM, digital imaging and communications in medicine (DICOM) tags for the dose area product (DAP) of each image were collected by investigating the DICOM tag data of each partial image, and additional information was identified including X-ray field size, tube voltage, the use of AEC mode, and distance between X-ray tube and detector (7). DICOM tag data of each image was found on a Centricity CA1000 workstation (GE Medical Systems, Milwaukee, US). Tag 0018,115E revealed the information for DAP as well as tube voltage, tube current, radiation time, and distance from the source to the detector (Figure 1) (8).
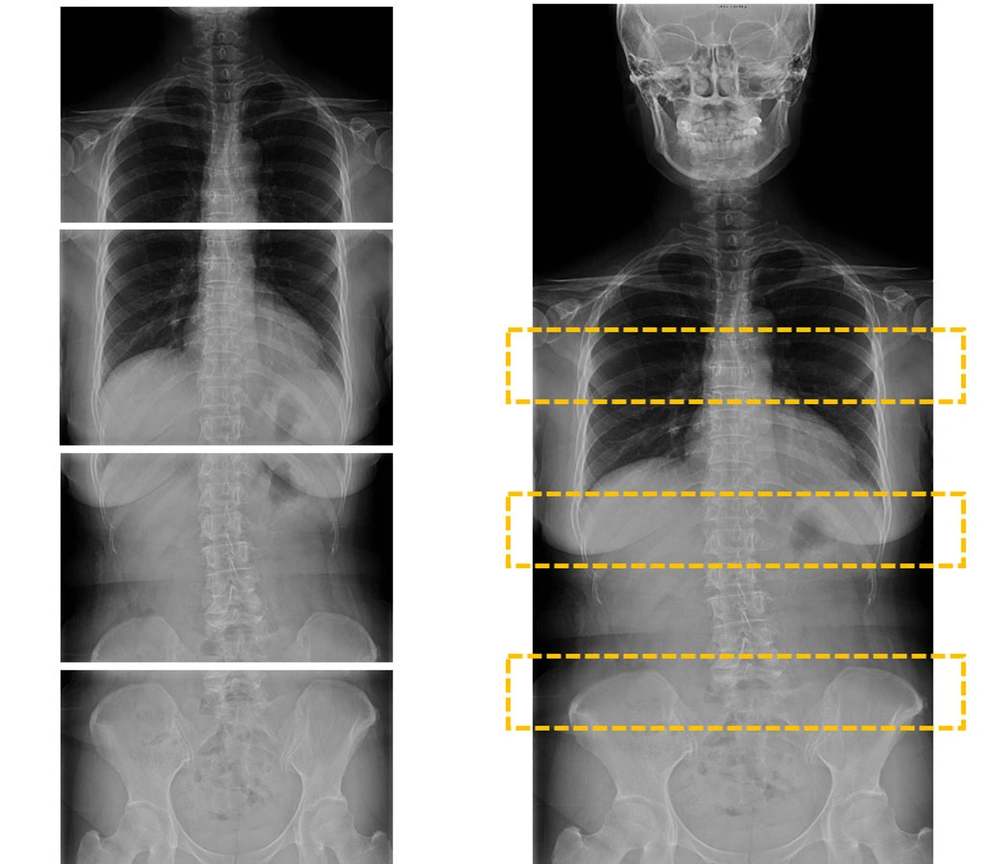
The AIPM established the top-to-bottom height before scanning, acquired images by moving the detector and X-ray tube, and then pasted together the acquired images. The device used in this study produced a 90 cm-long whole spine scanography within 12 seconds by acquiring and pasting together three partial images (Figure 2).
To evaluate ED of AP and lateral projections for each patient, ED was calculated using PCXMC v2.0 (STUK, Finland), a PC-based Monte Carlo program for calculating patient radiation doses in medical X-ray examinations. The PCXMC 2.0 hermaphrodite mathematical phantoms were based on the work of Cristy and Eckerman (9). The tissue weighting factors and effective dose calculations were based on ICRP 103 (10). Factors for evaluating effective doses were derived from information in the DAP of DICOM tag data. The PCXMC computer simulation used patient height, weight, gender, x-ray target angle, filter information, detector size, distance between detector and x-ray tube, tube voltage, and DAP information.
These data were used in analysis of frequency, group average analyses, tendency analysis, and correlation analysis by SPSS V20.0 (IBM Corporation, New York, USA).
4. Results
For the whole spine scanography of the 50 patients, an average of 6.1 images were taken for reconstruction of AP projections, while an average of 6.5 images were acquired for reconstruction of lateral projections, which equated to the acquisition of 7.37% more images in later versus AP projections. For female patients, the average DAP value was 2559 dGy cm2 for AP projections, and 9507 dGy cm2 for lateral projections. For male patients, the DAP was 5591 dGy cm2 for AP projections, and 12975 dGy cm2 for lateral projections. For female patients, the ED was 0.43 mSv for AP projections, and 0.53 mSv for lateral projections. For male patients, ED was 0.78 mSv for AP projections, and 0.78 mSv for lateral projections.
For all patients, the average AP projection DAP was 4257 dGy cm2, while the average lateral projection DAP was 11449 dGy cm2, which implied that the lateral projection DAP was 168% larger than the AP projection. Furthermore, the average ED of AP projections was 7% higher than the average ED of lateral projections (Table 2).
| Gender | AP DAP (dGy cm2) | LAT DAP (dGy cm2) | AP ED (mSv) | LAT ED (mSv) |
|---|---|---|---|---|
| Female (n = 22) | ||||
| Mean (SD) | 2559.00 (711.81) | 9507.09 (2794.20) | 0.43 (0.10) | 0.53 (0.14) |
| Range (Min - Max) | 2699.75 (1542.64 - 4242.39) | 10865.84 (5197.34 - 16063.18) | 0.38 (0.28 - 0.66) | 0.5 (0.36 - 0.86) |
| Var | 506683.21 | 7807564.61 | 0.01 | 0.02 |
| Male (n = 28) | ||||
| Mean (SD) | 5591.95 (2200.78) | 12975.88 (2493.97) | 0.78 (0.27) | 0.78 (0.21) |
| Range (Min - Max) | 10370.93 (2589.83 - 12960.76) | 11420.1 (7740.83 - 19160.93) | 1.23 (0.38 - 1.61) | 0.8 (0.46 - 1.26) |
| Var | 4843460.94 | 6219896.31 | 0.07 | 0.04 |
| Total (n = 50) | ||||
| Mean (SD) | 4257.45 (2280.09) | 11449.61 (3130.28) | 0.62 (0.28) | 0.67 (0.22) |
| Range (Min - Max) | 11418.12 (1542.64 - 12960.76) | 13963.59 (5197.34 - 19160.93) | 1.33 (0.28 - 1.61) | 0.9 (0.36 - 1.26) |
| Var | 5198833.27 | 9798695.17 | 0.07 | 0.05 |
aAbbreviations: AP, antero-posterior; DAP, dose area product; ED, effective dose; LAT, lateral; Max, maximum; Min, minimum; SD, standard deviation; Var, variance.
Evaluation of the impact of AEC mode on lateral projections revealed that using AEC mode, the average DAP value was 10,439 dGy cm2, and the corresponding ED was 0.60 mSv. However, using the manual mode, the average DAP value was 12964 dGy cm2 and ED was 0.77 mSv. Thus, using the manual mode resulted in 24% higher DAP values and 27% higher ED values.
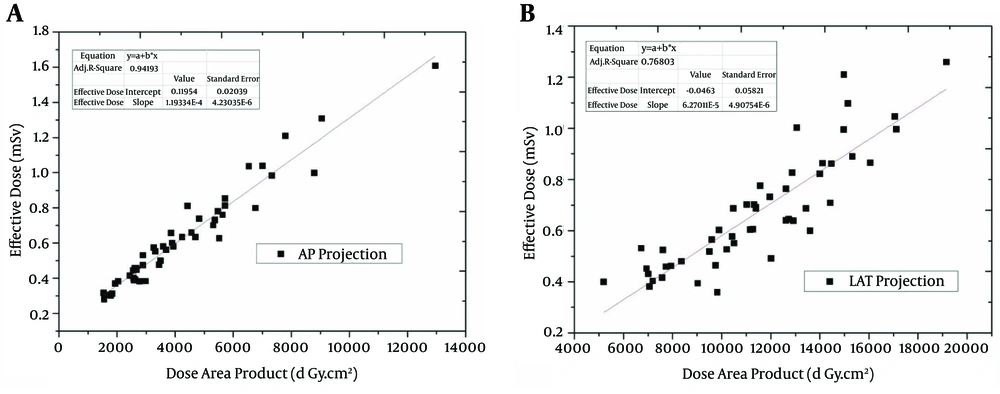
Analysis of the correlation of all patients revealed that R2 values for the correlation of DAP and ED were 0.94213 and 0.76803 for AP and lateral projections, respectively, which indicated a significant correlation (Figure 3).
DAP is converted to ED by the following equation, where the conversion factor b values are 0.119334E-4 in AP projection and 6.27011E-5 in LAT projection and the constants are 0.11954, and −0.0463, respectively.

y = ED (mGy), x = DAP (dGy cm2), a = constant, b = conversion factor.
Pearson correlation coefficients resulting from analysis of the correlation of effective dose and BMI were 0.771 and 0.546 for AP and lateral projections, respectively, which indicated a higher significant correlation for AP projections (P < 0.01) (Table 3).
| Group | LAT DAP, dGy cm2 | LAT ED, mSv |
|---|---|---|
| AEC (n = 30) | ||
| Mean (SD) | 10439.99 (3412.91) | 0.60 (0.23) |
| Range (Min - Max) | 13963.59 (5197.34 - 19160.93) | 0.9 (0.36 - 1.26) |
| Var | 11647999.32 | 0.05 |
| Manual (n = 20) | ||
| Mean (SD) | 12964.05 (1862.27) | 0.77 (0.17) |
| Range (Min - Max) | 6848.27 (10212.44 - 17060.71) | 0.61 (0.49 - 1.1) |
| Var | 3468072.37 | 0.03 |
| Total (n = 50) | ||
| Mean (SD) | 11449.61 (3130.28) | 0.67 (0.22) |
| Range (Min - Max) | 13963.59 (5197.34 - 19160.93) | 0.9 (0.36 - 1.26) |
| Var | 9798695.17 | 0.05 |
aAbbreviations: AEC, auto exposure control; DAP, dose area product; ED, effective dose; LAT, lateral; Max, maximum; Min, minimum; SD, standard deviation; Var, variance.
For normal BMI patients (BMI: 18.5 kg/m2 ~ 23 kg/m2), the Pearson correlation coefficients of total DAP for antero-posterior and lateral projections were respectively 0.739, and 0.638 (P < 0.05) and the Pearson correlation coefficients of total effective dose for AP and lateral projections were 0.638 (P < 0.01), and 0.522 (P < 0.05), respectively.
For obese patients (BMI > 23 kg/m2), the Pearson correlation coefficients of total DAP for AP and lateral projections were 0.091, and 0.017 (P < 0.01), respectively and the Pearson correlation coefficients of total ED for AP and lateral projections were 0.591 (P < 0.01), and 0.078 (P < 0.05), respectively.
The correlation coefficients of AEC with BMI also indicated the significance level of 0.586 (P < 0.01). The correlation of DAP with ED in each statistical group is mentioned in Table 4.
| Group | Correlation of DAP with ED | Significance Level |
|---|---|---|
| Total | ||
| AP projection | 0.971 | 0.01 |
| LAT Projection | 0.879 | 0.01 |
| Female | ||
| AP projection | 0.951 | 0.01 |
| LAT Projection | 0.841 | 0.01 |
| Male | ||
| AP projection | 0.954 | 0.01 |
| LAT Projection | 0.852 | 0.01 |
| Obese BMI | ||
| AP projection | 0.953 | 0.01 |
| LAT Projection | 0.764 | 0.01 |
| Normal BMI | ||
| AP projection | 0.957 | 0.01 |
| LAT Projection | 0.924 | 0.01 |
| AEC Mode | ||
| AP projection | 0.96 | 0.01 |
| LAT Projection | 0.887 | 0.01 |
| Manual Mode | ||
| AP projection | 0.947 | 0.01 |
| LAT Projection | 0.79 | 0.01 |
aAbbreviations: AEC, auto exposure control; AP, anterior-Posterior; BMI, body mass index; DAP, dose area product; ED, effective dose , BMI, body mass index, AEC, auto exposure contro.
5. Discussion
The calculated ED following use of AIPM for all patients was 0.6276 mSv and 0.6716 mSv for the AP and lateral projections, respectively, which were lower than the 0.798 mSv ED for the AP projection, and higher than the 0.597 mSv ED for the lateral projection reported by Mogaadi et al. (11). However, using AEC, ED of lateral projections was 0.605 mSv, which was slightly different. Accordingly, the results indicated that use of AEC mode with AIPM contributed significantly to a reduction in the exposure dose.
In WSS examinations, the conversion factors to ED from DAP in AP projections and lateral projections were 0.119334E-4, and 6.27011E-5, respectively. These conversion factors could be simply used to convert DAP value into ED in a clinical field. By using the DAP-ED conversion factor, one can easily estimate the patient-specific ED value and use it as the reference value for reducing patient’s dose.
On analysis of BMI, it can be detected that the Pearson correlation coefficients in AP projections are higher than those in lateral projections. So, it is considered that ED for patients in AP projections is higher than that in lateral projections.
The reason why the correlation of DAP with BMI in AP projections are higher than that in lateral projections is considered due to the increase of exposure area in AP projections.
In obese patients, since the difference of exposure area between AP projections and lateral projections is not so big, the correlation of BMI with DAP value is low. In normal weight patients, since there is a considerable difference of exposure area between AP projections and lateral projections, the correlation of BMI with DAP value is considered as high. Furthermore, the use of automatic exposure control is considerably related to BMI.
In the analysis of correlation of DAP with ED regarding to sex and BMI, there is a high correlation between DAP and ED, especially higher in LAT projection than AP projection. Therefore, in WSS examination, an effort to reduce DAP will help reduce the patient’s effective dose. Moreover, since this correlation of DAP with ED is higher in AEC mode than the manual mode, using AEC can be applied to reduce the patient’s effective dose.
Compared to the single exposure method used with the film-screen method, use of AIPM exhibited only a slight difference in ED. However, the significant reduction in exam time and convenience to both the examiner and patient contribute to the value of AIPM.
The study conducted by Mogaadi et al. (11) was carried out among patients between 16 years and 22 years and Hansen et al. (12) study was done among patients between 13 years and 18 years. Compared to these studies, the subjects of this study were adults aged between 26 years and 74 years. So, given the age of the patients, most of the patients were large-bodied adults.
Considering this situation, it is assessed that in the WSS examinations, using AIPM is more useful to reduce the patient exposure dose than using the single exposure film-screen method.
ED of this study is higher than the studies performed by Hallen et al. (13) and Chamberlain et al. (3). It is because these two studies used wedge-shaped aluminium filter resulting in a reduced exposure dose by weakening the strength of x-ray beam exposed to the chest region. This method is only available in single exposure method, and not in AIPM (Table 5).
| Study | Number of Patients | Age, y | Effective Dose (Min-Max) | Method |
|---|---|---|---|---|
| Hallen et al. (13) | 7 | 9 - 25 | PA and lateral: 0.12 mSv | Single exposure |
| Chamberlain et al. (3) | 61 | 9 - 55 | AP: (0.14 - 0.18) mSv | Single exposure |
| Lee et al. (2) | 54 | 4 - 17 | PA: (0.081 - 0.123) mSv; lateral: (0.124 - 0.207) mSv | Single exposure |
| Geijer et al. (14) | Alderson phantom | PA: 0.16 mSv | Digital fluoro-graphic image reconstruction | |
| Mogaadi et al. (11) | 13 | 16 - 22 | AP: 0.798 (0.545 - 1.305) mSv; lateral: 0.597 (0.344 - 1.187) mSv | Single exposure |
| Hansen et al. (12) | 22 | 13 - 18 | PA female: 0.97 mSv; PA male: 0.65 mSv; lateral female: 1.2 mSv; lateral male: 1.2 mSv | Single exposure |
| This Study | 50 | 26 - 74 | AP female: 0.43(0.28 - 0.66) mSv; AP male: 0.78 (0.46 - 1.26) mSv; lateral female: 0.53 (0.36 - 0.86) mSv; lateral male: 0.78 (0.46 - 1.26) mSv; AEC used lateral: 0.6 (0.36 - 1.26) mSv; AEC not used lateral: 0.77(0.49 - 1.1) mSv | Auto Image Paste |
This study was performed only among adult patients aged from 26 to 74, and did not include pediatric patients. So, this study has an important limitation, and further studies for pediatric patients should be performed in the future.
In conclusion, to reduce patient exposure dose, it is essential to consider the detector response characteristics and the final image quality of the whole spine scanogram. In particular, understanding the exact characteristics of the device, and applying AEC mode are useful for reducing patient exposure dose.