1. Background
Primary tumors and tumor-like lesions are rare in the clavicle which is an unusual bone with development and structures different from other tubular bones in many aspects (1). This bone is the first to ossify in the embryo probably at five months. In the first five years of life, further development happens in the diaphysis from intramembranous ossification, and later, typical endochondral ossification of tubular bone occurs at the sternal and acromial ends. Radiologically, evident epiphyses only appear at the sternal end while no epiphysis center appears at the acromial end. The clavicle interior is occupied by coarse cancellous bone with actually no cavity (2). The clavicle has sparse vascular supply with minimal red marrow surrounded by thick cortices of compact bone. These unusual features in the development and structures may account for the uncommon occurrence of tumors and tumor-like lesions in the clavicle (1, 2). Bone lesions in the clavicle are rare and not common even though every kind of bone lesion which occurs in the skeleton bone has been described in the clavicle. Many clavicular lesions have been reported in the literature despite that most articles are of single case reports or very small number of patients (3-15) even though some larger samples have been reported (1, 2, 16). The great variety of diseases in the clavicle makes radiological diagnosis challenging especially because of limited experience of individual radiologists with these tumors and tumor-like lesions.
2. Objectives
This study investigated patients with tumors and lesions resembling tumors in the clavicle over a period of forty years and analyzed the clinical and imaging characteristics of these diseases in order to increase the diagnostic accuracy.
3. Patients and Methods
This retrospective study was approved by the ethics committee of our hospital with all the patients given their signed informed consent. Between January 1963 and December 2018, patients with tumors in the clavicle confirmed by pathology were enrolled. Inclusion criteria were patients with clavicle tumors who had radiological examinations including plain radiography, computed tomography (CT) scan and magnetic resonance imaging (MRI). Exclusion criteria were infectious diseases, non-infectious inflammatory diseases, trauma and fracture of the clavicle. Age, sex, radiological signs and location of the tumor at the clavicle of the patients were analyzed and compared. For CT scanning, the Siemens 64-detector scanner (Siemens, Germany) was used with the scanning parameters of slice thickness 5 mm, slice interval 5 mm, tube voltage 120 kV, tube current 260 mA, window width 2000 and window level 500. For MRI scanning, the Siemens symphony 1.5 T scanner was used with the following parameters: T1 weighted image (T1WI): repetition time (TR)/echo time (TE) 690 ms/12 ms, T2WI: TR/TE 5000 ms/60 ms, slice thickness 5mm, slice interval 5 mm, field of view 24 cm × 24 cm, and matrix 256 × 256.
3.1. Statistical Analysis
Statistical analysis was performed with the SPSS ver. 24.0 (IBM, Chicago, IL, USA). Enumeration data were presented as number and percentages and tested with Fisher exact probability method, chi-square for paired t-test for significant difference between benign, malignant and intermediate tumors and other data. The significant P was set as < 0.05.
4. Results
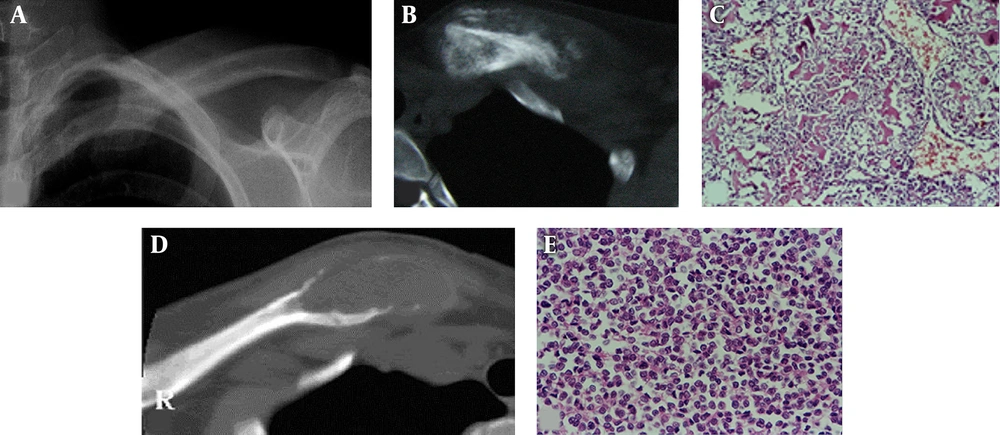
A total of 81 patients with tumors in the clavicle were identified including 49 males and 32 females with an age range of 2 - 76 years of age (mean = 42.6) and a male-to-female ratio of 1.53:1. There were malignant tumors in 50 cases (61.7%), intermediate tumors in 12 (14.8%) and benign tumors in 19 cases (23.5%) (Figures 1-3), with one peak age period of 11 - 20 years in 21 cases (25.9%) and another age peak period of 51 - 60 years in 37 cases (45.7%). Malignant tumors included metastatic tumors (38.3%), plasma-cell myeloma (12.3%), and osteosarcoma (4.9%). The intermediate bone tumors were mainly eosinophilic granuloma (7.4%) and aneurysmal bone cyst (3.7%), and according to the World Health Organization (WHO) classification of tumors of soft tissue and bone, intermediate bone tumors indicate those which are locally aggressive but rarely metastasizing (17). Benign tumors were mainly osteochondroma (6.2%), bone cyst (3.7%) and chondroma (3.7%) (Table 1).
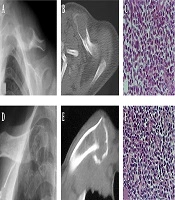
Metastatic tumors. A and B, At the sternal end of the right clavicle, osteolytic bone destruction is revealed with ill-defined margins, pathologic fracture and a soft tissue mass; C, Microscopy of the clavicle in (A) and (B) reveals metastatic adenocarcinoma of the lung with cancer cells forming an adenoid structure surrounded by reactive new bone; D and E, At the middle segment of the left clavicle, osteosclerotic bone destruction is shown with ill-defined margins, apparent periosteal reaction but no soft tissue masses.
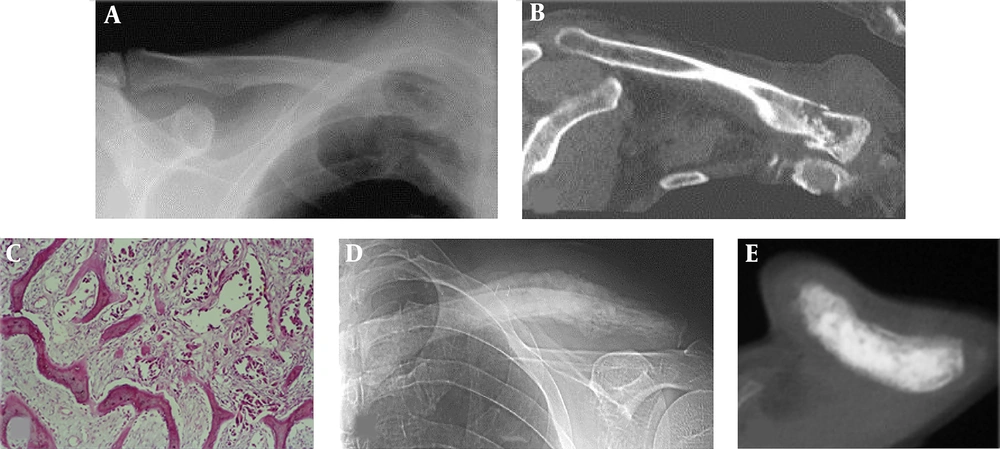
A-C, Eosinophilic granuloma. D-F, plasma-cell myeloma; A-C, An eosinophilic granuloma lesion is demonstrated at the middle segment of the left clavicle with osteolytic bone destruction, ill-defined margins, apparent periosteal reaction but no soft tissue masses (A and B); C, Microscopy of the eosinophilic granuloma shows many Langerhans cells of medium size with eosinophilic cytoplasm and round or oval nuclei which had nuclear groove. Scattered or clustered eosinophils are seen in the background; D-F, A plasma-cell myeloma is shown near the sternal end of the right clavicle with osteolytic, expansile bone destruction, ill-defined margins and pathologic fracture (D and E); F, Microscopically, the lesions of the plasma-cell myeloma are composed of tumor plasmocytes with deviated nuclei.
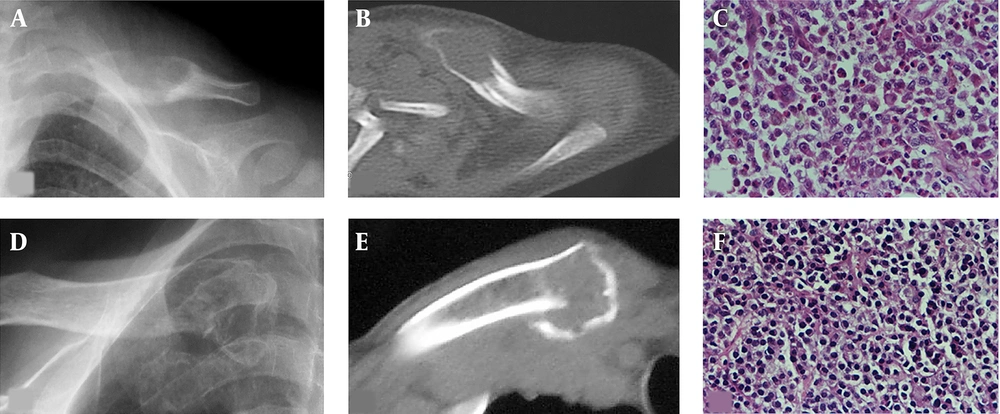
A-C, Osteosarcoma; D and E, Ewing’s sarcoma; A and B, An osteolytic destruction is demonstrated at the sternal end of the left clavicle with ill-defined margins, periosteal reaction, a lot of tumorous bone and soft tissue masses; C, Microscopically, the osteosarcoma is composed of tumor cells and tumor-like bone tissue which is produced directly by the tumor cells; D, An osteolytic, expansile destruction lesion is shown at the sternal end of the right clavicle with ill-defined margins, but no periosteal reaction and soft tissue masses; E, Microscopically, the Ewing’s sarcoma is composed of small round cells of the same size and shape, with few cytoplasm and fine nuclear chromatin.
| Disease | Percentage | M:F | Age range (mean) | Proximal Third | Middle Third | Distal Third |
|---|---|---|---|---|---|---|
| Malignant tumor | ||||||
| Metastatic (n = 31) | 38.3 | 19:12 | 4 - 76 (56.5) | 26 | 3 | 2 |
| PCM (n = 10) | 12.3 | 8:2 | 29 - 67 (57.3) | 6 | 1 | 3 |
| Osteosarcoma (n = 4) | 4.9 | 2:2 | 15 - 60 (39.3) | 3 | 1 | |
| Lymphoma (n = 2) | 2.5 | 1:1 | 34 - 72 (53) | 2 | ||
| Ewing’s sarcoma (n = 2) | 2.5 | 2:0 | 17 - 18 (17.5) | 1 | 1 | |
| Chondrosarcoma (n = 1) | 1.2 | 1:0 | 52 (52) | 1 | ||
| Intermediate tumor | ||||||
| Eosinophilic granuloma (n = 6) | 7.4 | 3:3 | 2 - 32 (15.6) | 3 | 2 | 1 |
| ABC (n = 3) | 3.7 | 1:2 | 15 - 45 (34.3) | 1 | 2 | |
| Giant cell tumor (n = 2) | 2.5 | 2:0 | 25 - 60 (42.5) | 2 | ||
| Chondromyxoid fibroma (n = 1) | 1.2 | 0:1 | 45 (45) | 1 | ||
| Benign tumor | ||||||
| Osteochondroma (n = 5) | 6.2 | 2:3 | 11 - 33 (19.5) | 4 | 1 | |
| Bone cyst (n = 3) | 3.7 | 1:2 | 11 - 15 (12.7) | 1 | 2 | |
| Chondroma (n = 3) | 3.7 | 2:1 | 12 - 36 (21.7) | 1 | 1 | 1 |
| Ossifying fibroma (n = 2) | 2.5 | 1:1 | 13 - 16 (14.5) | 1 | 1 | |
| Osteoid osteoma (n = 1) | 1.2 | 1:0 | 18 (18) | 1 | ||
| Hemangioma (n = 1) | 1.2 | 1:0 | 50 (50) | 1 | ||
| Fibrous histiocytoma (n = 1) | 1.2 | 0:1 | 60 (60) | 1 | ||
| Fibrous dysplasia (n = 1) | 1.2 | 1:0 | 13 (13) | 1 | ||
| Lipoma (n = 1) | 1.2 | 0:1 | 58 (58) | 1 | ||
| Osteoma (n = 1) | 1.2 | 1:0 | 22 (22) | 1 | ||
| Total | 100 | 49:32 | 2 - 76 (42.6) | 50 | 11 | 20 |
Abbreviations: ABC, aneurysmal bone cyst; F, female; M, male; PCM, plasma-cell myeloma.
The mean age was 53.5 years for 50 cases with malignant tumors, 31.4 years for twelve cases with intermediate tumors and 23.7 years for 19 cases with benign tumors. The mean age was 56.5 years for metastatic tumors, 57.3 for plasma-cell myeloma, 39.3 for osteosarcoma, 17.5 for Ewing’s sarcoma, 15.6 for eosinophilic granuloma, and 19.5 for osteochondroma.
The clavicle was divided into three segments as sternal end, middle segment and acromial end with each segment accounting for 1/3 of the clavicle. The location of the lesion was determined according to the position of the lesion center. More malignant tumors occurred in the sternal end than either the intermediate malignant (P = 0.013) or the benign tumors (P = 0.011) (Table 2). Fifty (61.7%) lesions were located at the sternal end, with 38 malignant tumors (76%) including metastatic tumors in 26 cases, plasma-cell myeloma in six, osteosarcoma in three, lymphoma in two and Ewing’s sarcoma in one. Among 81 cases, plain radiography was performed in 39 cases, of whom CT scan was conducted in 31, and MRI scan in 20 (Table 3). The bone destruction on CT imaging was in line with what was found on plain radiography, and the lesion had equal to low signal on T1WI but high signal on T2WI on MRI.
| Tumor | Male | Female | Left | Right | Proximal Third | Middle Third | Distal Third |
|---|---|---|---|---|---|---|---|
| Malignant tumor (n = 50) | 66.0% (33/50) | 34.0% (17/50) | 56.0% (28/50) | 44.0% (22/50) | 76% (38/50) | 8.0% (4/50) | 16% (8/50) |
| Intermediate tumor (n = 12) | 50.0% (6/12) | 50.0% (6/12) | 58.33% (7/12) | 41.67% (5/12) | 33.3% (4/12) | 25.0% (3/12) | 41.7% (5/12) |
| Benign tumor (n = 19) | 52.63% (10/19) | 47.37% (9/19) | 42.11% (8/19) | 57.89% (11/19) | 42.1% (8/19) | 21.05% (4/19) | 36.8% (7/19) |
| P value | 0.464 | 0.464 | 0.565 | 0.565 | 0.003 | 0.173 | 0.074 |
aFisher exact probability test was used. More malignant tumors occurred in the inner area than either the intermediate malignant (P = 0.013) or the benign tumors (P = 0.011). No other significant (P > 0.05) difference existed between any other two features.
| Lytic destruction | Expansile destruction | Sclerotic destruction | Mixed destruction | IDR | PR | PF | STM | |
|---|---|---|---|---|---|---|---|---|
| Metastatic (n = 22) | 15 | 14 | 1 | 6 | 17 | 2 | 4 | 15 |
| PCM (n = 5) | 5 | 4 | - | - | 5 | - | 3 | 3 |
| Osteosarcoma (n = 2) | 1 | 1 | - | 1 | 2 | - | - | 2 |
| Ewing’s sarcoma (n = 1) | 1 | 1 | - | - | 1 | - | - | - |
| EG (n = 4) | 4 | 4 | - | - | 2 | 4 | - | - |
| ABC (n = 2) | 2 | 2 | - | - | - | - | - | - |
| Bone cyst (n = 1) | 1 | 1 | - | - | 1 | - | - | - |
| Osteochondroma (n = 1) | - | - | - | - | - | - | - | - |
| Chondroma (n = 1) | 1 | 1 | 1 |
Abbreviations: ABC, aneurysmal bone cyst; EG, eosinophilic granuloma; IDR, ill-defined rim; PCM, plasma-cell myeloma; PF, pathologic fracture; PR, periosteal reaction; STM, soft tissue mass.
Among 22 cases with metastatic tumors (Figure 1), osteolytic destruction occurred in fifteen cases, and mixed destruction in six cases. Expansile destruction took place in fourteen patients, with pathological fracture in four cases. A soft tissue mass occurred in thirteen cases, with apparent sclerosis and periosteal reaction in one patient. In five patients with plasma cell myeloma (Figure 2), the lesion was osteolytic with expansile destruction, ill-defined margins and thinned cortex in three cases. Pathological fracture occurred in three cases with accompanied soft tissue masses. Among four cases with eosinophilic granuloma (Figure 2), three lesions had well-defined margins, but one lesion had ill-defined margins. In three children, the eosinophilic granuloma lesion was expansile with apparent periosteal reaction and bone shell formation. In the remaining two adult patients, the lesion was limited with slight periosteal reaction and no masses in the soft tissue. Malignant tumors had a significantly (P = 0.003) lower incidence in periosteal reaction but a significantly higher incidence in soft tissue mass than intermediate malignant tumors (Table 4).
| Tumor | Lytic | Sclerotic | Mixed | Expansile | IDR | PR | PF | STM |
|---|---|---|---|---|---|---|---|---|
| Malignant tumor (n = 30) | 73.33% (22/30) | 3.33% (1/30) | 23.33% (7/30) | 66.67% (20/30) | 83.33% (25/30) | 6.67% (2/30) | 23.33% (7/30) | 66.67% (20/30) |
| Intermediate tumor (n = 6) | 100% (6/6) | 0 | 0 | 100% (6/6) | 33.33% (2/6) | 66.67% (4/6) | 0 | 0 |
| Benign tumor (n = 3) | 66.67% (2/3) | 33.33% (1/3) | 0 | 66.67% (2/3) | 33.33%(1/3) | 0 | 0 | 0 |
| P value | 0.391 | 0.170 | 0.463 | 0.193 | 0.013 | 0.005 | 0.463 | 0.000 |
Abbreviations: IDR, ill-defined rim; PF, pathologic fracture; PR, periosteal reaction; STM, soft tissue mass.
aFisher exact probability test was used. Malignant tumors had a significantly (P = 0.003) lower incidence in PR but a significantly higher incidence in STM than intermediate malignant tumors. No other significant (P > 0.05) difference existed between any other two features.
In two cases with osteosarcoma (Figure 3), one case had osteolytic destruction with a soft tissue mass and tumorous bone, and the other case had mixed bone destruction with ill-defined margins, a soft tissue mass and tumorous bone. In the case of Ewing’s sarcoma (Figure 3), the lesion was osteolytic expansile destruction with ill-defined margins, thinned and discontinued cortex but no soft tissue masses. The aneurysmal bone cyst had eccentric, expansile lytic bone destruction with well-defined margins but no soft tissue masses. The simple bone cyst was expansile lytic bone destruction with well-defined margins. One osteochondroma presented as a bony protrusion like a cauliflower at the distal clavicular end. One case with chondroma at the sternal end had expansile bone destruction with no calcification nor soft tissue swelling.
5. Discussion
5.1. Lesion Nature
In this study, the most frequent lesion is malignant tumors in 50 cases (61.7%) including primarily metastatic tumor, plasma-cell tumor and osteosarcoma accounting for 38.3%, 12.3% and 4.9%, respectively. Fibrous dysplasia and giant cell tumor which are common in other body parts are rare in the clavicle accounting for only 1.2% and 2.5%, respectively, which is probably related to the flat bone of the clavicle. Based on the unpublished data in our hospital over 45 years, the tubular long bones are predominated by benign lesions while most flat and irregular bones like ribs, ilium and sacrum mainly have malignant tumors. The incidence of metastatic tumors and myeloma in the clavicle is similar to that in the ribs, probably in relation to the tissue and anatomical features of the clavicle which is actually a flat bone. All kinds of lesions which tend to occur in flat bones may take place in the clavicle, whereas fibrous dysplasia, giant cell tumors and chondroblastoma which tend to occur in long tubular bones are rare in the clavicle (1-4, 6, 7, 9-12, 14-16). In a study investigating the histopathology, anatomy and epidemiology of bone tumors of the clavicle in 113 patients with a mean age of 40 years (18), 22 benign, 31 intermediate and 60 malignant tumors were found, with eosinophilic granuloma as the most common neoplasm (18.6%), followed by bone metastases (15.0%), plasma cell myeloma (8.8%), Ewing’s sarcoma (8.8%) and osteosarcoma (8.0%). In this study, 53% of the tumors were malignant, with a mean age of 51 years in patients with malignant tumors and 28 years in patients with a benign/ intermediate lesion (P < 0.001).
5.2. Location of Lesions
Distribution of lesions in the clavicle also has specific characteristics. In our study, 50 (61.7%) lesions involved the sternal end of the clavicle, including 38 malignant tumors (76%), which indicates that most of the clavicular lesions occur in the sternal end especially malignant tumors, consistent with the study by Smith et al. (1) This is probably related to the rapid growth and appearance of the epiphysis center only at the sternal end. Because of sparse blood supply to the clavicle (2), metastatic tumors at this site are rare, but in our study, metastatic tumors in the clavicle had the greatest incidence of 38.3%. This is in comparison with other rare diseases in the clavicle because metastatic tumors have a high incidence. Clavicular tumors may easily cause pathological fractures. Traumatic fracture of the clavicle usually occurs in the middle and external segments, and clavicular fracture in the internal segment near the sternal end should raise suspicion of pathological fractures caused by metastatic tumors and plasma-cell myeloma, especially in middle and old citizens. In another study (18), the lateral third of the clavicle was most frequently involved.
5.3. Imaging Presentations
In the anteroposterior radiograph, the external segment of the clavicle does not overlap with other bones and could be displayed clearly; however, the internal segment does overlap with ribs and cannot be clearly displayed even in the oblique radiograph. CT scan is needed for further evaluation of the clavicle.
5.4. Metastatic Tumors
In our study, the metastatic tumors occurred mostly in patients over 50 years of age. The age was older compared to other bone metastases. These tumors mostly had expansile osteolytic destruction with discontinuation of the cortex and soft tissue masses (8). CT displayed lytic bone destruction with ill-defined margins, a soft tissue mass, discontinued cortex and a primary tumor. In some cases with osteosclerotic metastasis, the lesion had apparent osteosclerosis, bone destruction and a lot of periosteal reaction, similar to osteosarcoma (Figure 1).
5.5. Eosinophilic Granuloma
Eosinophilic granuloma is not frequently found in the clavicle; however, it has been described in detail in the literature (4, 7, 12, 15). The lesion most commonly occurs in children less than 10 years, but it also occurs in much older patients (1). The lesion has well defined margins, homogeneous density inside the lesion, apparent periosteal reaction in children and sclerotic rims. The lesion is usually adjacent to normal bone tissue with no soft tissue masses (Figure 2). Combination of the age of onset and imaging features can readily lead to the correct diagnosis in children rather than in adults because of no imaging specificity.
5.6. Plasma-Cell Myeloma
In our study, these patients were mostly more than 50 years and the lesion was lytic expansile bone destruction with ill-defined margins, thinned cortex and concurrent pathological fracture at the sternal end (Figure 2). It is difficult to differentiate it from metastatic tumors. Medullary biopsy and IgM detection in blood or urine may be helpful for diagnosis.
5.7. Osteosarcoma
In our series, patients with osteosarcoma over 20 years of age accounted for 71.4%; while, those over 30 years of age accounted for 57.1% of all osteosarcoma patients, with the age of prevalence greater than for patients with osteosarcoma in long bones (19). Imaging presentations of osteosarcoma are osteolytic destruction with tumorous bone formation and periosteal reaction (Figure 3). Mixed bone destruction can also be shown without periosteal reaction or tumorous bone. A soft tissue mass may be present, similar to the imaging presentations of metastatic tumors with difficulty in differentiation. Clavicular metastatic tumors may have imaging presentations similar to those of osteosarcoma (Figure 1).
5.8. Ewing’s Sarcoma
The prevalence of Ewing’s sarcoma in our study was between 10 and 20 years, consistent with the age of onset for this sarcoma (20, 21). The imaging presentations in one such patient was expansile bone destruction with thinned discontinued cortex, ill-defined margins but no soft tissue masses (Figure 3). These imaging features are not specific for Ewing’s sarcoma and may present difficulty in diagnosis.
In conclusion, many tumors and tumor-like lesions may occur at the clavicle with more malignant than benign tumors with no specific imaging features in most lesions, and a lesion near the sternal end with atypical benign imaging features should be considered as malignant.