1. Introduction
Malignant fibrous histiocytomas (MFH) arise from primitive mesenchymal elements more commonly in males in the 50 - 60-year age group (1, 2). MFH is seen more frequently in the extremities, followed by the abdominal cavity and the retroperitoneum (3). The iliopsoas compartment is a rare site for soft tissue sarcomas as well as other primary and secondary tumors (4). We hereby report a case of cystic malignant fibrous histiocytoma that was clinically and radiologically misdiagnosed as a psoas cold abscess.
2. Case Presentation
A 60-year-old male presented with gradually progressive history of lower abdominal pain associated with an intermittent fever for the past 6 months. Past medical history included presence of skeletal tuberculosis involving the ribs. Physical examination of the abdomen revealed no focal signs. Blood investigations revealed an elevated ESR and total leukocyte count with an increased lymphocyte count. Three sputum samples were positive for acid fast bacilli. On this basis, further treatment plan included category-two protocol of antituberculous antibiotic therapy including a three-month intensive phase of isoniazid (H), rifampicin (R), pyrazinamide (Z), ethambutol (E); two months of streptomycin (S); and five months continuation phase of HRE.
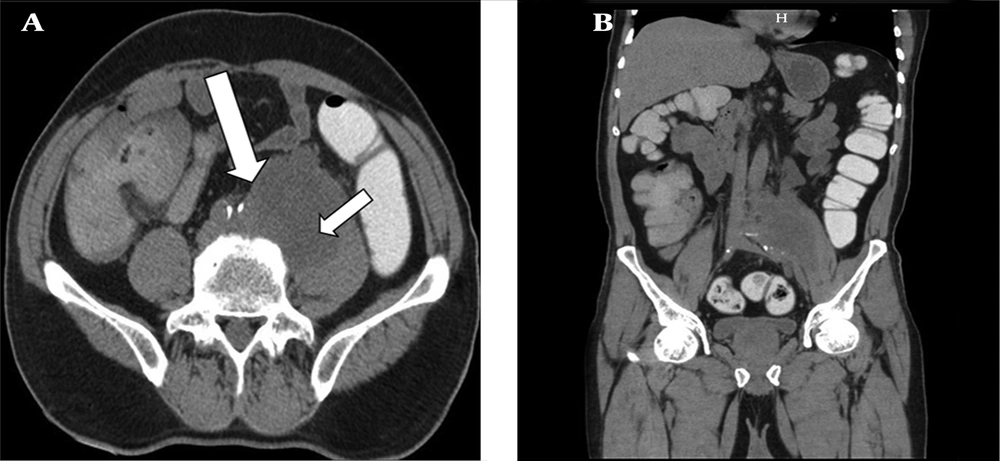
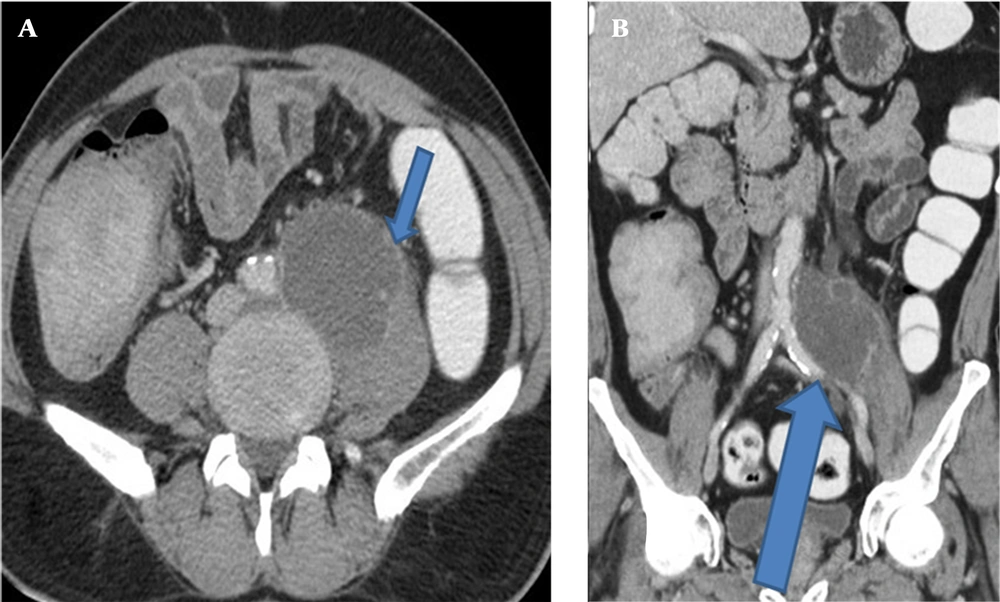
Gray scale ultrasound (US) of the abdomen revealed a large well-defined multilocular lesion with internal anechoic areas along the left psoas muscle. The US did not delineate the exact extent of the lesion. On Doppler study, the lesion showed no evidence of internal flow. The patient was further evaluated using cross-sectional imaging. A baseline nonenhanced computed tomography (NECT) scan followed by a contrast enhanced computed tomography (CECT) scan was acquired using a 16 slice scanner (General Electric Brightspeed, Milwaukee, Wisconsin, USA) by injecting 120 mL of intravenous contrast iohexol (Omnipaque, General Electric Healthcare) through an eighteen gauge needle in the right antecubital vein at the rate of 3 mL/sec. The scanning parameters used were a tube current of 105 milliampere seconds (mAs), and a tube voltage of 130 peak kilovoltage (kVp). Acquisition was performed at the slice thickness of 5 mm. Image acquisition was done during the venous phase (70 - 90 sec). The 5-mm-thick axial images were reformatted into thinner sections in three orthogonal planes (0.6 mm thick). On NECT, a large well-defined smoothly marginated multi loculated lesion of fluid attenuation (average HU 15 - 20) was noted in the left retroperitoneum involving the left psoas muscle (Figure 1). The lesion was 5.8 × 6.5 × 8.4 cm in size (AP × ML × CC). On CECT images, the lesion showed a peripherally thin, continuous rim enhancement in continuity with the left psoas muscle margin. The lesion caused inferomedial displacement of the left common iliac vessels; however, no evidence of invasion of adjacent retroperitoneal structures (including vessels) was noted (Figure 2). No evidence of vertebral erosion was noted.
A 60-year-old man with gradually progressive lower abdominal pain and intermittent fever for 6 months diagnosed as retroperitoneal cystic malignant fibrous histiocytoma. Non-enhanced computed tomography in axial (A) and coronal (B) views show a large well-defined smoothly marginated multi-loculated cystic lesion in the left retroperitoneum along the left psoas muscle (large arrow) with internal fluid attenuation areas (small arrow).
Contrast enhanced computed tomography in the same patient. A, axial and B, coronal images. The lesion shows peripheral thin continuous rim enhancement that is continuous with the left psoas muscle margin (small arrow in image A). The lesion has caused inferomedial displacement of the left common iliac vessels but no invasion of adjacent retroperitoneal structures, or vessels is noted (large arrow in image B).
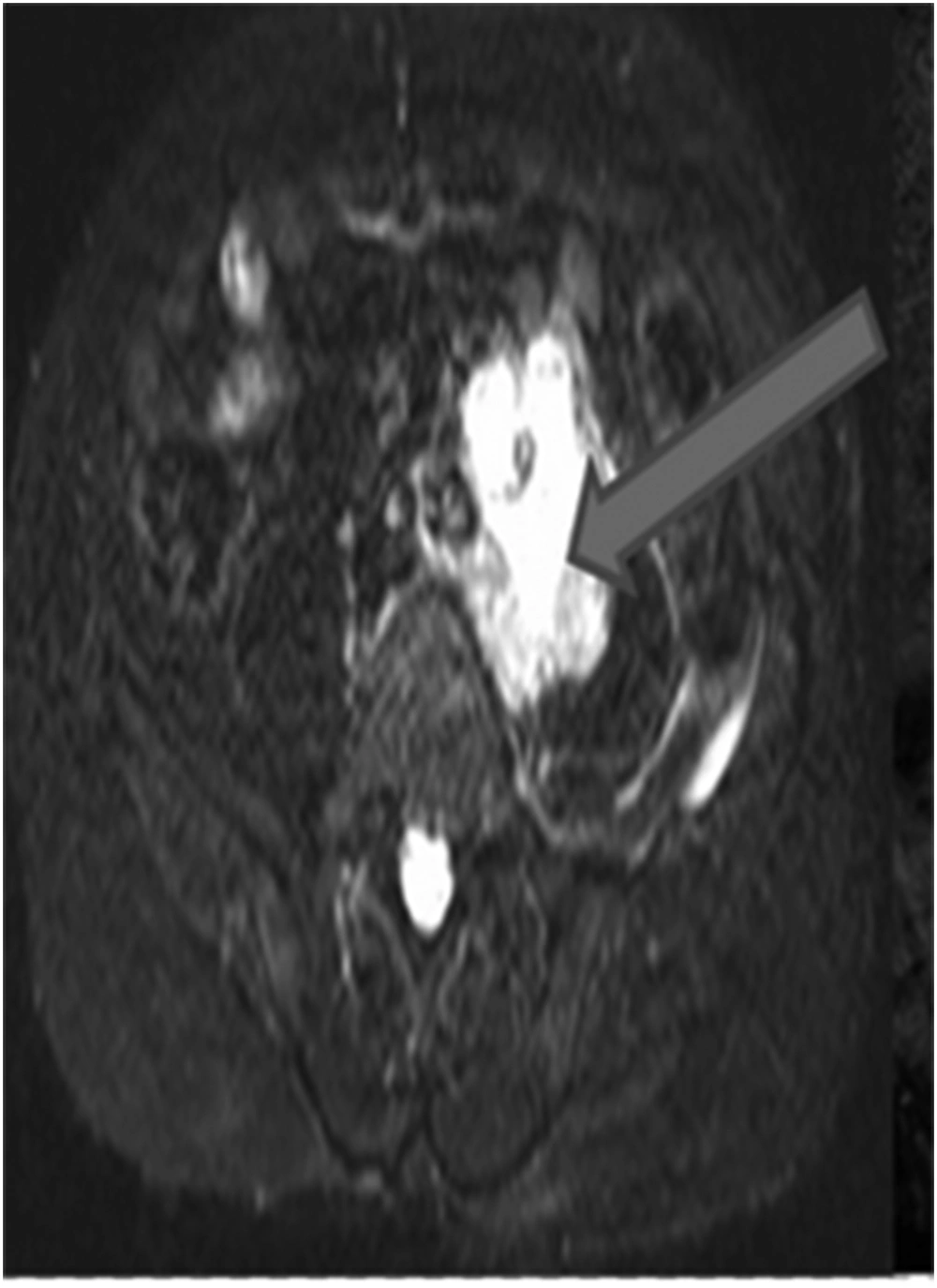
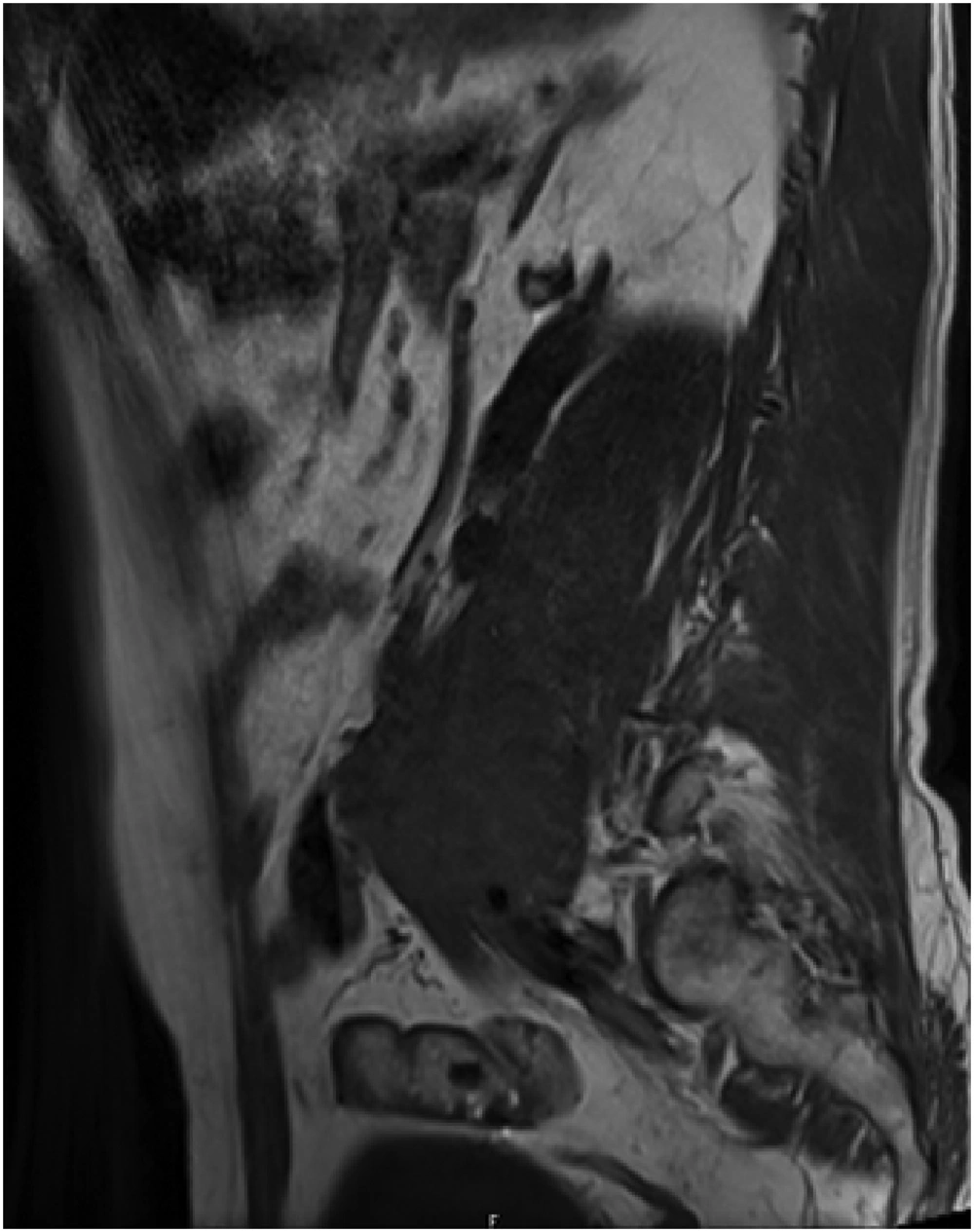
Magnetic resonance imaging (MRI) was performed with a 1.5 Tesla 8 channel scanner (Siemens Magnetom Essenza, Erlangen, Germany). A dedicated phased-array body coil was used. Non-enhanced MRI demonstrated a well-defined lesion with fluid signal intensity on short tau inversion recovery (STIR) images [TR 3750 ms, TE 30 ms, slice thickness 3 - 5 mm] (Figure 3) and hypointense signal lesion on T1 weighted images [TR 119 ms, TE 4.8 ms, slice thickness 5 mm] in the psoas muscle (Figure 4). No evidence of spinal canal extension was noted. No evidence of focal vertebral marrow lesions was noted.
Based on combined clinical history, laboratory investigations and imaging findings, a benign infective lesion such as psoas cold abscess was considered as the diagnosis.
Ultrasound guided needle aspiration of the lesion revealed blood stained turbid fluid with debris. Laparoscopic debridement of the lesion was done and the specimen was sent for histopathological examination.
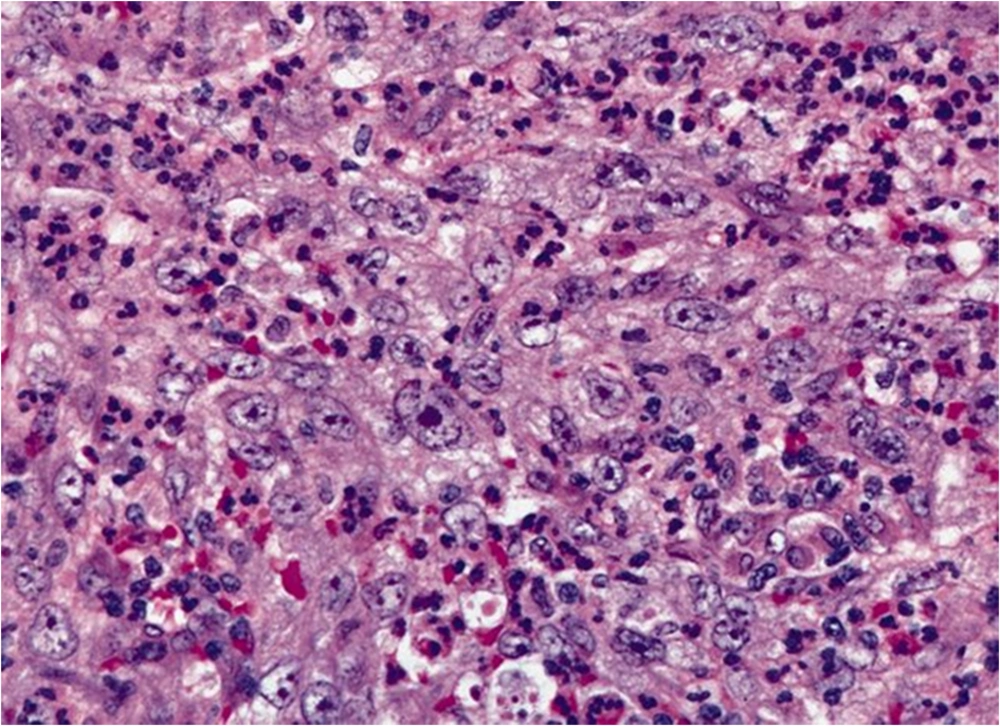
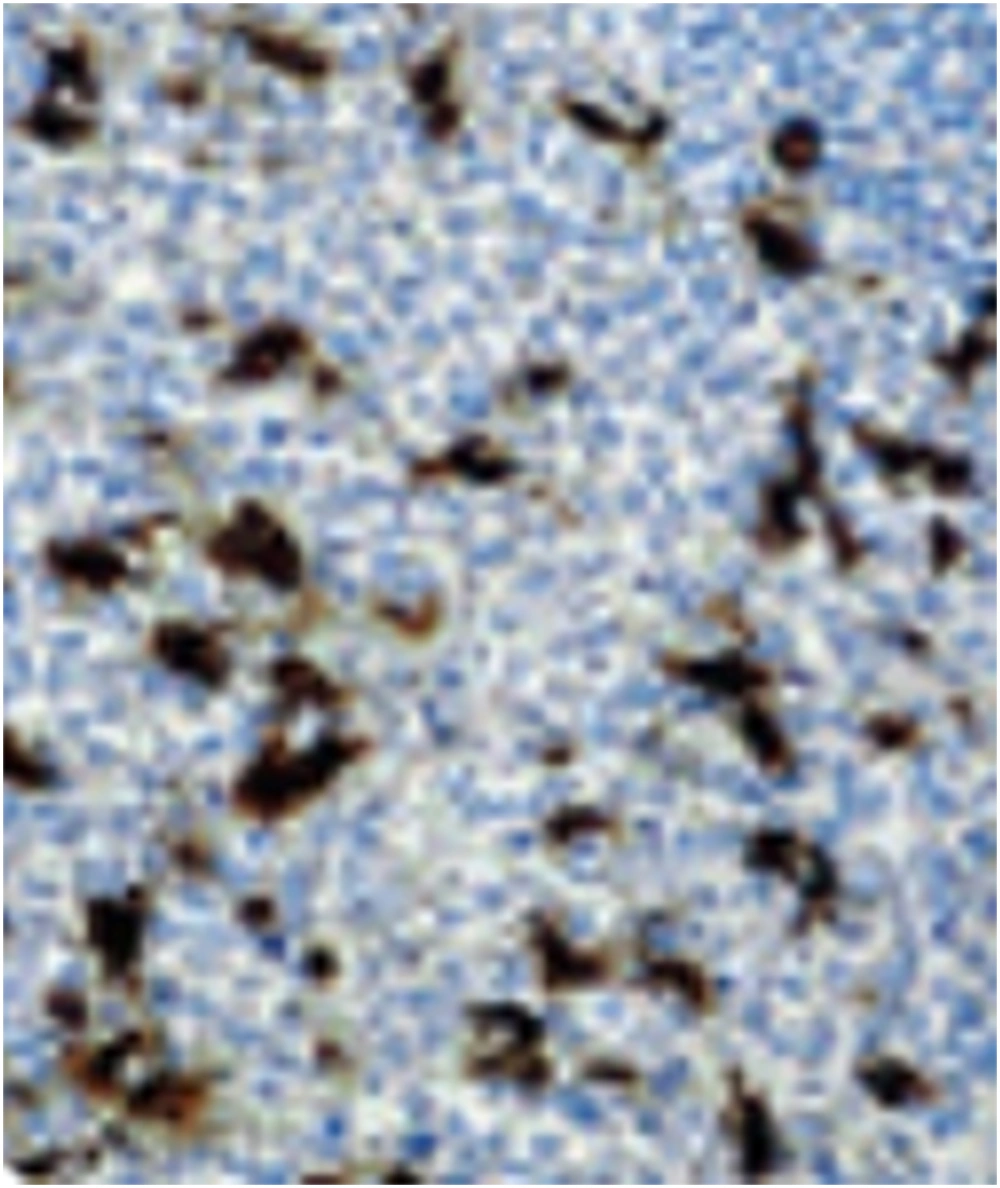
Histopathological examination showed spindle cells and fibroblast-like cells arranged in short fascicles and loosely arranged whorls in storiform pattern (Figure 5). Histiocytes with an increased nucleus-cytoplasm ratio and prominent nucleoli were noted. On immunohistochemical examination, the tumor cells showed positivity for CD68, lysozyme and negative staining for S-100, and smooth muscle antigen (SMA) (Figure 6). The patient was treated with adjuvant chemo-radiotherapy and is currently doing well. No cross sectional imaging follow-up has been performed for the patient yet.
3. Discussion
Inflammatory MFH is a rare subtype of MFH that can clinically mimic an abscess. It is characterized by intense acute inflammatory reaction in the absence of a known infection, and commonly affects the retroperitoneum. These patients frequently present with constitutional symptoms including fever, malaise, weight loss and anorexia in addition to local abdominal discomfort and elevated serum C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR). Inflammatory MFH typically shows hypervascularity on the arterial phase of CECT scan with an early wash-out on the venous phase (3).
MFH may appear as hypoechoic, of mixed echogenicity or predominantly anechoic with thick septa on ultrasound (US). On CT, MFH typically presents as a large poorly-marginated infiltrative soft tissue mass with a density similar to normal muscle, often with hypodense areas due to internal necrosis. Eccentrically located lumpy and ring-like calcifications have been reported on CT. MFH with extensive necrosis can rarely present as a benign cystic tumor or abscess. Five percent of MFH cases may demonstrate extensive hemorrhage associated with cyst-like space that may be confused with hematoma. Post contrast images may show a heterogeneously enhancing soft-tissue mass with areas of necrosis and invasion of adjacent organs with kidney being most commonly involved. Despite all the above features, most common imaging findings are mostly nonspecific (1, 2, 5).
Magnetic resonance imaging features favoring MFH over abscess include heterogeneous signal on T2-weighted images, and invasion into adjacent soft tissue plane however, definitive diagnosis can be made only by multiple site biopsy (3). The differential diagnosis for retroperitoneal cystic MFH includes leiomyosarcoma (cystic areas more common), abscess and hematoma formation in the order of importance (1, 5).
MFH is characterized microscopically by areas of spindle cells arranged in a storiform pattern, and pleomorphic areas with haphazardly arranged sheets of fibroblasts and histiocytes. On the basis of the pathologic findings, MFH can be classified into five types depending on the distribution of these cells: the storiform-pleomorphic type (most common type), the myxoid type, the giant cell type, the inflammatory cell type, and the angiomatoid type. The prognostic factors that predict local recurrence and distant metastasis include the histological grade of the mass and the status of the resected tumor margin (most reliable predictor), patient’s age, history of recurrence, the tumor size, and depth of invasion (5, 6).
Wide surgical excision with tumor-free margins remains the principal treatment modality with concurrent chemotherapy and radiation therapy that are needed to reduce the possibility of local recurrence and metastases (3, 6). MFH with extensive necrosis has been reported to mimic a benign cystic tumor or abscess (7).
Retroperitoneal cystic MFHs are difficult to distinguish on imaging from more common lesions such as psoas abscess, conglomerated tubercular necrotic lymph node mass, cystic schwannoma, and retroperitoneal abscess because radiologic findings are usually nonspecific. Despite the varied imaging findings of MFH, it should be considered as a differential diagnosis in a patient with retroperitoneal cystic mass in the psoas muscle especially in regions where tuberculosis is endemic.