1. Background
Pulmonary valve stenosis (PS) accounts for 10% of congenital heart diseases and is accompanied in approximately 20% of congenital heart disease cases (1). PS seldom presents with exercise intolerance, but frequently presents with an asymptomatic systolic murmur. Mild PS goes unnoticed for many years and has no negative symptoms, while severe PS could progress to significant stenosis and secondary hypertrophy in the infundibulum (2). Therefore, it is an urgent issue to develop an effective method for timely diagnosis of PS.
As multislice spiral computed tomography is widely applied in cardiovascular imaging, increasing attention has been paid on significance of computed tomography in the evaluation of heart valve (3, 4). Since Nie et al., Johnson et al., Flohr et al. and Li et al. initially applied dual-source CT (DSCT) for cardiac imaging; DSCT has been widely available in preoperative evaluation of patients with congenital heart disease, which can detect cardiac lesions in the right ventricle, right ventricular outflow tract, and pulmonary artery development (5-8). Therefore, current imaging examinations are capable of determining the number and shape of pulmonary valves exactly in most of affected patients stably and efficiently and some investigations on the DSCT system have been performed on other adult heart diseases (9-13). However, DSCT evaluation of pulmonary valve in children with congenital heart disease remained to be further investigated.
2. Objectives
The present study aimed to explore the significance of dual-source computed tomography (DSCT) in the evaluation of PS in children with congenital heart disease and to establish a score system for PS evaluation in children.
3. Patients and Methods
3.1. Patients
A total of 98 children with congenital heart disease were included in this study from October 2013 to March 2015. There were 46 boys and 52 girls and their age ranged from 3 months to 14 years (mean age was 1.7 ± 0.9 years). Among these patients, 78 cases (79.6%) had tetralogy of Fallot, 7 cases (7.1%) double outlet right ventricle, 6 cases (6.1%) trilogy of Fallot, 4 cases (4.1%) transposition of the great arteries and 3 cases (3.1%) corrected transposition of the great arteries.
3.2. Equipment and Method
Under a calm breathing state, all enrolled children were scanned by Somatom definition DSCT scanner (Siemens, Forchheim, Germany) using a dual-syringe power injector (Stellant D, Medrad, Indianola, PA). The scanning was performed in cardiac-DS-children-heart-ECG pattern and the orientation was from the head to feet. The scanning performed from the thoracic entrance to 5 mm subphrenic. Tube voltage (80 - 100 kv) and tube current (50 - 180 mAs) were individually adjusted according to their age and weight (14). Iopromide was injected to each child (370 mg/mL, 1.0 - 2.5 mL/kg) at the speed of 0.5 - 2.5 mL/s via two-tube high pressure syringe (Medrad, The USA), and then normal saline (2 - 20 mL) at the same flow rate. For setting DSCT, the main pulmonary artery was set as the region of interest and scanning was triggered with the bolus-tracking method at the threshold of 70 Hounsfield unit (HU) with 6 seconds delay.
3.3. Image Post-processing
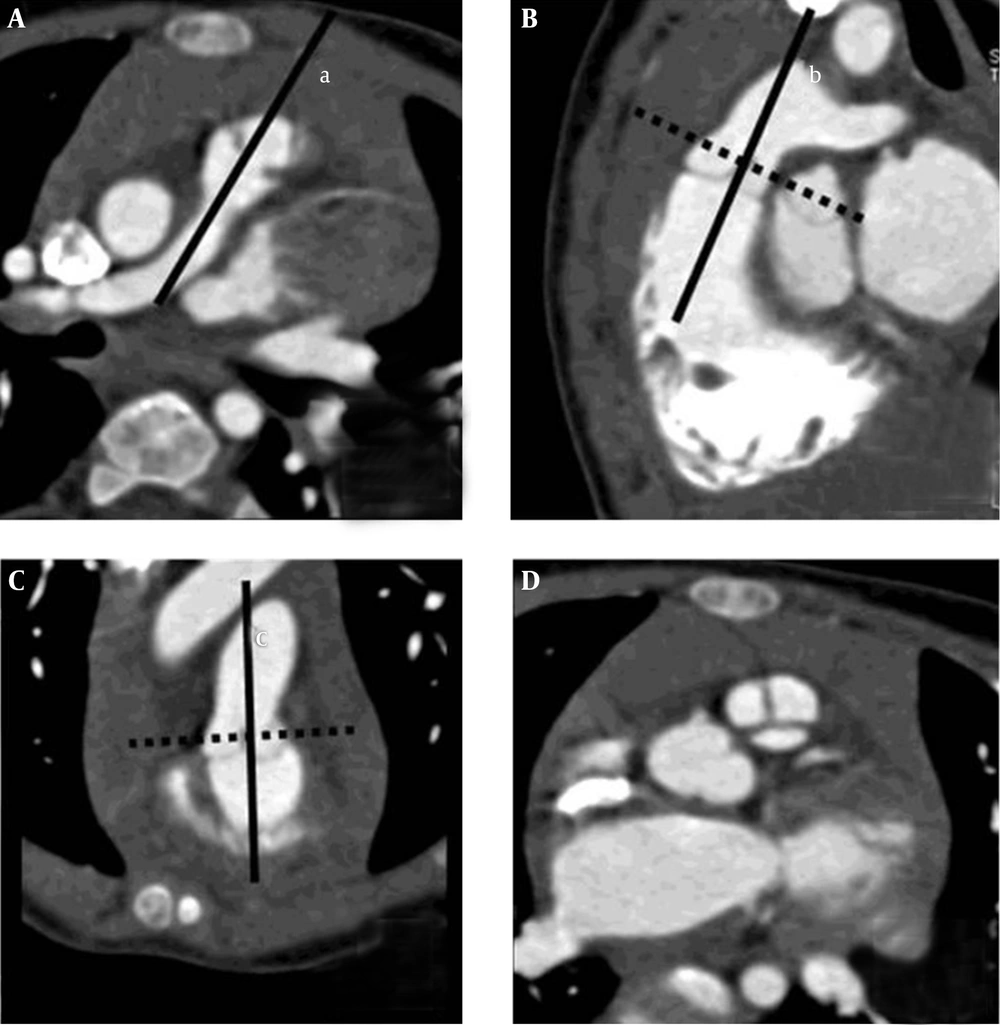
After scanning, the optimal diastolic and systolic images were automatically reconstructed and then uploaded to the Syngo workstation (Siemens healthcare, Erlangen, Germany) (15). The pulmonary valve was illustrated at three-dimensional interface through double-oblique multiplanar reformation (MPR) (Figure 1).
Pulmonary Valve Illustrated Through Double-Oblique Multiplanar Reformation; A, The marker line (full line a, referring to sagittal plane) was adjusted to be parallel to the long axis of main pulmonary artery at the transverse section, obtaining oblique sagittal image; B, the marker line (full line b, referring to coronal plane) on the oblique sagittal image was adjusted to be parallel to pulmonary artery root at a tangent position, obtaining oblique coronal image; C, the marker line (full line c, referring to sagittal plane) on the oblique coronal image was adjusted to be parallel to pulmonary artery root at a tangent position; D, the position and angle of transverse section marker line (dashed line) at the pulmonary artery root as shown in B and C were adjusted to be perpendicular to full line b and c, obtaining full view of pulmonary valve at oblique transverse section (a 10-month-old boy with mild tetralogy of Fallot showed three pulmonary valves and valve leaflet was thickened).
3.4. Image Evaluation
Two experienced radiologists independently assessed the image quality of pulmonary artery valves. If they got consistent results, the score was confirmed, while if disagreement occurred, the score was confirmed after discussion. When pulmonary artery valve is closed at diastolic stage, the valve closure line is clearly recognized and the number and shape of pulmonary valves could be analyzed (16). When pulmonary artery valve is open at systolic stage, the opening state of pulmonary valves can be observed (17).
Considering real-time three-dimensional echocardiography findings of pulmonary valve as the evaluation standard (18), image quality of transverse section and MPR image at diastolic stage was assessed ranging from 1 to 4 points; 4 points, valve leaflets are clearly visible at the transverse image and the number of valve leaflets is detectable by MPR image; 3 points, valve leaflets are fuzzy at the transverse image and the number of valve leaflets is detectable by MPR image; 2 points, valve leaflets are fuzzy at the transverse image and the number of valve leaflets is not detectable by MPR image; 1 point, pulmonary artery valve is not visible. A score of ≤ 2 points is excluded for the diagnosis.
In accordance with the pediatric age, involved patients were divided into four age groups: 0 - 1 year group, 1 - 3 year group, 3 - 7 year group and 7 - 14 year group (9). According to heart rate, participants were divided into three groups: < 90 beats per minute (bpm) group, 90 - 110 bpm group and > 110 bpm group.
3.5. Statistical Analysis
Statistical analysis was performed by SPSS ver. 13.0 software (SPSS Inc., Chicago, Ill, USA). The consistency of image quality assessment was checked by Kappa test. One-way analysis of variance was applied to detect the score difference between different heart rate groups and age groups. The differences between groups were compared using student-newman-keuls (SNK) test. Partial correlation analysis was used to test the effects of age and heart rate on image scores. P < 0.05 was considered as significant difference.
4. Results
4.1. Preliminary Evaluation of Image Quality
The image quality scores evaluated by the two radiologists were consistent (Kappa = 0.77). The average image quality score of 98 patients with congenital heart disease was 2.92 ± 0.85 points and the scores of 73.4% (72/98) cases were more than 3 points, which can be applied for further diagnosis.
4.2. Image Quality of DSCT Evaluation in Different Age Groups or Different Heart Rate Groups
As Table 1 shows, different scores were achieved by four age groups (F = 12.91, P < 0.001). There was a statistically difference (P < 0.05) between the four groups except 0 - 1 group and 1 - 3 group, 3 - 7 group and 7 - 14 group, and the image quality of elder group was higher than younger group.
| Age, y | Number | Score (Points) | ≥ 3 Points, % |
|---|---|---|---|
| 0 - 1 | 27 | 2.41 ± 0.89A | 15 (55.5) |
| 1 - 3 | 31 | 2.68 ± 0.70A | 20 (64.5) |
| 3 - 7 | 22 | 3.41 ± 0.59B | 20 (90.9) |
| 7 - 14 | 18 | 3.50 ± 0.62B | 17 (94.4) |
aMean values in 0 - 1 and 1 - 3 (A) are significantly different with 3 – 7 and 7 – 14 (B) age groups.
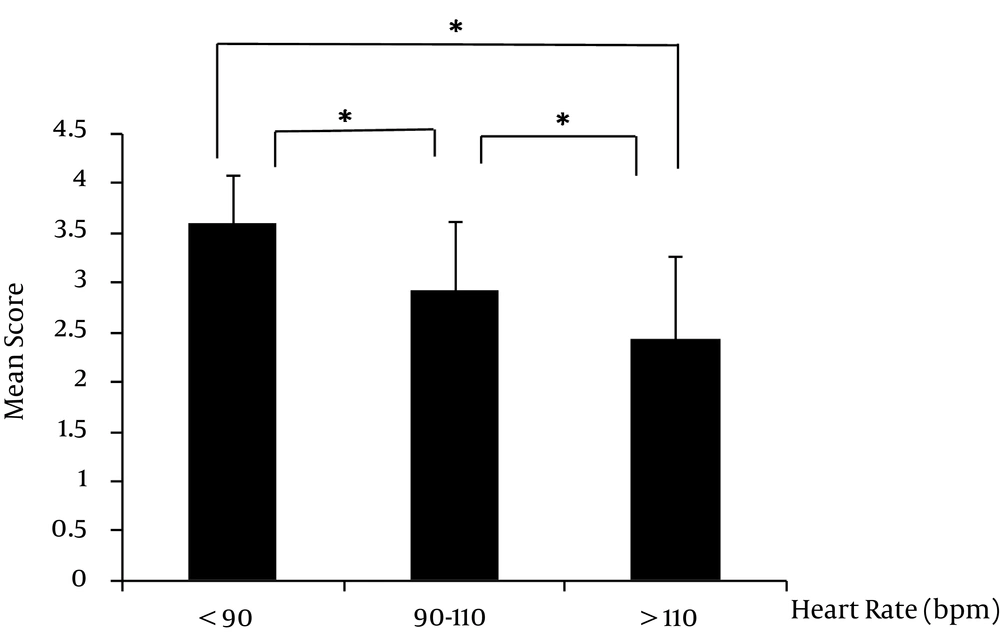
The image quality scores were different (Figure 2) between the three heart rate groups (F = 19.05, P < 0.001). There were significant differences in the scores between the groups (P < 0.05).
Correlation analysis results showed that the correlation coefficient was 0.185 (P = 0.070) for the effect of age on image score; the correlation coefficient was -0.391 (P < 0.001) for the effect of heart rate on image score; the correlation coefficient was -0.464 (P < 0.001) for the correlation between age and heart rate.
4.3. Evaluation of Leaf Number and Morphology in Diastole Phase by DSCT
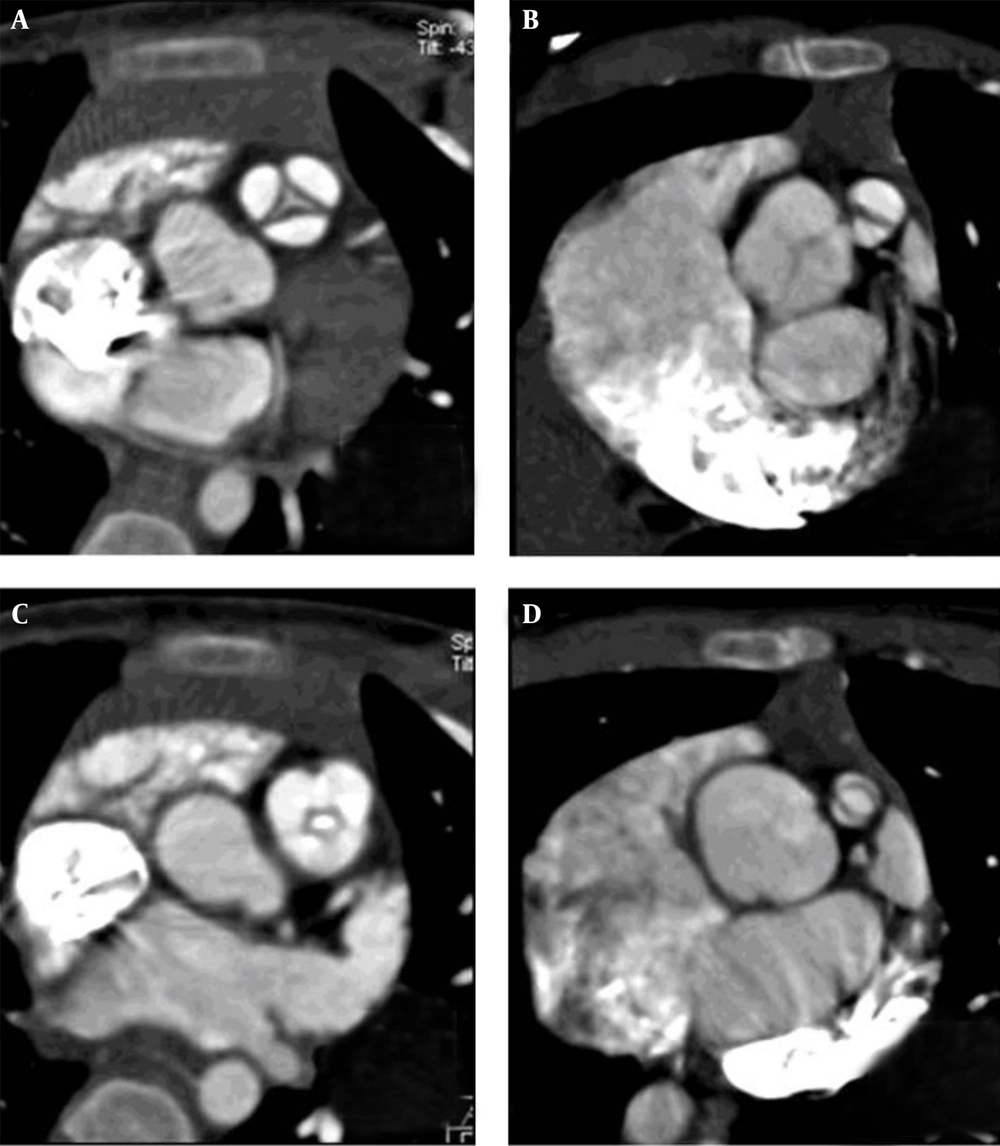
DSCT showed that 37 cases had tricuspid pulmonary valve and 35 cases bicuspid pulmonary valve. In 37 cases with tricuspid pulmonary valve, their closure line was Y-shaped, among which 28 cases had thickened leaflets, even irregular valve shape (Figure 3 A). In 35 cases with bicuspid pulmonary valve, their closure line was single, showing “—” shape in 17 cases, “|” shape in 11 cases and “/” or “” shape in 7 cases (Figure 3 B), among which 32 developed valve thickening. These results from DSCT were 100% consistent with those from the operation.
Evaluation of Valve and Valve Orifice Morphology; A, a 17-month-old boy with trilogy of Fallot, image quality score was 4 points, showing thickened valves in pulmonary artery and the valves were thickened; B, a 2-year-old girl with tetralogy of Fallot, image quality score was 4 points, showing bicuspid valve malformation in pulmonary artery and thickened valve, valve closure line at diastolic stage was “” shaped, valve annulus dysplasia was found; C, the same child shown in A, pulmonary artery valve opening was restricted at systolic stage, valve orifice was shaped as “fish mouth”; D, the same child shown in B, pulmonary artery valve opening was restricted at systolic stage.
4.4. Evaluation of Opening Status of Pulmonary Valve in Systole Phase by DSCT
Among these 98 children, only 23 cases (23.5%) could meet the evaluation condition in systole phase, among which 11 cases had tricuspid valves and 12 cases bicuspid valves. All tricuspid valve cases and 10 bicuspid valve cases had different degrees of opening limitation (Figure 3 C and D), showing cupola sign in long axis and “fish mouth” shape in short axis. The remaining two cases with bicuspid valve had no adhesion, of which valve leaflets opened parallel with severe hypoplasia in valve annulus. These results from DSCT were 100% consistent with those from the operation.
5. Discussion
Preoperative determination of PS severity, valve leaflet and valve annulus dysplasia, position of value junction and supravalvular or subaortic stenosis would play a crucial role in the surgical plan of PS (19, 20). There are three semilunar valves in normal pulmonary artery valve cases. Adhesion or fusion at the valve junction may lead to restriction of valve opening and valve orifice stenosis, consequently resulting in a series of morphological changes in the right ventricle and pulmonary artery. In addition, abnormalities in the number of pulmonary artery valve or dysplasia trigger PS (21). Congenital heart disease is often associated with bicuspid valve malformation, valves and valve annulus dysplasia, as well as fusion at the valve junction (22).
Several technologies have been used for PS: 1) transthoracic echocardiography only showed pulmonary artery longitudinal section and simultaneously displayed two pulmonary valve leaflets due to acoustic window. As a result, it fails to recognize the number of valve leaflets accurately and the full view of pulmonary valves can be observed in a minority of valve annulus transverse sections (23, 24); 2) Real-time three-dimensional echocardiography can determine the number of pulmonary valves in a half of PS patients through reconstruction of volume data acquired (25). However, this technique has some shortcomings, such as low display rate, poor spatial resolution, heavily depending on techniques and other several interference factors; 3) hemodynamic change, explicit PS location and severity of PS cases, can be detected by right ventricular angiography, but it cannot directly display the number and morphology of stenotic pulmonary valve. Though angiography findings are indicative evidence of the final diagnosis, it is invasive and has potential risks (26); 4) MRI is capable of displaying cardiac valve for further qualitative and quantitative evaluations, but it shows low spatial resolution, long-term detection, and large noise; moreover, it is not available for patients such as cardiac pacemaker; 5) multislice CT (MSCT) allows obtaining anatomical images of cardiac valve for further detecting valve movement through multiple phase reconstruction; its ionizing radiation makes it a supplementary examination for pulmonary valve disease (27). For patients with congenital heart disease, especially with tetralogy of Fallot, pulmonary valve imaging based on the volume data is beneficial for evaluation of cardiac structure.
Double-oblique MPR is characterized as simple operation and good reproducibility. It accurately obtains short axis section images of the pulmonary artery root and clearly displays the number and morphology of pulmonary valve (28). In this study, DSCT clearly displayed the pulmonary valve in children older than 3 years or heart rate below 90 bpm. Partial correlation analysis showed a significantly reverse correlation between heart rate and image quality scores, indicating that lowering heart rate can significantly improve the image quality. Although temporal resolution of DSCT reached 84 ms, it cannot satisfy children with high heart rate. Artifacts produced by pulmonary valve during heartbeat cannot be avoided, which considered to be the possibly effect of the image quality. Furthermore, age was positively correlated with the scores, but it was not significant, indicating that the image quality cannot be obviously improved along with age. The difference between different age groups can be explained by negative correlation between age and heart rate. When the child grows up, his or her heart rate decreases so the image quality improves. Therefore, careful consideration should be paid on application of DSCT in evaluation of pulmonary valve in children at a higher heart rate and the image quality can be improved by controlling heart rate (29).
In this study, 73.4% of children reached the image quality standard (> 3 points) for evaluation of pulmonary valve. The number of valve observed by DSCT was 100% consistent with that observed in the operation. In addition, DSCT accurately displayed the shape and location of pulmonary valve closure line and the valve size and detected valve thickening or calcification, which helps formulate treatment scheme and surgical approach. We explored the opening status of pulmonary valve at systolic stage and the results from DSCT were consistent with surgical findings (30). Unfortunately, image quality in only 23.5% of cases reached the evaluation standard (> 3 points) at systolic stage and further study is needed to analyze influencing factors.
In summary, DSCT can accurately evaluate the opening status of pulmonary valve and has potential application value. However, the image quality is affected by heart rate. Therefore, it is important to make an improvement on CT and effect of heat rate would be avoided through improvement of CT temporal resolution.