1. Background
Globally, cardiovascular diseases (CVDs) are the leading cause of premature death (1)). It is predicted that CVD-related mortality will increase to 23 million by 2030 (about 30.5% of all deaths) (2, 3). Out-of-hospital sudden cardiac arrest (OHCA) accounts for more than 60% of deaths caused by CVDs (4). In the United States, its prevalence is 300,000 events per year (5). Hence it has a substantial impact on mortality (> 90%) (6).
Bystander CPR performance has a significant effect on the survival rate (especially neurologically intact survival) from OHCA (7). Besides, it has been shown that bystander CPR increases the survival rate of OHCA by two to three-folds (8, 9); however, it is performed in 30% - 50% of the cases (10) due to a hesitation regarding the resuscitation in the lay rescuers (11). In addition to the CPR, the quality of the procedure defined as adequate compression depth and rate, complete chest recoil, minimized interruption, and avoidance of excessive ventilation are crucial factors in determining the survival of victims (12). Furthermore, from the military perspective, soldiers’ proficiency in performing first aid procedures help them to save more lives in the case of medical assistance for natural disasters, as well as to improve combat power in the battlefield (13).
Many methods have been introduced to improve the acquisition and retention of CPR-related knowledge learned in courses. The lecture-based teaching method is one of the most common and precedent ways of teaching CPR (14). Although this method has been integrated into the medical science curriculum, it may not be the best approach for teaching practical skills (Kumar 2015 of 10). Many other novel approaches have been introduced to improve the quality of learning. Video-assisted instruction (15, 16), simulation, multimedia learning, a combination of self-directed learning and instructor-led teaching with hands-on training (17, 18), and case-based instruction (19) are among the alternatives to traditional teaching methods. Many new devices, including CPR feedback-prompt devices, have been shown to improve the quality of CPR skills (20). Studies have also shown that the addition of a simultaneous hands-only practice to the video-only course would improve the performance of CPR (21) and enhance the retention of acquired CPR skills (15).
To the best of our knowledge, no study has compared the efficiency of different techniques of teaching CPR skills to the soldiers in the military training program.
2. Objectives
The current study aimed to compare three different methods of teaching CPR in terms of primary acquisition and retention of CPR skills in soldiers.
3. Method
3.1. Research Design
This study was performed from November 2019 to February 2020 on selected duty male soldiers doing their military service (in Iran military service is obligatory for males). The goal of this randomized controlled trial was to compare the effect of three instructional methods on the acquisition and retention of CPR skills in the soldiers. Sample size was estimated to be 13 in each group (effect size of 0.2, α = 0.05, and β = 0.8). The research protocols were approved by the local Ethics Committee. Written informed consent was obtained from participants. Literate duty soldiers aged 20 - 30 years with a primary CPR test score of below 10 were included in the study. Soldiers who had a history of attending a CPR-related course or were graduated from medical schools were excluded. All participants were randomized into 1 of the following 4 groups:
1) A lecture-based, 30-minute class session followed by a one-hour practice on a manikin;
2) A 20-minute instructional video followed by a one-hour practice on a manikin;
3) A 20-minute instructional video without practice on a manikin (video only);
4)No intervention.
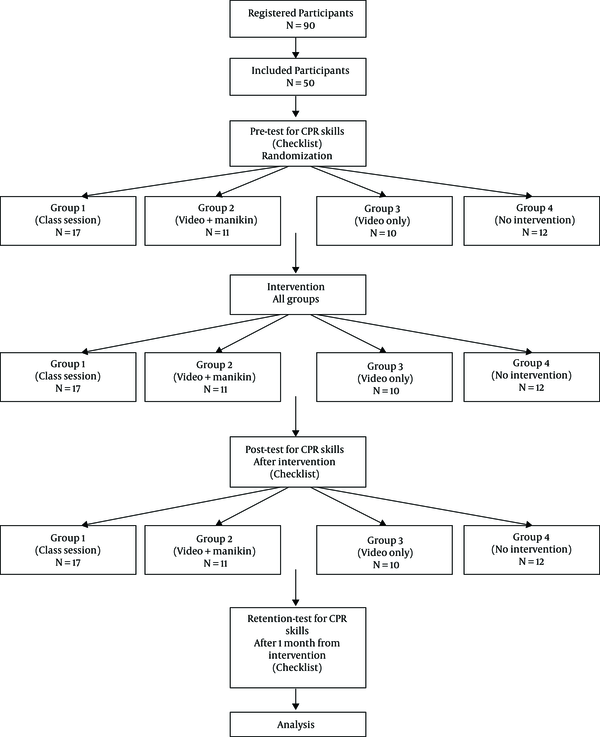
A research assistant supervised the implementation of pre- and post-tests to be according to the research protocols. A Retention test was performed one month after the initial post-test. The study randomization flow diagram is illustrated in Figure 1.
3.2. Selection of the Participants
An announcement was issued in one the army campus about the research to enforce soldiers to participate. Ninety soldiers registered to participate, and after applying the inclusion and exclusion criteria, 50 were included.
3.3. Intervention
Before initiating the study, all participating soldiers attended a meeting with the researcher. All protocols were explained, and informed written consent was obtained from them. They were randomized into 4 groups according to the mean random numbers generated by the computer. The participants were blinded to the intervention until the day of instruction. However, the researcher was not blinded to the intervention. All groups had their instruction courses, which were held simultaneously in the same classroom.
Members of group 1 were assigned to the traditional method. It included a 30-minute face-to-face lecture-based class followed by a one-hour manikin practice. All soldiers practiced CPR skills on the manikin with one-on-one feedback from the facilitator.
Members of group 2 watched a 20-minute instructional video followed by one-hour manikin practice without any feedback from the facilitator. This video was in the native Persian language and had all the criteria of AHA guidelines. All participants watched the video individually on a computer with earphones.
Group 3 was subjected to a 20-minute instructional video (video only) without any further practice. Group 4 also received no intervention and was subjected to the limited courses provided by the army during the educational period before the initiation of the military service.
The manikin used in this study was an IM13-S Brayden CPR manikin without illumination.
3.4. Method of Assessment
A pre-test was used to assure that all participants are deficient in CPR skills. A scenario of an OHCA was presented to the participants and they were asked to perform the appropriate interventions on the manikin. Their performance was videotaped and analyzed by two referees experienced in CPR. The referees rated the soldiers independently, and in cases of disagreement about the scores, they watched the video again together and agreed on a single score. The referees were blinded to the intervention type of each soldier. Soldiers’ performance was assessed using an observational sheet based on the updated American Heart Association CPR guidelines (22, 23). This checklist consists of 17 CPR items rated in three levels: “done correctly and completely” was rated as 2, “done but not completely or not accurately” as 1, and “not done” as 0. The interobserver reliability of the checklist was acceptable (interclass correlation coefficient of 0.9) (23). The referees rated the participants’ performance based on being consistent with the updated CPR guideline. The total score ranged from 0 to 34. We divided the total score into two subcategories, including “Preparation score” for the CPR (first 4 items) and “ABC score” (the remaining 13 items). The checklist is provided in Appendix 1 in Supplementary File.
After complete provision of the instructions, all groups were assessed separately in 4 consecutive days with a similar method as the pre-test. All soldiers were called for a retention test one month after the initial instruction session and were assessed with a similar method as a follow-up.
We used another self-made questionnaire to collect demographic data. Data on age, education level, marriage status, history of CVD, family history of CVD, living with a high-risk person for the cardiac attack, history of facing an OHCA victim, and history of observing a CPR were also collected.
3.5. Statistical Analysis
The distribution of test scores in each study group is reported by the median (interquartile range) at the baseline. We used a mixed-effect model analysis using random intercept and restricted maximum likelihood variance estimator to test the effect of each intervention compared to the control group on test score changes relative to the baseline. In each model, the interaction of group and time (before the intervention, after, and one month later) was used to assess the effect of intervention compared to the control. Post-hoc marginal tests were used to calculate the mean (SEM) of test scores in each group and time point as well as to calculate the P value for pairwise comparison of each intervention and control. All analyses were performed in Stata version 16.0 (StataCorp., College Station, TX).
4. Results
4.1. Baseline Characteristics
In total 50 male participants with a mean age of 22.44 ± 2.08 years (ranged 20 - 27) were investigated. There was no difference concerning the baseline characteristics of the participants (Table 1). Most of the participants were married and did not have experience in CPR observation.
| Characteristics | Group 1 (N = 17) | Group 2 (N = 11) | Group 3 (N = 10) | Group 4 (N = 12) | P Value |
|---|---|---|---|---|---|
| Age | 23.12 ± 2.26 | 21.73 ± 1.73 | 22.40 ± 2.37 | 22.17 ± 1.80 | 0.356 |
| Education | 0.594 | ||||
| Diploma | 8 (47.1) | 8 (72.7) | 5 (50) | 7 (58.3) | |
| University degree | 9 (52.9) | 3 (27.3) | 5 (50) | 5 (41.7) | |
| Marital status | 1.000 | ||||
| Single | 13 (76.5) | 9 (81.8) | 8 (80) | 10 (83.3) | |
| Married | 4 (23.5) | 2 (18.2) | 2 (20) | 2 (16.7) | |
| Positive self or family history of CVD | 2 (11.8) | 1 (9.1) | 1 (10) | 0 (0) | 0.754 |
| Living with a high-risk person for cardiac attack (yes) | 2 (11.8) | 0 (0) | 1 (10) | 0 (0) | 0.526 |
| Positive history of observing a CPR | 1 (5.9) | 0 (0) | 2 (20) | 0 (0) | 0.285 |
| Positive history of facing an OHCA victim | 3 (17.6) | 0 (0) | 1 (10) | 0 (0) | 0.250 |
| Preparation score | |||||
| Pre-test | 2.0 (2.0 - 3.0) | 3.0 (2.0 - 3.0) | 2.0 (1.0 - 3.0) | 2.0 (2.0 - 3.0) | 0.091, 0.058 |
| Post-test | 5.0 (3.0 - 6.0) | 4.0 (2.0 - 4.0) | 4.0 (3.5 - 6.0) | 2.0 (2.0 - 3.0) | 0.008, 0.669 |
| Retention-test | 2.0 (2.0 - 5.5) | 2.0 (1.0 - 4.0) | 4.0 (3.5 - 5.25) | 2.0 (2.0 - 3.0) | 0.118, 0.210 |
| ABC score | |||||
| Pre-test | 0.0 (0.0 - 0.0) | 0.0 (0.0 - 0.0) | 0.0 (0.0 - 0.0) | 0.0 (0.0 - 0.0) | 1.000, 1.000 |
| Post-test | 23.0 (21.5 - 24.0) | 18.0 (17.0 - 24.0) | 21.0 (16.5 - 23.0) | 0.0 (0.0 - 0.0) | < 0.001, 0.057 |
| Retention-test | 20.0 (18.5 - 23.0) | 15.0 (13.0 - 22.0) | 20.5 (16.5 - 23.0) | 0.0 (0.0 - 0.0) | < 0.001, 0.121 |
| Total score | |||||
| Pre-test | 2.0 (2.0 - 3.0) | 3.0 (2.0 - 3.0) | 2.0 (1.0 - 3.0) | 2.0 (2.0 - 3.0) | 0.091, 0.058 |
| Post-test | 27.0 (24.5 - 29.5) | 21.0 (20.0 - 28.0) | 26.0 (21.0 - 27.25) | 2.0 (2.0 - 3.0) | < 0.001, 0.083 |
| Retention-test | 24.0 (21.5 - 27.0) | 18.0 (14.0 - 26.0) | 24.5 (20.75 - 27.25) | 2.0 (2.0 - 3.0) | < 0.001, 0.140 |
4.2. Pre-Test Results
The result of the pre-test showed that all participants were deficient in CPR skills and there was no difference between groups in terms of preparation score, ABC score, and the total score (P value = 0.091, 1.000, 0.091, respectively). The median (IQR) of total score was 2.0 (2.0 - 3.0), 3.0 (2.0 - 3.0), 2.0 (1.0 - 3.0), and 2.0 (2.0 - 3.0) in groups 1 - 4, respectively.
4.3. Post-Test Results
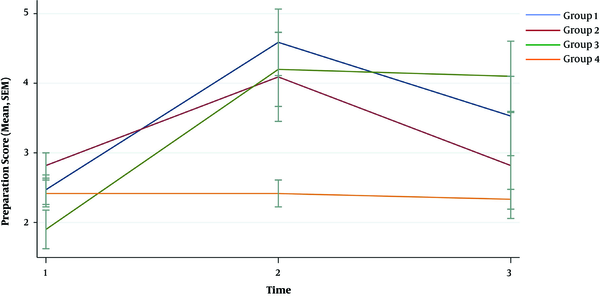
The median (IQR) score of groups 1-3 increased significantly after providing the intervention compared to the pre-test results (overall P value of interaction < 0.001, indicating that all interventions had a positive effect in increasing the scores compared to the control group). Group 3 (video only) experienced the highest increase in the preparation score. While, the increase (95% confidence interval) in preparation score was 2.12 (1.10 - 3.13), 1.27 (0.15 - 2.40), and 2.30 (1.15 - 3.45) for groups 1 - 3, respectively, compared to the control group.
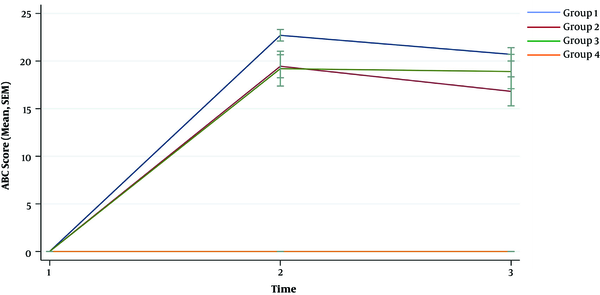
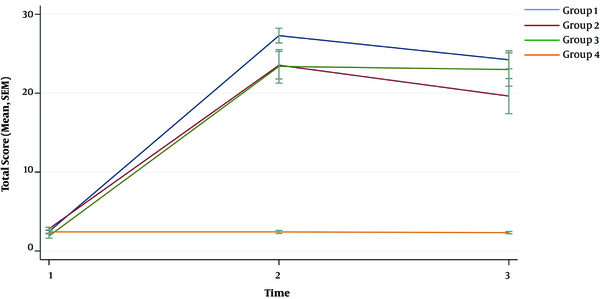
Concerning the ABC score and total score, group 1 (class session) showed the highest increment of scores. The increment (95% confidence interval) of ABC score was 22.70 (20.41 - 25.00), 19.45 (16.91 - 22.00), and 19.20 (16.60 - 21.80) for groups 1 - 3, respectively. The increment (95% confidence interval) of total score was 24.82 (21.84 - 27.80), 20.73 (17.43 - 24.02), and 21.50 (18.12 - 24.88) for group 1 - 3, respectively.
4.4. Retention-Test Results
For all intervention groups, the preparation, ABC, and total scores were higher, even one month after the instructions, compared to the control group (P value < 0.001). However, the scores decreased significantly compared to the post-test results. We developed a sustainability model to evaluate the effect of time on the retention of CPR skills. Group 3 (video only) showed the most sustained results compared to groups 1 and 2 (class session and video + manikin). In terms of preparation score, groups 1 and 2 showed a significant decrease in preparation score compared to group 3 (P value = 0.001, < 0.001). Moreover, groups 1 and 2 showed significant decrease in ABC and total scores compared to the group 3 (P value for ABC score = 0.007, 0.001; P value for total score = 0.001, < 0.001). The trends of changes between the pre-test, post-test, and retention test scores are illustrated in Figures 2-4 separated by the intervention group.
5. Discussion
According to the results, the classroom session teaching with a manikin practice accompanied better acquisition of CPR skills. However, using a simple video to teach CPR skills had better retention generally. We also found that the video only group experienced higher preparation score (also called “responsiveness” in other studies).
Previous studies have shown degradation of CPR skills months after training, which is consistent with our results (24, 25). This is logical, as trainees are supposed to perform and remember up to 50 psychomotor skills (26). Degradation depends on many factors. A study showed that among emergency physicians the performance of CPR was not deteriorated with time (27), while other aforementioned studies reported deterioration of skills in bystanders. The subjects’ personal relationship with a high-risk patient is also shown to be correlated with the retention of CPR skills based on higher personal motivation to learn (28). Frequent exposure is another factor that may maintain retention of the skills, as more practice will improve skills retention (29).
We found that the addition of psychomotor skill practice would not improve the acquisition or retention of CPR skills, which is consistent with the study of Bobrow et al. (15). They also found that the addition of psychomotor practice would neither improve the performance nor the retention of hands-only CPR skills. They also showed that a brief video has a better influence than a common video. This may be justified by the fact that when the video is brief and not accompanied by a second psychomotor practice, the participants can focus on the most fundamental aspects of CPR, and this will improve the performance and retention of CPR skills (15). Here we should state that our method in video + manikin group was “watch, then practice”, which is slightly different from “practice, while you watch”. “Practice, while you watch” method has been shown to perform as well as conventional CPR training in infant mothers (30); however, this cannot be compared to our video + manikin method.
We also found that concerning responsiveness (preparation score), the video-only group was superior to other groups, while classroom sessions provided a better ABC score. A study by Beskind et al. (31) showed that using a brief video or a classroom training course would improve CPR skills performance. They also showed that the administration of a brief video would accompany better responsiveness, while some skills, including depth of compression, would not improve by this type of intervention (31). Many other factors are also crucial to CPR quality, including hands-off time. Studies have shown that as hands-off time enhances, the morbidity and mortality will increase (6, 32, 33). Hands-off time has also been shown to decrease after a brief video demonstration, which supports the benefits of using a video-only method for bystanders (31).
We found that the classroom session group had better initial performance compared to other groups concerning the perspective of the ABC score. This finding is consistent with the result of a study by Chung et al. (34). They showed that participants who were attended at classroom training had better initial performance than self-instructed participants. They also justified this by the fact that the imparting of individual skills might be better in classroom training. Also, self-instructed materials (video and kits) may be an important factor in determining the performance of CPR (34). However, the superiority of a method should be addressed by long-term retention. The initial performance seems to be less important than the retention of skills (34). A beneficial strategy to maintain retention of skills is a refresher course program, which is more feasible with the self-instruction methods (34, 35).
The current study had some limitations, such as not assessing the subjective effect of CPR training skills, including self-confidence and willingness, to perform CPR in public. Previous studies have shown that different methods of teaching possess different subjective feelings (34). We also did not use a real-time objective feedback method due to the limitation of resources. Studies have shown that real-time measurement of key metrics during CPR improves the quality of CPR (36-38). We followed participants for one month, while longer follow-up is needed to comprehensively assess the retention of skills. Moreover, the hands-off time was not measured in the present study, while many factors, including hands-off time, can influence the quality of CPR.
5.1. Conclusions
Based on the results, the classroom session teaching with a manikin practice accompanied better acquisition of CPR skills. However, the retention of CPR skills, which is more important to CPR performance, is better maintained with a simple video-only method.