1. Context
Asthma is a heterogeneous disease characterized by reversible airway obstruction and chronic inflammation. It has been estimated that about 300 million people suffer from chronic asthma worldwide (1). Inflammation is the primary pathological mechanism leading to hyperresponsiveness and airway remodeling in asthma patients; it also plays a vital role in the occurrence and development of asthma (2). In addition to chronic airway inflammation, systemic inflammatory mast cell activation occurs in patients with asthma, mediated by a variety of cell cytokines (e.g., eosinophilic neutrophils, macrophages, platelets, etc.) and a variety of mediators, which have been considered crucial in the development of clinical asthma (3, 4).
Research on neutrophil-to-lymphocyte ratio (NLR) has gained interest over recent years. Systemic inflammation measured by NLR has a significant association with prevalent chronic conditions (5, 6). In asthma patients, a high NLR is associated with an increased risk of severe exacerbation, and NLR has been suggested as a useful marker for asthma (7). Research has shown that NLR and PLR may be potential diagnostic indices for pediatric recurrent wheezing (8). However, the role of NLR in the diagnosis and assessment of bronchial asthma remains unclear.
2. Objectives
The purpose of this meta-analysis was to explore the role and clinical significance of NLR in the diagnosis of bronchial asthma so as to provide a theoretical basis for the diagnosis of bronchial asthma.
3. Methods
3.1. Literature Search
A comprehensive search for studies on NLR that distinguished asthmatic patients from healthy people was conducted using EMBASE, PubMed, and Cochrane databases prior to 10 April 2020. The search strategy (Table 1) and query criteria were as follows: (((NLR[Title/Abstract]) OR ((neutrophil[Title/Abstract]) AND lymphocyte[Title/Abstract]))) AND ((asthma[Title/Abstract]) OR "Asthma"[Mesh]). This is a meta-analysis, and ethical approval was not required.
| Step No. | Query |
|---|---|
| #1 | “neutrophil” [Title/Abstract] |
| #2 | "lymphocyte"[Title/Abstract] |
| #3 | "NLR"[Title/Abstract] |
| #4 | “asthma” [Title/Abstract] |
| #5 | "asthma "[Mesh] |
| #6 | #1 AND #2 |
| #7 | #3 OR #6 |
| #8 | #4 OR #5 |
| #9 | #7 AND #8 |
Abbreviation: MeSH, medical subject headings.
a This table provides details on how the literature was searched in various databases.
3.2. Study Selection
Criteria for the inclusion of articles were the following: (1) evaluating asthmatic patients and healthy controls; (2) addressing NLR; and (3) studying mild or stable asthma. The exclusion criteria comprised of: (1) being reviews; conference abstracts, non-human research, comments, and letters; and (2) not including a control group.
3.3. Data Extraction
The two researchers independently read the literature and extracted the data according to the inclusion and exclusion criteria. The following data were extracted: (1) the first author, (2) the country, (3) the year, (4) the number of patients, (5) the mean age, (6) the gender ratio, and (7) the NLR.
3.4. Quality Assessment
A modification of the Newcastle-Ottawa scale (NOW) was used for the quality evaluation of the literature (9). This scale consists of the following three parts: (1) patient selection, (2) comparability between the two groups, and (3) the evaluation of outcomes of interest. The total score is nine, and an article with a score of six or more is of high quality (Table 2).
| Author | Year | Nation | NOWS Score | Total Number | Gender Ratio (M: F) | Age (y) | NLR | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Asthma Group | Healthy Group | Asthma Group | Healthy Group | Asthma Group | Healthy Group | Asthma Group | Healthy Group | ||||
| Beyhan S. (10) | 2020 | Turkey | 8 | 80 | 22 | 57: 23 | 7: 15 | 41.5 ± 11.6 | 42.0 ± 10.5 | 1.8 ± 1.5 | 1.8 ± 1.85 |
| Dogru M. (11) | 2016 | Turkey | 6 | 469 | 170 | 266: 203 | 90: 80 | 8.58 ± 3.25 | 8.71 ± 3.03 | 2.07 ± 1.41 | 1.77 ± 1.71 |
| Hendy R. M. (12) | 2019 | Egypt | 8 | 45 | 45 | 20: 25 | 16: 29 | 37.82 ± 14.54 | 33.07 ± 10.89 | 2.77 ± 1.87 | 1.4 ± 0.52 |
| Nacaroglu H. T. (13) | 2016 | Turkey | 7 | 54 | 94 | 27: 27 | 47: 47 | 10 ± 3 | NA | 2.4 ± 0.3 | 1.5 ± 1.2 |
| Shi G. (14) | 2017 | Chinese | 6 | 175 | 130 | 60: 115 | 40: 90 | 47.94 ± 12.63 | 49.51 ± 13.58 | 1.99 ± 1.15 | 1.68 ± 0.51 |
| Yildiz E. (15) | 2020 | Turkey | 6 | 150 | 150 | 80: 70 | 78: 72 | 35 ± 3.1 | 38 ± 2.5 | 2.8 ± 1.4 | 1.7 ± 0.5 |
Abbreviations: NOW score, the score of Newcastle-Ottawa Scale; NLR, neutrophil-to-lymphocyte ratio; NA, not applicable.
a Values are expressed as mean ± SD unless otherwise indicated.
3.5. Statistical Analysis
The forest plots were established using the random model in the new methodology, and heterogeneity testing was also conducted in this study. Review Manager (RevMan, version 5.3. Copenhagen: The Nordic Cochrane Centre, the Cochrane Collaboration, 2014) was used for data analysis.
3.6. Grouping Description
The overall analysis included six studies. Subgroup 1 included four studies performed among adults, and subgroup 2 included children as cases. Subgroups 3 and 4 included two subgroups with no obvious heterogeneity, which were generated by excluding each study one by one in order to analyze the heterogeneity of the overall analysis group.
4. Results
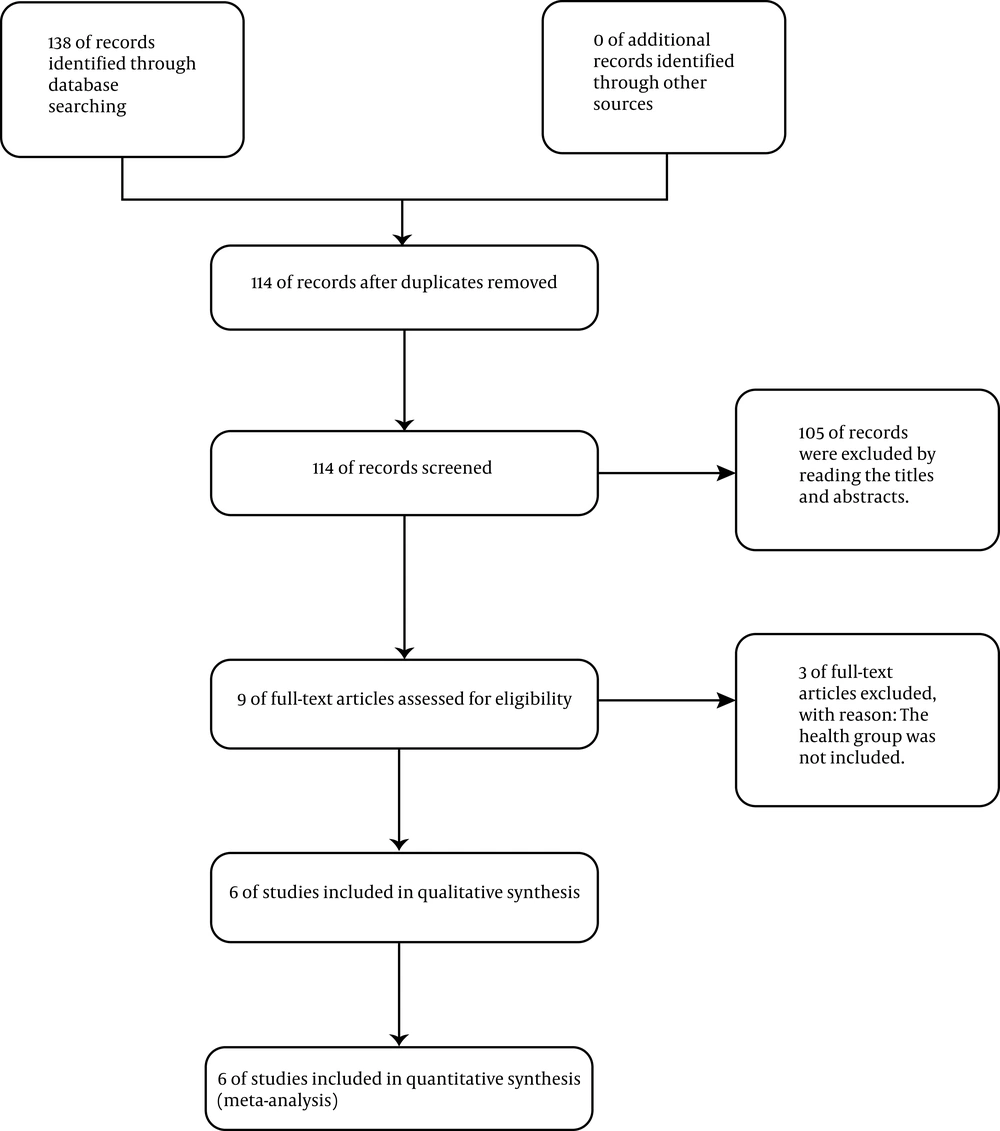
According to the search criteria, we retrieved 138 articles, 24 of which were duplicates. One hundred and five articles were excluded by scanning the titles and abstracts. Finally, six articles (10-15) were included in this study. The selection process of the literature is presented in Figure 1.
4.1. Study Characteristics
Demographic characteristics are shown in Table 2.
4.2. Heterogeneity Test
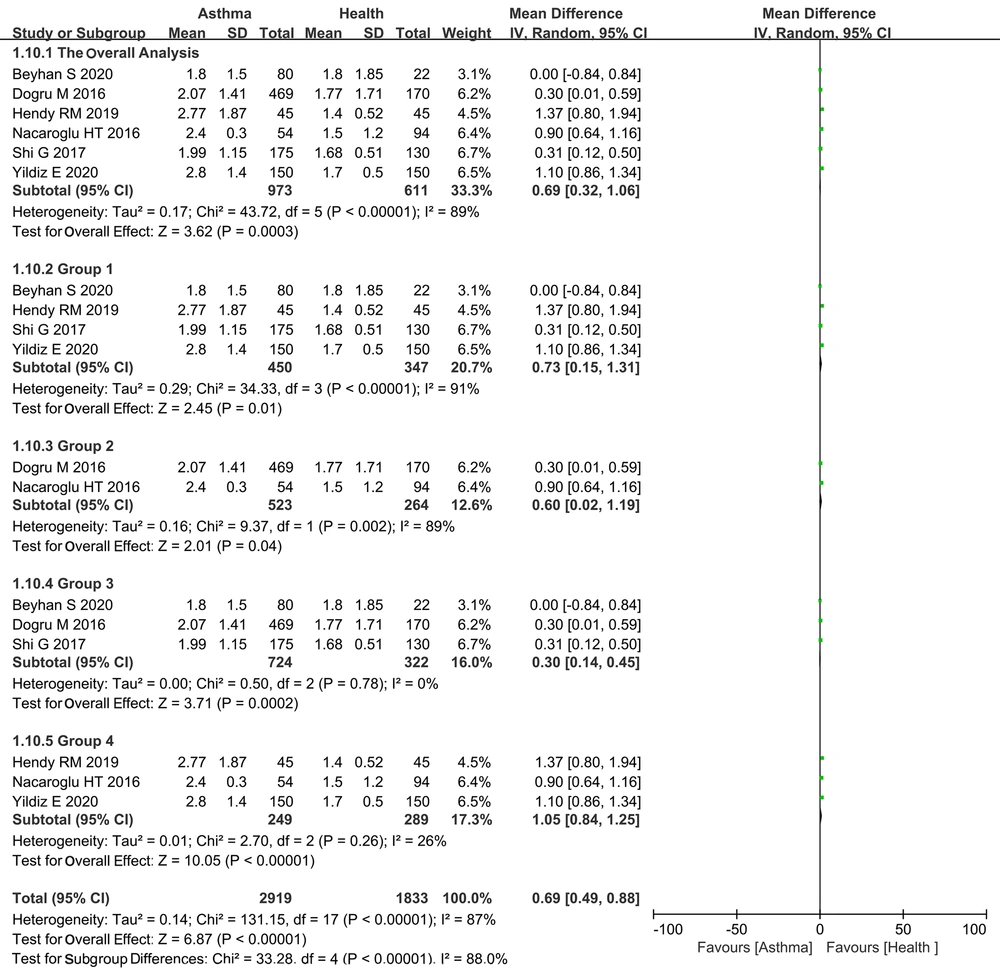
The heterogeneity of the overall analysis and subgroups 1 and 2 were high, I2 = 89%, I2 = 91%, and I2 = 89, respectively. We used the random model for analysis. There was no obvious heterogeneity in subgroups 3 and 4, I2 = 0% and I2 = 26%, respectively.
4.3. The Mean Difference
This study showed that the comprehensive mean differences between the two groups in overall and subgroups 1 and 2 were 0.69, 0.73, 0.60, 0.3, 1.04, respectively, which was statistically significant (P < 0.05; Figure 2). The comprehensive mean difference of asthmatic groups was higher than that of healthy groups.
Forest plots showing the mean difference with corresponding 95%. Confidence intervals (CIs) for NLR in asthma and healthy group in each study. Overall analysis, including six articles. Subgroup 1 included four studies with included adults cases, and subgroup 2 included children as cases. Subgroups 3 and 4 included two subgroups with no obvious heterogeneity, which were generated by excluding each study one by one in order to analyze the heterogeneity of the overall analysis group.
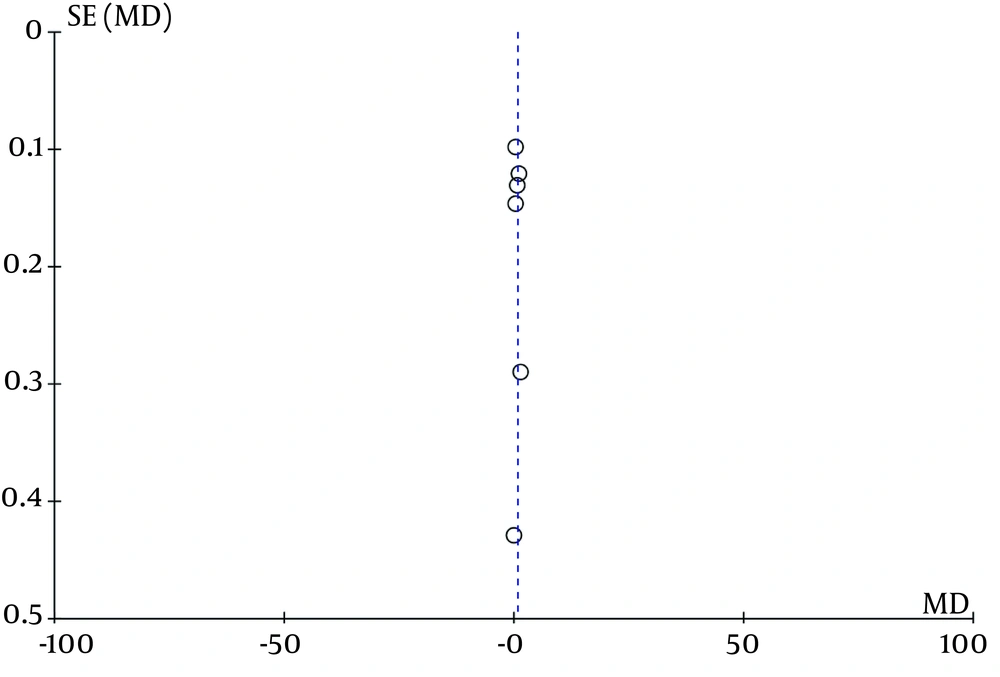
4.4. Publication Bias
A funnel plot was used to evaluate possible publication bias (Figure 3).
5. Discussion
Neutrophils participate in airway inflammation and are activated in inflammatory pulmonary diseases such as asthma (16). NLR is likely to be a biomarker for airway and systemic inflammation (5), and it may be different in asthmatic patients and healthy people. Four studies (11-13, 15) showed that the ratio of neutrophils to lymphocytes was significantly different between control groups and asthma groups. In contrast, two studies (10, 14) showed no significant difference between asthma and healthy groups.
In sum, our results suggested that NLR in asthmatic patients was significantly higher than that in healthy individuals, both among adults and children. NLR can be used to distinguish asthmatic patients from healthy people, and increased NLR has a certain clinical value in distinguishing asthma patients from healthy people (14). Because the heterogeneity of the overall analysis was very high, heterogeneity analysis was performed to identify the possible causes of heterogeneity. We found that no obvious heterogeneity in subgroups 3 and 4 through the one-by-one elimination method. In addition to these two subgroups, there was high heterogeneity in any combination of three or more studies.
Some limitations in the present study need to be pointed out. First, only a few studies were included. Second, the included studies were all non-randomized controlled and retrospective studies. More prospective multicenter studies are needed to further verify our findings.
6. Conclusions
The ratio of neutrophils to lymphocytes in the peripheral blood of asthmatic patients is higher than that in healthy individuals. This result has certain clinical value in distinguishing asthma patients from healthy people.