1. Introduction
Human resources are an asset to the organization, and the dissatisfied employee is the organization's first enemy. Therefore, employees should be treated as assets and not debts, and this is only possible through the process of designing a human job, known as the quality of working life. In this regard, in order to increase labor productivity and create attachment in the work environment, thinkers in the management of transformation and improvement of organizations have proposed the quality of work life (QWL), which is called an ideological movement (1). QWL can be defined as the level of employee participation in the work environment to achieve the goals of the organization according to the satisfaction of meeting individual and job needs (2). In relation to nurses, paying attention to the QWL is one of the important elements in providing health services, which, if not considered, can lead to a decrease in the performance of nurses and the tendency of nurses to resign from the nursing job (3).
The desired level of QWL has a significant effect on an individual's commitment to the organization (4). Numerous studies have been conducted on the positive effect of QWL on various organizational and individual components such as employee commitment (5), organizational effectiveness (6), correlation and inverse effect of QWL on various organizational and individual components such as turnover, absence, leaving work, and work-family conflicts (7).
One study evaluated the relationship between job stress and QWL of nurses working in selected hospitals of the Armed Forces, reporting that the level of QWL of most nurses (81%) was moderate, and there was a negative correlation between job stress and QWL of nurses and positive interaction (8). In addition, the QWL is affected by various factors such as working hours, lack of facilities, insufficient hours off, management practices, lack of sufficient opportunities for advancement, unfavorable working conditions, lack of staff, and income level (9). In another study on the QWL of nurses, it was reported that 60% of nurses have an average QWL, 37.1% have an unfavorable QWL, and 2% have a good QWL (10). Research on the quality of life among nurses showed that 67.2% of nurses were dissatisfied (7), and 40% were dissatisfied with their working life (11). In examining the relationship between organizational justice and QWL and the mediating role of organizational culture in this regard, it has been suggested that there is a positive correlation between organizational justice and its components with QWL, between organizational justice and its components with organizational culture, and organizational culture with QWL. Findings have also shown that organizational culture plays a mediating role in the relationship between organizational justice and QWL (12).
One way to ensure that nurses' QWL is assessed is to use a valid measurement tool. This requires measurement under a validation method that demonstrates the accuracy of the measurement. In this regard, Walton first designed the dimensions of QWL in the 1970s and a general questionnaire of QWL in eight areas, including fair and adequate pay, safe and healthy work environment, human resource development, opportunity for growth and continuous security, social integration and cohesion., legalism, the general atmosphere of life, and the social dependence of work life (13). Moreover, Ventegodt et al. developed the Self-Evaluation of Working Life Quality Questionnaire (SEQWL) based on the Global Quality of Life Scale (GQOL). This tool relies on the individual's mental judgment, and the interpretation of the collected data requires a process of deep understanding of the nature of the individual's consciousness and precise methodological criteria (14). However, it should be noted that the best tools are those that are taken from people's lived experiences, and the content related to the tools is taken directly from the reference people. If the structures of QWL result from the intellectual formats of the participants, it can be stated with confidence that the created tool has considered all the dimensions related to the concept in the statistical population. On the other hand, knowledge of the validation characteristics of the tool can be a guide for researchers to choose the appropriate tool for research in the field of health. It can also help tool designers to design and present a tool with the desired quality of credit (15).
Today, one of the main issues in contemporary research studies is the selection of appropriate and relevant measurement tools, which is as important as conducting research and preparing scientific documents (16). In addition to producing a standard tool, it will help policymakers to improve the organization's physical and psychological environment, behaviors, and performance, as well as manage the maintenance of the workforce according to the cost-effectiveness rule with a focus on behavioral effectiveness and organizational economics (17).
One of the criteria for selecting an appropriate instrument is the consensus-based standards for the selection of health status measurement instruments (COSMIN) in a Delphi international study proposed by Mokkink et al., which examines the characteristics of validation, including reliability, validity, responsiveness, and interpretability of the instrument (18).
The checklist consists of 12 areas. Ten areas can be used to assess whether a study meets standards of good practice. Nine of these domains contain standards for character measurement, including internal consistency, reliability, measurement error, content validity (including face validity), construct validity, hypothesis testing, and intercultural validity. In addition, two areas in the checklist include general specifications for articles to which item response theory (IRT) methods are applied and the general requirements for generalizability of results (18).
In previous research, different dimensions of the QWL of nurses have been measured using various tools. Therefore, this study aimed to systematically review the studies conducted on the QWL of nurses and present them in a systematic review using the COSMIN chloramphenicol. This can help policy makers to plan for better and more complete employment conditions for nurses.
2. Methods
This systematic review and meta-analysis evaluated the QWL of nurses based on available sources and documents. Five major databases, including Google Scholar, PubMed, ScienceDirect, Scopus, and Web of Science were searched for relevant papers published between 2000 and October 2020 using the following keywords: ‘nurse’, ‘nursing work life’, ‘quality of work life’, ‘nurses' quality of work life’, and ‘scale’.
First, we prepared a list of titles and abstracts of all articles in the mentioned databases and examined them separately to select the relevant titles. The required key data were extracted from the articles and recorded in a form, which included the following information: General information related to the article (title and time of the study), study details (sample size and method), and the results. Then, the related articles entered the research independently. All the included studies assessed the QWL of nurses. The exclusion criteria were: Articles measuring the quality of working life for other jobs, review studies, studies related to other organizational factors, studies published before 2000, books and dissertations, and lack of access to the full-text of the article.
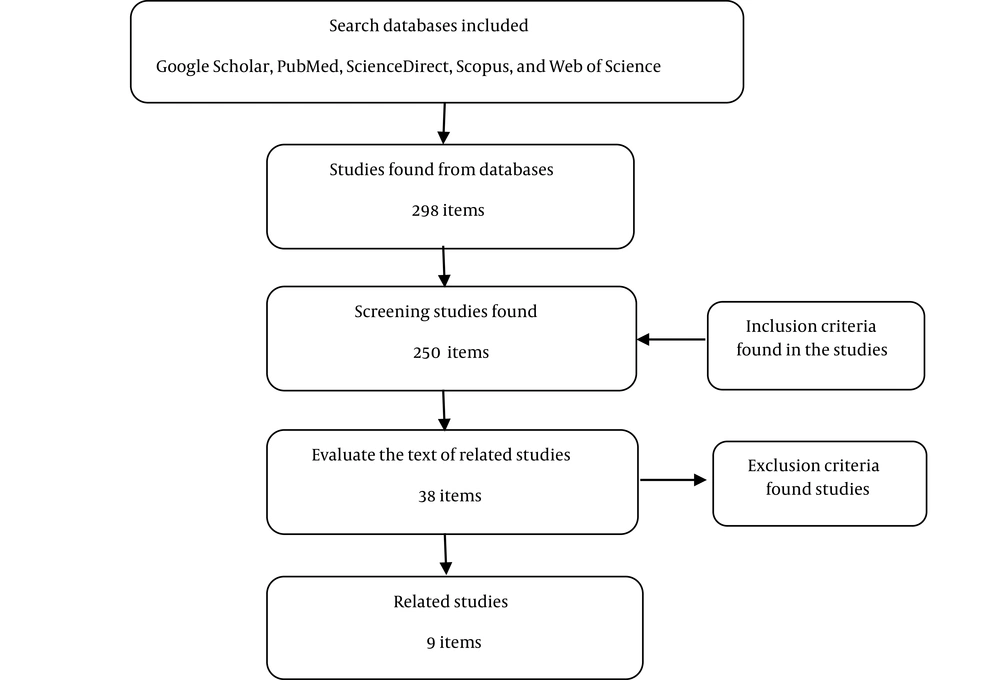
A total of 298 articles were selected and organized in the Endnote software. In the next stage, after reviewing the titles and abstracts, the related articles were identified and entered the third stage. Next, we evaluated the qualitative and quantitative aspects of the articles in terms of type of study, statistical method, and sample type, and deleted 289 articles. Finally, nine articles were selected based on inclusion criteria (Figure 1).
The criteria for evaluating the quality of studies included the following: Method of research, validity and reliability of data collection and analysis tools, sample size, and data collection method.
3. Results
Out of 298 articles (55 articles in PubMed, 36 articles in Scopus, 87 articles in Web of Science, 20 articles in ScienceDirect, and 100 articles in Google Scholar), 288 articles were excluded from the study due to duplication, inconsistency with the study aims based on screening the abstracts, and lack of access to full-text of the articles.
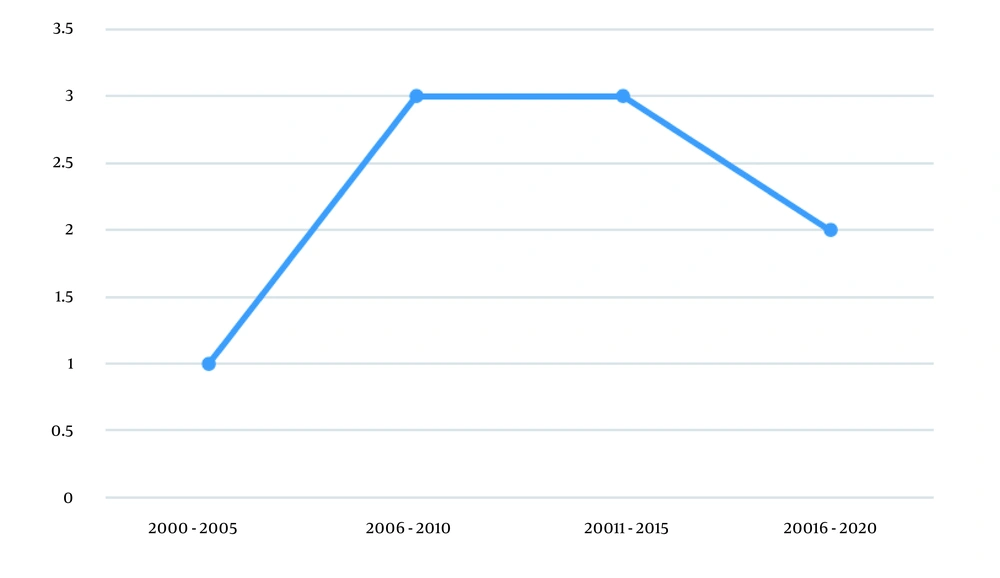
More than half of the studies had been conducted after 2010 (Figure 2), which can be considered due to their greater role in the health care system (19). Table 1 presents the main characteristics of the valid articles validated in this review study.
| No. | Name of Scale | Scale Maker | Samples | Number of Items | Factors | Content Validity | Construct Validity | Internal Consistency | Reliability | Responsiveness/Interpretability |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | The Chinese Quality of Nursing Work Life Scale | Su & Shieh (20) | Nurses | 57 items; 13 factors | Work environment, rewards, benefits, promotion, training and development, automation, boss leadership, interpersonal interactions, communication, organizational system, organizational climate and culture, working hours / workload and family / social factors | Not mentioned | Factor analysis | α = 0.88 | Test-retest (r = 0.89) | Not mentioned |
| 2 | English version Quality of Nursing Work Life | Brooks et al. (21) | Nurses | 42 items; 4 factors | Individual life-work life, work design, work field, and work world | Nursing experts | Factor analysis | α = 0.91 | Test-retest (r = 0.83) | Not mentioned |
| 3 | The Work-Related Quality of Life Scale (WRQOLS) | Van Laar et al. (19) | Health care professionals and nurses | 23 items; 6 factors | Job satisfaction, general well-being, stress at work, control at work, home-work relationship and working conditions | Expert panel | Exploratory and confirmatory factor analysis | α = 0.91 | Split-half factor | Not mentioned |
| 4 | The scale for the quality of work life of Iranian nurses | Vagharseyyedin (22) | Nurses | 67 items; 9 factors | - | Tool making specialists | Exploratory factor analysis; | α = 0.76 | Test-retest (r = 0.77) | Not mentioned |
| 5 | Thai Version of a Work-related Quality of Life Scale | Sirisawasd et al. (23) | Nurses | 34 items; 7 factors | Employee interaction, work control, home-work relationship, public welfare, job and professional satisfaction, work position, work stress | Nursing experts | Factor analysis | α = 0.97 | Test-retest (r = 0.892) | Not mentioned |
| 6 | Turkish Version of Quality of Nursing Work Life Scale | Sirin & Sokmen (24) | Nurses | 35 items; 5 factors | Work environment, relationships with managers, working conditions, job perception, support services | Nursing specialists and experts | Exploratory and confirmatory factor analysis | α = 0.89 | Test-retest (r = 0.75) | Not mentioned |
| 7 | Chinese version of the Quality of Nursing Work Life Scale | Fu et al. (25) | Nurses | 42 items; 4 factors | Individual life - work life, work design, field work, and work environment | Nursing experts | Chi-square; RMSEA; AIC; CAIC; GFI & CFI. | α = 0.912 | Test-retest (r = 0.74) | Not mentioned |
| 8 | Quality of Nursing Work Life Scale-Korean | Kim et al. (26) | Nurses | 36 items; 3 factors | Work context, personal / work life support systems, work design and staff | Nursing professors | Exploratory factor analysis; | α = 0.93 | Test-retest (r = 0.90) | Not mentioned |
| 9 | Taiwanese Version of the Work-Related Quality of Life Scale for Nurses | Dai et al. (27) | Nurses and other medical staff | 23 items; 5 factors | Job satisfaction, public welfare, stress at work, control at work, home-work relationship | Not mentioned | Factor analysis | α = 0.88 | Test-retest (r = 0.89) | Not mentioned |
4. Discussion
The results of the study showed that most of the valid tools used in the research related to nurses' QWL can be used for nursing staff. Due to the unique working conditions in the nurses’ work environment, special accredited tools are needed to measure the nurses' QWL.
We identified nine valid tools, seven of which evaluated the QWL based on nurses' experiences. Also, the tools were validated, and features were evaluated based on the COSMIN checklist. Although the articles did not mention the COSMIN checklist, they all considered the main indicators of reliability (internal consistency and stability) and validity. The number of items and factors had been expressed in all cases. The structural validity of eight questionnaires was determined using factor analysis and a tool with chi-square test, root mean square error of approximation (RMSEA), Akaike information criterion (AIC), comparative-analysis by independent contrasts (CAIC), goodness of fit index (GFI), and comparative fit index (CFI). The stability of all the above instruments was acceptable using Cronbach's alpha coefficient and reliability (retest r > 0.7). A high level of internal consistency indicates a high correlation between items, and that the relevant tools can measure the concept. Also, the results of internal consistency in all questionnaires reported high values of Cronbach's alpha, indicating that they are suitable for the purpose of the study.
The first tool mentioned in the present study was designed with 57 items and 13 factors; factor analysis showed internal consistency of 0.88, and the correlation between test-retest during two weeks was high (r = 0.89), which indicates good reliability (20).
The second instrument was determined by Brooks in the United States in 2000 with 42 items, four factors, and a 6-part Likert scale. The minimum score was 42, and the maximum was 252, with higher overall scores indicating a better QWL. Alpha coefficients for factors ranged from 0.45 to 0.60, and the total score of correlation coefficient ranged from r = 0.24 to 0.68. Brooks reported that QWL for nurses is a valid and reliable tool (21).
The results of the third study indicated that the overall reliability of the instrument with 23 items, six factors, and a 5-part Likert scale was 0.91, and the reliability of the subscales was between 0.76 - 0.91, indicating a good reliability. In this study, there was no reference to the responsiveness and interpretability of the instrument (22).
The fourth study determined the construct validity using heuristic factor analysis for nine factors, which in total accounted for 4.59% of the total variance of the factors. Cronbach's alpha indicated that the appropriate internal consistency of the instrument was 0.76. The reliability of stability through test-retest showed a correlation coefficient of 0.77. The results of the study showed that the introduced tool was a suitable tool for measuring the QWL (23).
In the fifth study, the overall content validity index (CVI) was 0.97, and there was a strong relationship between test and retest (r ¼ 0.892, P < 0.05). In addition, seven factors had high reproducibility (0.65 < r < 0.78; P < 0.05) (24).
In the sixth study, a 6-part Likert scale was used to measure 35 items and five factors. During the two-week period, 96 respondents participated in the test and retest and the correlation was obtained for the whole instrument (r = 0.75, P < 0.001). There was no significant difference between the two weeks of the test (t = 0.524, P > 0.05) (25).
In the seventh study, internal consistency (α = 0.912) and reliability with test-retest (ICC = 0.74) showed high values. RMSEA value was 0.091, AIC value was 1806.00, CAIC value was 7730.69, CFI value was 0.93, and GFI value was 0.74. The QWL scale for nurses was valid in Chinese nurses, and it could be suggested as a clinical and research tool for measuring work-related factors among Chinese nurses (26).
In the eighth study, the lowest score was 42, and the highest score was 252 on the 6-point Likert scale (the higher the score, the higher the QWL). The reliability of the test and retest was 0.90 (27).
The results of the ninth study showed that the Work-Related Quality of Life (WRQoL) had good reliability and overall credibility for QWL assessment of nurses in Taiwan. In addition, the WRQoL-T template was the same as the main WRQoL scale, consisting of 23 items and a 5-point Likert scale. Therefore, technical equality with the main tool was ensured. Another strength of WRQoL-T was that the validity of the instrument with test-retest test (within three weeks) was 0.89 (P < 0.001), which was higher than 0.70, which is considered acceptable for a new tool (28). It also had an overall alpha coefficient of 0.88, which is approximately equal to the original WRQoL alpha, indicating excellent internal consistency reliability. The reliability of the subscale ranged from 0.68 to 0.84, which is acceptable (19).
Despite the validity and reliability of the tools mentioned in previous studies, other COSMIN checklist criteria such as standard validity and measurement error have not been mentioned. Criterion validity examines the ability of a tool to predict an individual's behavior in defined specific situations and each individual's performance relative to a criterion such as the Standard Gold. One of the standard deviations is the distribution of error scores (28).
Responsiveness (sensitivity to change and responsiveness) and interpretability (quality of change significance) were other items of the COSMIN checklist not addressed in the tools mentioned in the study.
4.1. Conclusions
Nurses are the largest group of staff in hospitals. Identifying the factors related to the QWL of nurses can provide important information for nursing managers to design and create management applications to make the nursing profession more attractive. In the present study, we evaluated the tools according to the COSMIN checklist. The results showed that the used tools had acceptable validity and reliability and were suitable for evaluating the QWL of nurses.
Applied clinical tips for military communities:
• Emphasis on the need to design tools with acceptable and appropriate accreditation features for military nurses
• Implementing the necessary interventions to improve organizational productivity using the results of special tools for military nurses