1. Context
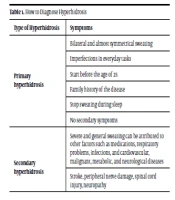
Hyperhidrosis is more severe sweating than the body’s physiological needs to balance the body’s temperature (1, 2). It often appears in the palms, soles of the feet, and armpit area with the accumulation of perspiration glands and causes individual and social problems (3, 4). People with hyperhidrosis have difficulty using metal, paper, and electronic tools, which impairs the social functioning of individuals and causes material and spiritual damage to societies (5, 6). According to studies, the prevalence of this disease is between 1% and 2%. Based on the causes of hyperhidrosis, this disease can be divided into 2 categories: Primary and secondary hyperhidrosis (7). In primary hyperhidrosis, except for heredity (8), the causes of the disease are unknown. However, the secondary type of the disease can be attributed to diseases, intense exercise, or certain medications (9). Nowadays, there are various treatment methods for effective treatment of this disease, and the method of choosing these treatment methods depends on the severity of the disease, area of the disease, age of the patient, and costs. The first step in the treatment of hyperhidrosis is to diagnose the disease. To diagnose primary hyperhidrosis, observing severe and concentrated sweating for 6 months without any cause with 2 symptoms of Table 1 is required.
| Type of Hyperhidrosis | Symptoms |
|---|---|
| Primary hyperhidrosis | Bilateral and almost symmetrical sweating |
| Imperfections in everyday tasks | |
| Start before the age of 25 | |
| Family history of the disease | |
| Stop sweating during sleep | |
| No secondary symptoms | |
| Secondary hyperhidrosis | Severe and general sweating can be attributed to other factors such as medications, respiratory problems, infections, and cardiovascular, malignant, metabolic, and neurological diseases |
| Stroke, peripheral nerve damage, spinal cord injury, neuropathy |
The secondary type of hyperhidrosis can generally be due to secondary factors such as neurological diseases and social anxiety diseases. In some cases, damage to peripheral nerves and stroke can also be the causes of this disease in people.
2. Evidence Acquisition
In this narrative review, the data about hyperhidrosis treatments were selected and reviewed from databases such as ScienceDirect, PubMed, Springer, Wiley Online Library, Google Scholar, etc. The time range of articles includes from 1980 to 2021. Selecting articles started with searching for keywords such as hyperhidrosis, topical antiperspirants, tap water iontophoresis, Botox injection, hyperhidrosis surgical solutions, etc.
3. Results
3.1. Topical Therapy
Local antiperspirants are at the forefront of treatment methods for hyperhidrosis (10, 11). These drugs are simply available in pharmacies and have very few side effects. This family’s most widely used drugs are aluminum chloride hexahydrate (12, 13) and aluminum chloride 20% (14, 15). The efficiency of these drugs is that aluminum metal salts interact with sweat mucopolysaccharides and cause obstruction of the sweat duct by creating sedimentation (16). In using these drugs, sweating is done within the body, but these drugs reduce sweating by mechanical obstruction of the exit site of the perspiration glands. This treatment is a temporary method that is suitable for less severe cases. One of the results of using these drugs is changes in the form of sweating glands. Recently, studies have shown that topical antiperspirant therapy can alter the form of perspiration glands (17). The use of these drugs should also be taken into consideration. For example, the maximum efficiency of using these drugs is at the time of minimum sweating. As a result, it is recommended to use the drug in the area of the disease for between 6 and 8 hours at night. The most common side effect of this method is feeling discomfort in the area of use. The use of aluminum chloride in the armpit area has a high effect due to low skin thickness, although palm and foot sweating decreases due to increased skin thickness and inability to penetrate the skin (12, 18). This treatment method is a suitable option for starting hyperhidrosis patients, especially in less severe cases. This method is inexpensive, simple, and effective and is of interest to physicians.
3.2. Anticholinergic Therapy
Anticholinergic drugs prevent sweating by preventing the effect of acetylcholine, which stimulates postsynaptic muscarinic receptors to force sweat glands to secrete sweat (19, 20). Glycopyrrolate and oxybutynin are used to treat hyperhidrosis. These drugs block acetylcholine activity in parasympathetic spots in smooth muscles, the central nervous system, and sweat glands. This process stops sweating in the perspiration glands. Glycopyrrolate usage has been approved for patients over 11 years old in the USA, and this treatment has been studied in several studies (21, 22). Studies have shown that up to 79% of patients with concentrated hyperhidrosis are treated with glycopyrrolate (21). The required amount of this drug for children is 2 mg daily and for adults up to 4 mg per day (19). However, higher doses may be used to diagnose more severe cases. Methantheline bromide is among the anticholinergic drugs used at a dose of 50 mg and 2 to 3 times a day in Europe to treat subcutaneous hyperhidrosis. Cholinergic drugs show their effectiveness 1 week after treatment. Due to the lack of severe side effects, these drugs can be used for the required period until the results are stable. Due to the systematic absorption of anticholinergic drugs based on the dosage used, side effects can vary. These drugs’ most common side effects are dry mouth, nausea, and headaches. The combination of topical antiperspirants and anticholinergic drugs can also reduce sweating in severe cases of hyperhidrosis. This treatment is used after topical medications for the treatment of hyperhidrosis. However, some patients may leave the treatment process halfway due to the side effects of these drugs.
3.3. Iontophoresis
Iontophoresis is one of the most common treatment methods for hyperhidrosis in the palm of the hand and soles of the feet (23-25). In this treatment method, direct electrical energy with a current of up to 20 mA is used for treatment. Anode and cathode electrodes, an electrical current source, anode and cathode electrodes, a container containing water, and cloth coating are required to treat iontophoresis. The electrical current source provides the necessary electrical energy for the treatment and transmission of ions, and the anode and cathode electrodes are responsible for transferring this current among the skin in the treatment area. Using fabric coating prevents direct contact with the skin and the surface of electrodes from preventing side effects. The use of tap water in this treatment is expected so that water and solutes help transfer ions into the skin. In some studies, antiperspirants are added to the urban water container to occur in the middle of the skin using the drug-supplying iontophoresis method (26). Kim et al. treated palm hyperhidrosis by the iontophoresis method (15). Their study was performed on 29 patients with severe sweating for 2 weeks, with 5 weekly treatment sessions. They showed an improvement in 92.9% of patients, and it was concluded that iontophoresis was a safe and effective method with the help of municipal water. In another study, Yaghoubi et al. (27) compared the effect of municipal water and the normal saline solution on treating a 21-year-old female patient with primary hyperhidrosis. This study showed that using a normal saline solution could be up to 1.7 times more effective than urban water solution in treating this disease. So far, the mechanism of the effectiveness of this treatment has not been investigated, but reasons such as nervous system stimulation, increased threshold of stimulation, and mechanical obstruction of sweating glands have been mentioned as effective methods of this treatment. This treatment is usually a 4-week treatment period and performed in the first week of 4 sessions, in the second week 3 sessions, in the third week 2 sessions, and in the last week for 20 minutes. With all the benefits of this treatment, there are also limitations to using this method. Before starting the treatment session, patients are asked questions to ensure the absence of metal implants, pacemakers, and pregnancy. Side effects of this treatment are rare and include burning sensation, redness, and blistering in the treatment area, which can be prevented by using creams. This treatment is one of the most effective treatment options for hyperhidrosis in the palms and soles of the feet.
3.4. Suction Curettage Surgery
Suction curettage is the beginning of invasive treatments to prevent severe sweating (28, 29). Suction curettage is mainly used for the treatment of hyperhidrosis in the axillary area. In this treatment, sweating glands remove with relatively low invasiveness. This method is a surgical technique with the least possible invasiveness for the treatment of hyperhidrosis. Local anesthesia is used for this treatment, and patients will see sweating discontinuation in a short time. This treatment is invasive, and one of the most critical factors in such treatments is the surgeon’s skill. One of the side effects of this treatment is scar incidence and, in some cases, infection.
3.5. Botox Injection
Botox injections are used as a non-surgical method for treating hyperhidrosis at different severities of the disease (30, 31). Botox blocks acetylcholine release from presynaptic nerve terminals by targeting the snar protein and preventing sweating. The most common type of botulinum used in treating this disease is botulinum type A (32). Patients with myasthenia gravis disease and pregnant women are prohibited from using this treatment. One of the weaknesses of using this treatment method is the temporary inability of people to use palm muscles after Botox injection. It is also a painful procedure for children. The optimum concentration of botulinum type A is between 1 and 2.5 U per 0.1 mL (33, 34). The volume of toxin injected into the skin is 0.1 to 0.2 mL per square centimeter. The injection method should be in the form of an array of injection sites. Depending on the patient’s response, 100 - 150 units of type A toxin are needed to treat each hand. Studies show that patients’ satisfaction after using this treatment is between 80% and 90% (35, 36), and treatment should continue periodically every 6 to 9 months. One of the common side effects of Botox injection is a pain in the injection area. This treatment is effective and straightforward. However, it is costly to repeat the treatment for several periods.
3.6. Sympathectomy
Sympathectomy is the last treatment used in hyperhidrosis treatment if all the mentioned methods do not answer (37-42). Thoracic sympathectomy surgery blocks the upper thoracic sympathetic chain through an incision or clamp. This treatment is suitable for severe sweating in the upper extremities, especially in the palms. One of the requirements for implementing this treatment is the patient’s physical health. Postoperative complications include arterial bleeding, pneumothorax, hemothorax, and limb drowsiness (43, 44).
4. Conclusions
There are several major treatments to confront hyperhidrosis (Table 2). These treatments start with low-cost topical medicines, which are useful for less severe cases. Another family of treatments includes anticholinergic therapy, which can be used in combination with topical antiperspirants to treat severe cases of hyperhidrosis. Iontophoresis, as a novel and promising treatment for different diseases, has been used. This method may provide a uniform, high-quality treatment for hyperhidrosis patients. This method is straightforward and has long-term efficacy and promising results, especially in certain areas such as palmoplantar regions. However, there is not sufficient information about the procedure of the treatment. Botox injection shows great results in preventing hyperhidrosis. Patients are able to pursue their normal life for about 6 months after a single treatment session. However, this method is costly and invasive and may lead to temporary disabilities in injection sites and areas. Suction curettage surgery stands as the last choice of hyperhidrosis treatment. This method is mainly used in severe cases and needs surgeons with enough experience. However, in most cases, there are scar incidents and even, in some cases, infections. The use of laser waves, ultrasound, magnetic waves, and radiofrequency waves (45-50) is one of the most modern treatments for hyperhidrosis. Radiofrequency heat therapy is our solution between minimally invasive and surgical methods to treat hyperhidrosis in armpits. It has been shown that radiofrequency heat therapy can be an effective treatment option according to the patients’ satisfaction. However, the emerging methods have not been able to replace classical treatment methods.
| Treatment | General Hyperhidrosis | Axillary Hyperhidrosis | Head and Face Hyperhidrosis | Plantar Hyperhidrosis | Palmar Hyperhidrosis |
|---|---|---|---|---|---|
| Topical antiperspirants | Negative | Positive | Positive | Positive | Positive |
| Tap water iontophoresis | Negative | Negative | Negative | Positive | Positive |
| Botox injection | Negative | Positive | Positive | Positive | Positive |
| Oral anticholinergic drugs | Positive | Positive | Positive | Positive | Positive |
| Medical equipment such as radiofrequency, ultrasound, laser | Negative | Positive | Negative | Negative | Negative |
| Curettage | Negative | Positive | Negative | Negative | Negative |
| Sympathectomy surgery | Negative | Positive | Positive | Positive | Positive |