1. Background
In December 2019, China witnessed a massive outbreak of a highly contagious acute respiratory disease called coronavirus disease 2019 (COVID-19) (1), which has become a global public health crisis (2). The outbreak of COVID-19, especially around the world, has led to increased pressure on hospitals in general and intensive care units (ICUs) (3, 4). Despite the fact that ICUs are almost full under normal conditions, about one-tenth of patients with COVID-19 require some type of ventilatory support (invasive or non-invasive) in these units (5). The combination of increased workloads and reduced numbers of healthcare workers is likely to put severe pressure on the capacity to maintain essential healthcare services (6). The COVID-19 pandemic has left many countries with significant economic and health system challenges (7). Examples of this problem include the rural healthcare system in India, which was inadequate or unprepared to prevent the transmission of COVID-19, particularly in many heavily populated northern states of India due to a lack of physicians, hospital beds, and equipment. The COVID-19 pandemic poses a particular challenge due to a lack of testing services, a weak surveillance system, and, above all, poor medical care (8). Also, the COVID-19 pandemic is stressing the healthcare system in Africa (9).
Globally, the damage from COVID-19 is potentially reversible, so efforts to support patients must be continued. However, the acute course of illness can last days or even weeks, with bed occupancy often prolonged, resulting in severe shortages of ICU beds and ventilators (5). Interestingly, the COVID-19 pandemic has given way to increased participation in health-related activities at the domestic level of countries. This epidemic is considered an important moment in healthcare performance. The pandemic, as a security threat, affected policies and procedures related to the health and military domains (10). The direct and indirect role of the army in national responses such as COVID-19 increases the trust of society and stabilizes them as joint players in the field of health. In this regard, in one of the less privileged provinces in Iran, due to the high prevalence of COVID-19, the number of beds, treatment units, and healthcare workers was not adequate due to the high number of patients in that province. Therefore, the police medical force tried to help the country's health system by building a field hospital.
2. Innovation
In order to solve this critical shortage, the Police Organization, the Governor, and the University of Medical Sciences from that province collaborated to establish a 64-bed field hospital for patients with COVID-19, with two separate wards for male and female Outpatients. A COVID-19 Police Field Hospital managed respite and monitored beds for patients with COVID-19 who required the injection of the second and subsequent doses of Remdesivir drug. Patients with COVID-19 were immediately transported to the reference hospital by A-type ambulances if their clinical condition changed to an acute respiratory position.
3. Implementation
3.1. Site Assembly
A COVID-19 Police Field Hospital was launched on July 1, 2021, following the cooperation memorandum regarding the control of the outbreak of COVID-19 in the province. The planning team, led by the Provincial University of Medical Sciences, used local resources, including field hospital land, municipal agencies, and other bodies, to envision and scale a 64-bed light-structure hospital facility in the local center. In order to establish the hospital, the executive team followed up engineering works for ten days and around the clock. During this period of near-continuous construction, executive staff worked with the field hospital leadership team to transform the land into a field hospital, meeting standards of infection prevention and clinical care (Figure 1). The main concern was to provide oxygen for this type of patient with acute respiratory problems due to COVID-19. A 600-liter oxygen generator was prepared and installed to achieve this goal. Electricity generators and electrical installations were also used. Lists of drugs and medical equipment were created by focusing on the specific conditions of COVID-19 and using the guidelines of the emergency management units and the opinions of the experts of the vice president of treatment. In two wards, equipment such as beds, two intubation devices, emergency carts and items inside the trolley cupboards, mobile blood pressure, high-flow nasal cannula, pulse oximetry devices, medicine storage refrigerator, etc., were arranged.
In parallel with this issue, the most important item was the supply of healthcare workers such as general physicians and disease specialists, nurses, and emergency medicine, which needed to be called from other police hospitals from all over the country's provinces. For proper implementation of this matter, it was announced to the hospitals that, at first, volunteers were used, and then the available capacities were requested to cooperate in the work shifts set for this center. For every 5 beds, one nurse and emergency medicine were considered. In each shift, there was an anesthesiologist to manage patients with changing respiratory conditions. Also, one general physician, one internist and infectious disease specialist, and one anesthesiologist were deployed for each ward.
The location of the medical staff was also in the apartment units near the hospital building, which, in case of emergency, could immediately help the group on the clinical wards. Psychological experts were also considered for mental and emotional support for the medical staff and patients who were present continually. Also, the biomedical engineers invited to collaborate regularly checked the oxygen generator system and the electrical and ventilation routes. The diplomates in environmental health and public health were responsible for distributing covers, masks, and gloves among the personnel and cleaning the building, departments, routes, and disinfection. In addition, the support part was also responsible for preparing and distributing snack food for medical staff in each shift. In this regard, the nutritional needs were provided by the University of Medical Sciences of the province.
On the other hand, the HIS (Hospital Information System) and discharge system were located at the end of the hall, where the patients' files during admission and discharge were managed by insurance experts. Above all, during the injection and before discharge, the doctors and nurses gave training related to the received drug, its side effects and therapeutic effects, and breathing exercises. Another point was that every day, the nursing director of the provincial University of Medical Sciences interacted with me, and one of the clinical supervisors of the provincial university hospital was present during the shifts to follow up on the medical affairs. The statistics of the patients and their physical condition were reported daily to the University of Medical Sciences and the reference hospital. According to the decision of the Ministry of Health, medical affairs were free.
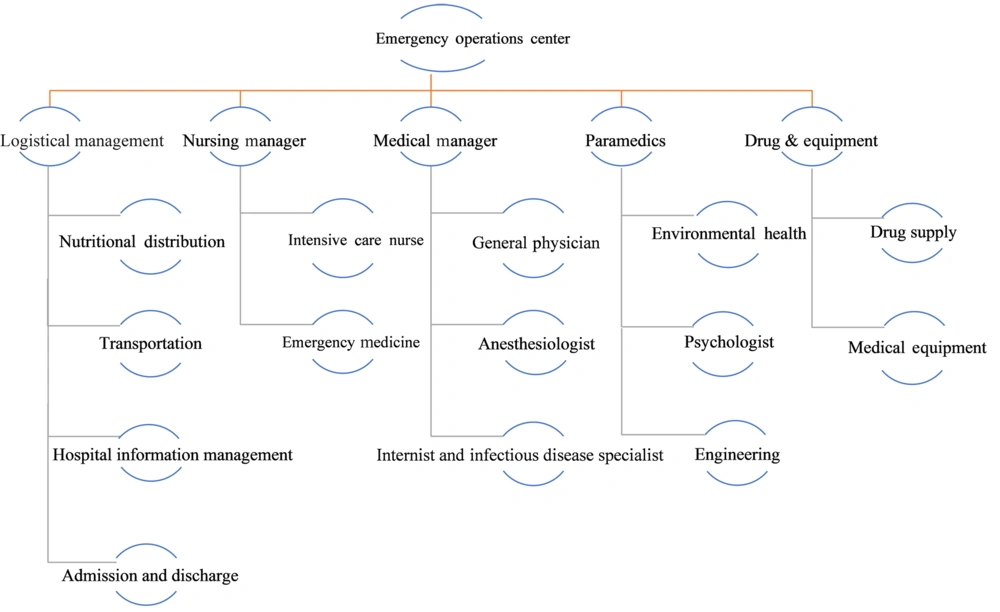
3.2. Organizational Structure of a COVID-19 Police Field Hospital
At first, it was considered an incident command system unit and was led by an incident commander, a military general, who was supported by the head of the university hospital of the province. For other main affairs such as clinical care, human resources, facilities/supplies, data management, and information technology, tasks, and structure were defined and included clinical teams and support and administrative services (Figure 2).
4. Results
About a thousand patients were admitted over eight weeks from July 12 to August 31, 2021. All patients were referred from University Hospital of the province. The initial admission was done by the university hospital, and the first round of Remdesivir injection was done in that center. Then, it was referred to the COVID-19 Police Field Hospital for the next round of injections. Admissions were later opened to emergency departments for cases of acute respiratory problems. The average length of stay was five hours; 65% of patients were male, the average age was 40-50 years, and 5% were 65 and older.
There was no intubation, cardiopulmonary arrest, or patient death. Six patients were transferred by ambulance to the university hospital due to the changing clinical conditions of the patients and some non-COVID issues such as chest pain and high blood pressure. All patients were discharged after receiving the drug injection dose and returned the next day to receive the next dose of the drug.
5. Discussion
This study pointed to the measures taken to eliminate the gap caused by the lack of facilities and healthcare workers in providing treatment plans to control the outbreak of this disease in less privileged provinces. The COVID-19 pandemic is an important moment in the contemporary presence of the military in global health (10).
There is limited literature to guide organizations and governments in order to structure and scale emergency facilities for patients in emergency situations, especially with COVID-19. In this regard, the existing experience showed that it is possible to quickly assemble and manage a field center for COVID-19 (11). This report provides guidance for others facing similar challenges. In emergency situations, cooperation between organizations and, in some cases, people and policymakers has a main role in controlling critical situations (12). Establishing a public health emergency operations center with the participation of local government, the military, and major healthcare organizations is necessary to support logistical and medical resources (13). It is worth mentioning that in response to the COVID-19 pandemic, the armed forces have mobilized in every country around the world. Current military assistance is driven by an urgent need for additional personnel and resources and is facilitated by framing the crisis in terms of war (14). This type of action by France shows that during COVID-19, eight French military teaching hospitals cooperated with civilian regional health agencies. The French military medical supply chain supported all military medical centers in France and abroad and dealt with the growing shortage of medical equipment. The Biomedical Research Institute of the French Armed Forces performed diagnostic procedures, participated in several research projects, updated the scientific literature review on COVID-19 daily, and provided expert advice on biosafety. Eventually, even students from the French Military Medical Academy volunteered to participate in the fight against the COVID-19 pandemic. As a result, in an unprecedented medical crisis, the French military medical service took several innovative and adaptive measures in the fight against COVID-19, which are still ongoing (15).
Gibson-Fall has proposed in the study that by imposing restrictive measures and putting pressure on health systems, military deployment has been revealed through three clear trends of engagement: (1) minimal military-technical support, (2) blended civilian-military responses, and (3) military-led responses (10).
Therefore, the government, the Ministry of Health, the military forces, non-governmental organizations, and other voluntary support should make the necessary preparations in the health and treatment centers and improve the infrastructure (1).
5.1. Conclusions
In emergency situations and lack of facilities in specialized medical personnel, beds, and medical equipment, the construction of field hospitals will reduce the burden on countries' medical systems. On the other hand, maintaining the power dynamics of the army continues through cooperation with various institutions, including the wide field of treatment, which also follows the military's political legacy. Collaboration between the military and civilian healthcare systems fosters the common goal of achieving the goal of "Saving the Greatest."