1. Background
The coronavirus disease-19 (COVID-19) pandemic has significantly affected various sectors, especially the healthcare systems in all over the world (1). Indonesia is the largest archipelago with the fourth largest population in the world. Despite its size and diversity, the country shares several features with other densely population such as India, Brazil and the United States which are known to have been severely impacted by the COVID-19 pandemic (1). Insufficient number of medical personnels, fragile medical supply chain, inadequate of health infrastructure to deal with increasing cases of COVID-19 were serious problems faced by health services in Indonesia. In addition, the optimal of patient referral system and the suboptimally limited capacity of the health care system to provide essential health services in prolonged emergency conditions has an impact on reducing the quality of services for non-COVID cases such as patients with chronic disease (2).
Down syndrome ( DS) is a chronic disease known to be due to trisomy of chromosome 21 that is associated with risk for recurrent infections, autoimmune diseases, and inflammatory conditions (3), as a result of immune dysregulation (4). Chromosome 21 in DS patients saves many genes involved in immune response regulation, and its over-expression causes an overactive immune system due to chronic interferon hyperactivity even in the absence of infection (5). Severe COVID-19 can result in an uncontrollable immune response and multi-organ failure (6), making individuals with trisomy 21 at relatively high risk for more severe symptoms, increased hospitalization, and even death (4). In spite of the emergency risks faced by children with DS, they are also have increased risk of developing thyroid disease, especially autoimmune thyroid disease (AITD) which has the most common manifestation as Hashimoto's thyroiditis/autoimmune hypothyroidism. Hypothyroidism is a treatable cause of mental retardation. There for, the lack of appropriate treatment deepens the children’s retardation as well as affecting their growth process in this already impaired population (7). Adequate management of patients with thyroid diseases remains essential during the pandemic, but it could be compromised because of healthcare service restrictions (8).
Medication adherence is defined as the degree to which the person’s behavior corresponds with the agreed recommendations from a health care provider. Rate of adherence is usually reported as the percentage of the prescribed doses of the medication actually taken by the patient over a specified period. Complexity of adherence is the result of an interplay of a range of factors including patient views and attributes, illness characteristics, social contexts, access and service issues. Barriers to the effective use of medicines specifically include poor provider-patient communication, inadequate knowledge about a drug and its use, not being convinced of the need for treatment, fear of adverse effects of the drug, long term drug regimens, complex regimens that require numerous medications with varying dosing schedules, cost and access barriers (9). During the COVID-19 pandemic, there were extraordinary changes that impacted the health care system, one of which was the lack of availability or accessibility of drugs, which disrupted medication adherence for many chronic diseases patients who require repeat visits, follow-up, examination, refilling of prescriptions and access to health facilities had difficulty visiting the hospital and obtaining medicines, which puts them at risk of exacerbating the course of their disease (10-12). Several studies conducted on various cases of chronic disease in several countries have shown different results of medication adherence during the COVID-19 pandemic. Study in Type 1 diabetes mellitus (T1DM) reported missed in insulin dose and glucose monitoring not done routinely during lockdown (11), a meta-analysis study of epilepsy as other chronic disease reported inadequate adherence to anti-seizure medication during the COVID-19 pandemic in Italy and Saudi, while study in Turkey reported the COVID-19 pandemic made patients more motivated and informed about drug compliance (13).
The consequences of non-adherence are drug wastage, disease progression, reduced functional ability, lower quality of life, increased use of medical resources such as hospital visits and hospitalizations (9). Economic studies reveal that non-compliance with prescribed regimens can result in serious health consequences including the risk of hospitalization increasing more than two times compared to the general population, increased emergency department visits with severe complications which have an impact on higher health financing (14). To our knowledge, there has been no study that examined medication adherence in children with chronic disease in Indonesia during the COVID-19 pandemic as an as an archipelagic country with limited drug availability and travel barriers experienced by patients and their families.
2. Objectives
This study aims to evaluate medication adherence in Indonesian Down Syndrome children with AITD during the COVID-19 Pandemic and explore several causative factors.
3. Methods
3.1. Sample and Study Designs
An observational analytic study was conducted at tertiary referral teaching Dr. Soetomo Surabaya Hospital from January to July 2021. During that period, Indonesia currently undergoing the first wave of COVID-19. Local transportation and interdistrict/interstate communication are not allowed during the entire period. Consecutive sampling was performed from parents of DS with AITD patients enrolled in a pediatric endocrinology outpatient clinic. We contacted the telephone number recorded in the medical record and invited them to an online educational activity that contains about their illness and the importance of continuing treatment during the COVID-19 pandemic. Inclusion criteria were: (1) parents of DS patients who already diagsoned as AITD aged 1 - 18 years, (2) patients taking the oral medication for thyroid function (levothyroxine for patients with hypothyroidism and vitamin D for patients with euthyroidism) and regularly visit to our hospital before January 2020, (3) parents could fill out questionnaire forms independently and signed informed consent for participants. The exclusion criteria included parents of DS patients who did not take medicine and those who received treatment after the pandemic was declared in Indonesia (March 2020). The sample size was calculated using the ‘sample calculation formula’ for an observational analytic study (15). This study was conducted in accordance with the Declaration of Helsinki and was approved by the ethical committee of Dr Soetomo General Hospital, Surabaya Indonesia (Ref. No. 1960/KEKP/IV/2020).
3.2. Data Collection Tools
The data collection technique was carried out by filling out the on line questionnaires after education on line session. Informed consent was given before respondents answered the questionnaire. Respondents who did not fill out the questionnaire on that day were followed up regularly to fill out the questionnaire up to a maximum of 1 month after the online education session was held.
A self assessment questionnaire was administered consisting of (1) demographic and clinical data including patient age, gender, co-morbidity, regular treatment/daily doses, and duration of taking regular medication, parent’s occupation, parent’s educational background and salary per month, and distance traveled to the hospital which were extracted from the interview and medical record. (2) Questions regarding barriers to hospital visit and barriers to medication adherence during the pandemic were developed (Appendix 1 in Supplementary File). At our hospital, each patient will receive a statement regarding the next visit control schedule. According to the condition of the DS patient with AITD, the patient can be scheduled for routine control every 1 month or every 3 months. A patient is defined as compliant if he comes in the same month as scheduled. It is said to be disobedient if he comes in a different month. We define non-adherence if the patient misses a dose in ≥ 2 consecutive days or misses a dose in 1 day without adding an extra dose the next day (16).
Each question in the barrier of regular visit and medication adherence during pandemic was developed based on literature research. Unintentional non-adherence arises from capacity and resource constraints that prevent patients from implementing their decisions to follow treatment recommendations (eg problems accessing prescriptions, costs, competing demands) and sometimes involves individual constraints. While intentional non-adherence arises from beliefs, attitudes and expectations that affect the patient's motivation to start and stay with the treatment regimen (9, 17). Each question has been tested on 10 patients with other diagnoses in our clinic as a preliminary study and tested for validity and reliability.
3.3. Analysis of Data
Descriptive analysis was conducted to describe the demographic, clinical data and also detail the barriers to hospital visit and barriers to medication adherence during the pandemic. Statistical analysis using the Wilcoxon comparison test was performed to obtain the difference between adherence on regular visit and medication adherence before and during pandemic, with P < 0.05 considered as statistically significant. Statistical analysis was performed using Statistical Package for the Social Sciences version 17.0.
4. Results
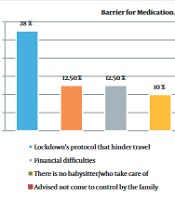
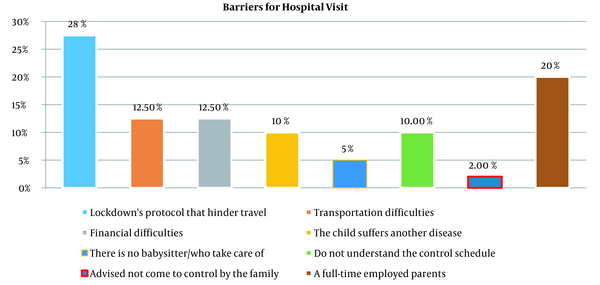
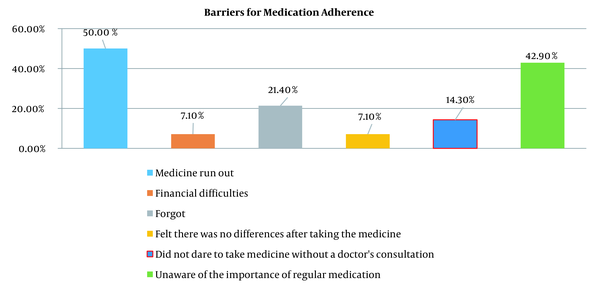
Based on data recorded in medical records, we have a total of 42 DS patients with AITD in 2020. Unfortunately 3 patients died during the pandemic. Of the remaining 39 patients, there were 31 respondents (80%) who filled out the questionnaire completely. Table 1 describes the baseline characteristics of the sample. The mean duration of mediation was 11.84 ± 17.69 months with the majority (51.8%) of patients taking 1 drug per day. The adherence to hospital visits was significantly higher before the COVID-19 pandemic compared with during the COVID-19 pandemic (P = 0.001), as seen in Table 2. There was no significant difference in the compliance for taking medication before and during the pandemic, but there were 18/31 (58.0%) patients who received non-prescription drugs from our clinic, the majority (41.9%) bought the drugs themselves. The most common hindrance faced by patients during the pandemic for a follow‑up visit and taking medicine was the lockdown restrictions (28%) and medicine running out (50%), respectively.
| Parameters | No. (%) or Mean ± SD (n = 31) |
|---|---|
| Age | 40.97 ± 32.64 |
| Sex | |
| Male | 18 (58.1) |
| Female | 13 (41.9) |
| Mother’s education | |
| Diploma/graduate | 12 (38.7) |
| High school | 17(54.8) |
| Middle school | 1 (3.2) |
| Primary school middle school | 1 (3.2) |
| Parent’s income | |
| < 4,000,000 IDR | 16 (51.6) |
| ≥ 4,000,000 IDR | 15 (48.4) |
| Distance traveled to the hospital, km | |
| < 51 | 16 (51.6) |
| ≥ 51 | 15 (48.4) |
| Duration of oral medication, mo | 11.84 ± 17.69 |
| The number of drugs that are routinely taken each day | |
| One drug | 18 (58) |
| Two drugs | 12 (38.8) |
| Three drugs or more | 1 (3.2) |
| Congenital disease | |
| Yes | 13 (41.9) |
| No | 18 (58.1) |
| Thyroid dysfunction | |
| Yes | 29 (93.5) |
| No | 2 (6.5) |
| Thyroid autoimmune parameters, IU/mL | |
| Thyroid peroxidase antibody (TPO-Ab) | 594.68 ± 1565.074 |
| Thyroglobulin antibody (Tg-Ab) | 2036.93 ± 2031.394 |
Demographic and Clinical Charateristics of the Study Participants
| Parameters | Respons to Questioner | P-Value | |
|---|---|---|---|
| Yes, (No. %) | No, (No. %) | ||
| Adherence to hospital visit | 0.001 a | ||
| Pre COVID-19 | 22 (70.97) | 10 (32.26) | |
| During COVID-19 | 9 (29.03) | 21 (67.74) | |
| Compliance for taking medication | 0.544 | ||
| Pre COVID-19 | 22 (71.0) | 9 (29.0) | |
| During COVID-19 | 25 (80.6) | 6 (19.4) | |
| How to get medicine during the COVID-19 pandemic | 0.045 a | ||
| Buy them themselves | 13 (41.9) | 18 (58.1) | |
| Presciption from doctor in another hospital | 5 (16.1) | 26 (83.9) | |
| Presciption from doctor in dr Soetomo hospital | 13 (41.9) | 18 (58.1) | |
Participant’s Response to the Questionnaire
5. Discussion
This study was conducted to identify the challenges of lockdown during COVID-19 and considering the importance of continuity of care in DS patients. The majority of patients in this study did not adhere to the medication control schedule and showed a significant difference in hospital visit compliance before and during the COVID-19 pandemic. This result is in line with other studies that showed the number of outpatient visits decreased during the COVID-19 pandemic (18, 19). Poor adherence is associated with increased emergency room visits, hospitalizations, and suboptimal clinical outcomes, leading to an increased burden on the health care system. During the pandemic, the decrease in routine visits is important factors that must be considered (20). We have data on 3 patients who died during the COVID-19 pandemic, which, although not shown to be directly associated with reduced adherence to treatment, is consistent with the results of other chronic disease studies showing increased morbidity and mortality of chronic disease patients over this period (11, 21).
In this study, the main reason for not visiting the hospital was the lockdown restrictions (28%), which led them forgetting about the routine follow-up visit to the doctor. In addition, 15 (48.4%) patients in this study had to travel ≥ 51 km for a hospital visit, thus making follow-up visits more difficult during lockdown restrictions. Many governments have had to make difficult decisions to protect their citizens in the face of the current pandemic, including lockdowns and restrictions on people’s movements. Because of the lockdown policy and the relocation of medical workers to the frontlines of the COVID-19 pandemic, 44% of patients with chronic conditions who require revisits, follow-ups, and medication refills may face difficulties due to limited access to health facilities and attending physicians. Furthermore, due to the increased risk of infection in hospitals, the majority of people avoid consulting their doctors (22, 23).
The second reason for the lack of adherence to visiting hospital is full-time employed parents (20%). Lockdown protocol, which also makes schools and workplace closed, has forced many parents to do their work at home while also taking care of their children. This situation can be stressful for some of them and make them busier during this pandemic (24). Parents of children with special needs face additional challenges compared to other parents. They must look after their children, particularly the DS patients, whose behavior and emotions can be unpredictable. Taking care of their children, doing housework, and having to complete office work can be very demanding, thus making the parents busier and creating stressful situations. Mothers who have children with special needs are more likely to experience stress. When parents are busy, a lack of social awareness and support may cause the family to struggle to understand the children and, as a result, impede treatment planning (25).
Our study has also identified financial difficulties (12.50%) as a factor that can only worsen the patient’s difficulty in visiting the hospital. Financial difficulties can prevent patients from receiving medicines, as up to 50% of respondents earned less than the minimum wage. Another study discovered that financial constraints have an impact on medication adherence and follow-up (26, 27). Most of the medical expenses for DS patients with AITD are covered by state insurance, but transportation costs have swelled due to the absence of public transport during the lockdown and the loss of livelihoods for some parents due to the pandemic are aggravating financial factors that make them not routinely take their children to visit the hospital.
In this study, non-adherence of hospital visit during pandemic was arises from capacity and resource constraints such as lock down, combined with individual constraints such as a full time employee and financial difficulty which is apart of un-intentional adherence (9). Recent studies indicate that unintentional nonadherence is significantly affected by beliefs about illness and medication or self-efficacy (28). There for, education about the disease and the importance of treatment is an important thing that must be done to increase adherence to hospital visits, in addition to bringing services closer to the patient's residence during the pandemic.
Our study found no difference between the compliance for taking medication before and during pandemic. This result in line with study in Turkey that reported during COVID-19 pandemic, patients more motivated and informed about drug compliance (13). The interesting thing is when this data is combined with how parents get routine medicines for their children, then there is approximately 41.9% of patients obtained their own medication during the pandemic. Self-medication (SM) as the selection and use of medicinal products by consumers to treat a self-recognized disease or the intermittent or continuous use of drugs prescribed by a doctor for chronic or recurrent disease (29). The prevalence of SM is increasing sharply throughout the world, where the prevalence of self-medication in developing countries ranges from 12.7% to 95% (30). SM is one of the major contributors to making essential medicines accessible and affordable in developing countries. However, if not used as intended, it can lead to serious problems such as drug toxicity, drug interactions, drug dependence, microbial resistance and wasted medical resources.29 Unfortunately there has been a marked increase in self-medications without prescription during the pandemic (31).
Drugs running out during the onslaught of the COVID-19 pandemic has been determined as one of the main barriers in our study for patients to get regular therapy. The use of medicines prioritized for COVID-19 patients caused the supply of medicines for chronic diseases to dwindle; additionally, drug manufacturing companies were busy attempting to produce medicines and equipment aimed at dealing with COVID-19; moreover, the supply of imported medicines was also prioritized for COVID-19 patients, so essential medicines were not available or difficult to obtain for people with chronic diseases (23). The existence of travel restrictions that cause border closures, restrictions on trade between countries, and transportation problems have resulted in the disruption of national and international supply chain systems, including the supply of medicines (32). This data serves as a lesson for us that in the event of a pandemic, the availability of drugs for chronic cases cannot be secondary, because a break in the drug supply chain that causes patients to stop taking regular medication will become a big time bomb with an explosion of chronic cases that were neglected during the pandemic COVID-19.
The factors that contribute to poor medication adherence are numerous, not only those related to the health care system, but also those related to physicians (e.g., prescribing complex drug regimens, communication barriers, ineffective communication of information about side effects, and provision of care by multiple people), no less important are patient-related issues (e.g., suboptimal health literacy and lack of involvement in the treatment decision-making process) (33). Our study showed 42.9% of patients expressed ignorance about the importance of medication and 21.4% cited forgetting as a reason for not taking medication regularly. This data reflects the low knowledge of parents about their child's illness. In addition, only 38.7% of our respondents received education up to college. This is in accordance with other studies which show the higher the level of education, the better is the patient's knowledge about their medication (34).
The DS patients in this study had comorbidities, namely AITD, with the majority having thyroid dysfunction (93.5%). In addition, 41.9% of patients have congenital diseases that require strict medication adherence and continuous monitoring. As a result, the inability to do so will increase the risk of mortality and morbidity (35). The pandemic has exposed the fragility of the medical supply chain, the weakness of patient referral systems, and the health care system's limited capacity to deliver essential health services in protracted emergencies. Various strategies to overcome these mounting challenges must be developed to increase the capacity of health services. As an archipelagic country, Indonesia has major obstacles in accessing tertiary health services. By optimizing the role of general practitioners in public health centers spread throughout Indonesia, cases that require tertiary services can be served through tiered referrals so that patients can be served and educated every month by general practitioners who have been supervised and will come to the tertiary hospital in 3 - 6 months to get subspecialty treatment. This system also needs to be considered to facilitate the provision of drugs and evaluation laboratory services needed in determining the next dose. Shifting medication counseling to the nearest primary health care provider with supervision from a tertiary referral specialist appears to be a reasonable and potentially cost-effective strategy in improving treatment adherence especially in a pandemic setting (36). This will provide an opportunity for patients and families to not self-administer their medication and they will benefit from different types of support by healthcare professionals (37). Services for patients can also be brought closer through virtual visits (telemedicine). Although not applicable in all areas, this concept can be applied in urban areas in Indonesia with sufficient internet access and adequate transportation support for drugs and laboratory tests in these areas. The use of tele-health and digital health platforms has increased during the COVID-19 pandemic due to the implementation of physical distancing measures and restrictions. However, we must also be aware of the limitations faced by telemedicine services such as quality of care in terms of patient involvement, empathy, and emotional and human considerations, as well as concerns about practical safety and clinical, and security of medical data (38).
This study provides data on medication adherence during a pandemic and identifies various barriers experienced by patients. Existing data can be used as material for consideration in taking steps to improve the health system during the COVID-19 pandemic in Indonesia. Particular attention should be paid to the importance of storing chronic patient information within the health system, and the importance of tracking disease complications during the COVID-19 pandemic. In addition, training on the health care is important for preparing for a crisis situation like a war or invasion. The limitations of this study were limited number of samples due to very specific cases, and a single-centered study. Conducting a multi-center study to collect more data in another center in Indonesia during the COVID-19 pandemic will be beneficial.
5.1. Conclusions
The COVID-19 pandemic has crippled healthcare services around the world. There was a change in hospital visit and medication adherence during the COVID-19 pandemic, as has been determined in this study. Lockdown regulations and travel restrictions causing limiting medicine availability and raising the risk of morbidity and mortality among children with DS. During the COVID-19 pandemic, parents’ efforts to improve medication adherence by purchasing medicine without a prescription highlighted the need to increase the accessibility of medical care for DS patients. The health service approach strategy through a tiered referral system and telemedicine needs to be implemented carefully by considering all available resources in all regions in Indonesia which have different characteristics. Furthermore, training in health care is important in preparation for an emergency condition such as war or invasion, an emergency condition that might be experienced by the health system in Indonesia apart from the COVID-19 pandemic.