1. Background
With an estimated birth incidence of 9.4%, congenital heart defects (CHDs) rank among the most prevalent birth disorders globally (1). These disorders remain the leading cause of disability and mortality in neonates and children, resulting in significant physical and mental comorbidities that heavily burden families and society (2). The etiology of CHDs is identifiable in approximately 15% of cases, with factors such as maternal diabetes mellitus, genetic predispositions, poor nutrition, certain medications, and obesity playing a role (3). The pathophysiology of most CHDs is greatly influenced by the interplay between environmental and genetic factors, especially modifiable aspects of maternal lifestyle and diet (4, 5).
Animal studies suggest that cardiac abnormalities in newborns may be associated with zinc deficiency during pregnancy (6). However, human studies on serum zinc levels in these patients have produced inconsistent results. One study found no association between zinc levels and CHDs (4), while another showed an inverse relationship between serum zinc levels and the occurrence of ventricular septal defects (VSD) (7). Another piece of research indicated that patients with CHD had higher zinc levels compared to healthy controls (8).
Conversely, studies indicate that a deficiency in maternal vitamin D levels is associated with an increased incidence of CHDs in offspring (9). In the general population, vitamin D deficiency is linked to a heightened risk of cardiovascular events and is associated with increased cardiovascular morbidity and mortality (10). Moreover, in individuals with CHD, occurrences of secondary hyperparathyroidism and vitamin D deficiency have been noted (8, 11). Thus, it can be argued that hypoxemia, cyanosis, and the use of certain medications for CHD may impact the kinetics of vitamin D and the functioning of the parathyroid gland (11-13).
2. Objectives
The current study aims to assess the serum levels of vitamin D and zinc in children with CHD and compare them with those in a control group.
3. Methods
3.1. Participants and Study Design
This case-control study included children with CHD who were admitted to the Children's Hospital in Bandar Abbas in 2018, from June 22 to December 21. The inclusion criteria were an age range of one month to 14 years and echocardiography-confirmed CHD. A control group of children without CHD was also evaluated. The sample size of this study was set at 25 patients for each group, based on serum vitamin D levels estimated from the study by Noori et al. (22). The sample size calculation used a type I error rate of 0.05 and a power of 90%.
The Ethics Committee of Hormozgan University of Medical Sciences approved this study under the ethics code IR.HUMS.REC.1397.018, in accordance with the principles of the Declaration of Helsinki. Parents or guardians of the participating children provided written informed consent for their children’s participation and for the publication of the study data.
After recording the demographic variables of the participants, 4cc of blood was drawn from each child to measure serum levels of vitamin D and zinc. Serum 25-hydroxy vitamin D levels were assessed using the chemiluminescence method (Abbot Architect i1000SR, USA), and serum zinc levels were measured using the absorption method with a standard photometer. Vitamin D levels between 20 to 30 ng/mL were considered insufficient, and levels less than 20 ng/mL were considered deficient. Zinc levels below 70 mcg/dL were categorized as zinc deficiency. Additionally, patients with CHD were classified into cyanotic and non-cyanotic groups.
3.2. Data Analysis
The data were analyzed using Stata software (version 14.2). Continuous quantitative variables were described using means and standard deviations, while qualitative variables were categorized by frequency and percentage. Independent t-tests were utilized to compare continuous variables between the two groups, with this approach being justified by the central limit theorem (14). Moreover, Cohen’s d was employed to calculate the standardized mean difference (SMD), with interpretations as follows: Less than 0.19 was considered trivial; between 0.20 to 0.49, a small effect; between 0.50 to 0.79, a medium effect; and more than 0.80, a large effect (15). The chi-squared test was used to compare categorical data between the two groups. Effect sizes for a 50% CHD prevalence were reported as odds ratios (ORs), with interpretations ranging from 0 - 1.48 for a trivial effect, 1.49 to 3.44 for a small effect, 3.45 to 8.99 for a medium effect, and more than 9.00 for a large effect (16). The significance level was set at P-values ≤ 0.05.
4. Results
Overall, the study assessed 106 children, with each group—CHD and controls-comprising 53 participants. Among the children with CHD, 43 (81.1%) had non-cyanotic and 10 (18.9%) had cyanotic conditions. Table 1 displays the general characteristics of the study groups.
| Variables | Congenital Heart Defect (n = 53) | Control (n = 53) |
|---|---|---|
| Age | ||
| 1 month - 1 year | 26 (49.1) | 24 (45.3) |
| 1 - 5 year | 23 (34.4) | 25 (47.2) |
| 6 - 14 year | 4 (7.5) | 4 (7.5) |
| Sex | ||
| Male | 31 (58.5) | 22 (41.5) |
| Female | 22 (41.5) | 31 (58.5) |
a Values are expressed as No. (%).
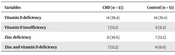
The statistical analysis revealed no significant differences in the serum vitamin D levels between the groups (P = 0.242). Conversely, the serum zinc levels were significantly lower in children with CHD compared to the controls, showing a medium effect (SMD = -0.67, 95% confidence interval [CI] -1.06 to -0.28) (Table 2). Regarding the frequency of vitamin D deficiency and insufficiency, both groups were similar (P = 1.000 and P = 0.767, respectively). However, the likelihood of zinc deficiency was 4.31 times higher in children with CHD than in the controls (OR = 4.31, 95% CI 1.52 to 13.31) (Table 3).
Abbreviations: CHD, congenital heart defect; SMD, standardized mean difference.
a All values are adjusted means (95% CI) in adjusted models and means (95% CI) in crude models and expressed as mean (standard deviation).
b Calculated using Cohen’s d.
c Analyzed by the independent t-test.
| Variables | CHD (n = 53) | Control (n = 53) | OR (95% CI) | P-Value b |
|---|---|---|---|---|
| Vitamin D deficiency | 14 (26.4) | 14 (26.4) | 1.00 (0.39; 2.60) | 1.000 |
| Vitamin D insufficiency | 7 (13.2) | 6 (11.3) | 1.000 1.19 (0.32; 4.64) | 0.767 |
| Zinc deficiency | 21 (39.6) | 7 (13.2) | 0.767 4.31 (1.52; 13.31) | 0.002 |
| Zinc and vitamin D deficiency | 7 (13.2) | 0 (0.0) | - | 0.006 |
Abbreviations: CHD, congenital heart defect; OR, odds ratio; CI, confidence interval.
a Values are expressed as No. (%).
b Analyzed by the chi-squared test.
5. Discussion
This study aimed to compare serum levels of vitamin D and zinc in children with CHD against those of a control group. We found that the serum zinc levels were significantly lower in the CHD group, exhibiting a medium effect. Similarly, Yalçin et al. investigated the blood and tooth content profiles in children with CHD, finding that zinc levels were lower in patients, though not to a statistically significant degree (17). Sadoh and Sadoh reported comparable outcomes, noting lower, albeit not statistically significant, serum zinc levels in children with CHD (18). The disparity between these studies and our own may be due to the smaller sample sizes used in their research. Additionally, other factors, such as the nutritional status of the children with CHD and their medications—especially diuretics used for treating congestive heart failure-could affect serum zinc levels (18). Our study did not examine these potential influencing factors.
Thus, zinc deficiency in children increases the likelihood of CHD compared to those with adequate serum zinc levels. Similarly, Zhu et al. observed zinc deficiency in children with isolated VSDs (7). Zinc is known to be a crucial component of proteins and plays a significant role in cell signaling due to its coordination geometry's flexibility and its ability to rapidly change protein shapes required for biological interactions (19). Key targets of zinc include various proteins involved in signaling pathways, ion channels, and mitochondrial metabolism, all vital for regulating cardiac contractility (20). Juriol et al. noted that a lack of zinc could alter the heart's inflammatory, apoptotic, oxidative, and nitric oxide pathways. Zinc deficiency has been shown to increase inflammatory and apoptotic processes in the heart tissue while reducing the expression of transforming growth factor β1 and the activity of nitric oxide synthase (21).
Despite observing lower, albeit not statistically significant, levels of 25-hydroxy vitamin D in children with CHD, this study found no difference in the prevalence of vitamin D deficiency and insufficiency between children with CHD and controls. In contrast, Noori et al. reported significantly lower serum levels of vitamin D in children with CHD compared to controls (22). The presence of 25-hydroxy vitamin D receptors in the heart's endothelium, smooth muscle, and myocytes supports the hypothesis that 25-hydroxy vitamin D may be beneficial in cardiovascular disease (23). The diminished function of this receptor in cardiac cells can lead to diastolic disturbances and, ultimately, cardiovascular complications (24). Furthermore, recent studies have suggested that various aspects of the vitamin D pathway are involved in cardiogenesis (25, 26). In parallel, a study by Rahayuningsih et al. showed that serum vitamin D levels were associated with heart failure, the types and severity of VSDs, and pulmonary hypertension in children with VSD (27). Additionally, Koster et al. found a twofold increase in the incidence of CHD in children born to mothers with low levels of vitamin D (9).
This study has some limitations, including the cross-sectional design does not allow for the determination of causality between CHD and deficiencies in zinc or vitamin D, although the odds ratios reported here may overestimate the associations. Furthermore, the relatively small sample size, despite being larger than that of most previous studies, limits the generalizability of our findings. As a result, we could not evaluate the potential effects of age, sex, and CHD type.
5.1. Conclusions
In this study, children with CHD had significantly lower levels of zinc compared to controls, while no significant differences were observed between individuals diagnosed with coronary heart disease (CHD) and the control group regarding vitamin D deficiency or insufficiency. However, it is crucial to conduct larger longitudinal studies to confirm these findings and assess the causality between serum levels of vitamin D and zinc in children with CHD.