1. Background
Preventing errors and patients’ safety in transfusion medicine have been serious problems (1). Although there are systems for checking the quality as well as electronic information processing machines, near-miss transfusion events are certain concerns in blood transfusion medicine, which are threatening for patients’ lives and impose a remarkable cost on the health care system (1). Transfusion errors occur at five phases: wrist‐banding of the patient, collecting samples, laboratory assessment, blood products issuing, and transfusion time (2).
Over 650,000 patients annually are affected by one of such preventable errors resulting in needless pain, trauma, and even death (3). According to statistics from the Joint Commission on Accreditation of Healthcare Organization (JCAHO), blood transfusion errors (2.9%) were priority adverse events in all hospital departments in America in 2008 (4). Also, recent reports on serious hazards of transfusion (SHOT) estimated a frequency of incorrect blood component transfusion as high as 70% of total transfusion errors (5). In addition, according to annual reports, more than 13 million units of blood are collected and injected into 4 million patients; 10% of these people may be affected by complications of blood transfusion (6) Also, according to Pahuja et al., the incidence rate of immediate blood transfusion complications in one hospital in India from 2005 to 2013 was reported to be 0.19% (7). In addition, according to Karim et al., the incidence rate of blood transfusion complications in one hospital in the south of Pakistan from 2012-2016, was reported as 1.16 per 1000 blood products (8).
In February 2018, the Accreditation Organization of Iran, in accordance with the National Quality Forum Committee, has developed the “Never Events” framework for immediate investigating and reporting for detecting as well as root cause analysis (RCA) of these incidents. Life-threatening adverse events in the treatment of patients in Iran are classified into 28 categories, one of which (item 14) is related to death or severe disability relevant to hemolytic reaction as a result of quite incompatible blood or blood products. Based on this system, in case one of these occurs, hospitals should report the incident within 24 hours by fax to the vice-chancellor’s office for treatment of the university. Besides, the vice-chancellor of the university is obliged to investigate the issue within the maximum period of 24 hours and upload it to never event system of the Ministry of Health and Medical Education (9). For obtaining their goals, identifying the risks as well as implementing plans for managing such risk factors are needed to be done by organizations (10). Several strategies have been suggested for clinical risk management for ensuring the health care service quality and safety of the patients, of which RCA is a valid method. It is effective to analyze the system failures and find potential solutions to eliminate and/or reduce the errors (11). In the process of RCA of the events, we are not looking for putting the blame on those making the error but also identification and correction of the likelihood of similar adverse events through the therapy and healthcare organizations are considered (12).
In general, one of the priority programs in the field of medical treatment at the medical universities of Iran from 2017-2018 was to improve the reporting system of vital life events of the patients (13). Moreover, RCA has been shown as a structured method for risk assessment and decrease and it has been confirmed as a central approach used in learning from errors and in risk reduction (14). On the other hand, blood transfusion and the control of its complications have always been a cause for concern for blood transfusion centers; and the blood transfusion organizations have always attempted to reduce these complications and manage patients’ blood (15).
2. Objectives
The present research aimed at evaluating the RCA of the adverse events relevant to blood transfusion reported by one of the major vice-chancellor’s offices of the university of medical sciences in Iran, in spring 2018.
3. Methods
This research was done according to the retrospective-qualitative method via achieving the benefits of RCA approach. The study protocol was approved by the Research Ethics Committee of Shahid Beheshti University of Medical sciences. Prior to the study, written informed consent was obtained from the patients or parents of patients.
This research follows the eight following phases introduced for RCA of the healthcare events by the National Authority for Health (16). It showed be noted that some modifications were considered to implement the eight-stage model.
1- Defining the Sentinel Events:
In this phase, a short explanation, the type, time, impact, and severity of adverse events related to blood transfusion were explained.
2- Selecting a Multidisciplinary Team to Perform RCA:
The permanent members of the vice-chancellors for treatment, after receiving the immediate report, attended the place of occurrence within 24 hours and examined all clinical and non-clinical documentation of the patient, and conducted interviews with people involved in the incident.
3- Gathering Information:
In this phase, following group discussion meetings, semi-structured interviews with the affected people, evaluating the patient’s documents, as well as collecting other related files, and observation of the event scene, data associated with the incident were gathered. Next, narrative chronology and timeline or table timeline related to the sentinel incidents were organized by the RCA team.
4- Identifying Problems:
In this stage, the defect and the deficiency available through the service delivery process were accurately classified into two main classes, including care delivery problems and service delivery problems. They were categorized according to the “classifying nursing errors in clinical management (NECM)” approach (17). through group discussion meetings and semi-structured interviews.
5- Identifying Causal Factors:
In this stage, factors that influence the performance and lead to the delivery of unsafe services, resulting in the occurrence of an incident or an event were classified into two general sets of influential factors and causal factors by taking advantage of cause and effect analysis sessions and via copying the lead of the approved model by the UK national health system.
6- Identifying Solutions:
In this phase, enhancement solutions to omit/ reduce the mistake’s concerns and reasons were presented in team meetings by “an innovative problem-solving theory” (18). followed by classifying based on the suggested pattern “classification of the medical errors preventive strategies” (19, 20)
7- Prioritizing and Implementing Solutions:
In this phase, according to the results of the study, the instructions for the management of blood transfusion blood products were formulated by the experts’ recommendations in team meetings.
4. Results
Table 1 reports the narrative description of adverse events relevant to incompatible blood and blood transfusion and issues relevant to care or service.
| Brief Description | Problems Related to Service Delivery Problems(SDP) | Problems Related to Care Delivery Problems(CDP |
|---|---|---|
| For a 34-year-old woman, the anesthesiologist used the previous patient’s medical record for blood transfusion, and the transfusion of 2 units of packed cells with A+ blood type was mistakenly applied for the patient with O+ blood type, and subsequently, it resulted in hematuria, and the patient was kept under intensive care. | Inadequate management in sending the medical record | The patient’s identification wristband had not been checked |
| Error in the delivery | ||
| Inadequate management in the implementation of surgical safety by the treatment staff | ||
| Inadequate provision of safe care | ||
| A 58-year-old patient was hospitalized because of hematuria. Packed cell with A+ blood type injected to the patient with O+ blood type by a nurse with 3 years of clinical experience in nephrology. | Deficiency in implementation of safe systems regarding the maintenance and surveillance | The patient’s identification wristband had not been checked |
| A 24-year-old patient who identified with thalassemia, without the nurse’s permission, took another patient’s blood bag from the refrigerator mistakenly and injected himself. | Lack of medical records for outpatients | The nursing team had no control over the treatment room |
| Deficiency in implementation of safe environment standards |
Narrative Description of Adverse Events and Distribution of delivery problem to Care or Service
Based on the results of (Table 1), 70% of errors were in the category of care errors, 10% in the category of communication errors, 20% in the category of administrative errors, and 0% in the category of knowledge and skill errors; the categories were proposed by the association of NECM. In total, 38 reasons were detected for the adverse events of incompatible blood and blood transfusion in group discussion sessions. Table 2 represents the contribution of each factor with respect to 9 groups of contributing factors based on the UK National Health System model.
| Contributing Factors | Frequency (%) |
|---|---|
| Organization | 7 (18.4) |
| Task | 5 (13.2) |
| Patient | 3 (7.9) |
| Individual | 4 (10.5) |
| Communication | 4 (10.5) |
| Team | 4 (10.5) |
| Education and training | 5(13.2) |
| Equipment and resource | 2 (5.2) |
| Working condition | 4 (10.5) |
| Total | 38 (100) |
Frequency of contributing Factors in Adverse Events Related to Incompatible Blood Transfusion and Blood Products
Table 3 represents proposed the classification of strategies and preventive measures of adverse events.
| Strategy Classification | Frequency (%) |
|---|---|
| Human resources management | 7 (23) |
| Installation of the electronic prescribing system | 1 (3.3) |
| Making people accountable to patient’s safety | 1 (3.3) |
| Process standardization | 1 (3.3) |
| Improvement of the patient identification process | 3 (10) |
| Making clear policies | 4 (13.3) |
| Availability of suitable technology | 1 (3.3) |
| Continuous training | 1 (3.3) |
| Participating patients in the treatment process | 1 (3.3) |
| Monitoring suitable changes in clinical processes | 4 (13.3) |
| Promotion of communication | 2 (6.6) |
| Team work | 4 (13.3) |
| Total | 30 |
Classification of Strategies and Preventive Measures for the Causes of Adverse Events
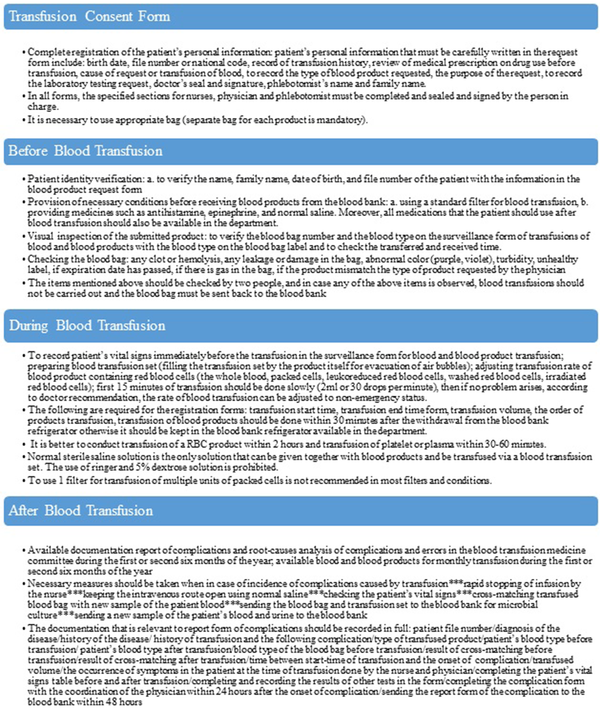
Given that in the present study, most strategies were related to the provision of instructions for the proper administration of blood transfusion process, and periodic training for the staff and because the introduction of advanced systems for the automatic transfusion of blood and blood products, such as an intelligent system for identification of the patients, is not economically feasible due to the lack of appropriate infrastructure in Iran; therefore, at the level of vice-chancellor for treatment, the instructions for transfusion management of blood and blood products in the two areas of “necessary measures before, during and after the transfusion of blood and blood products” and “the practice of haemovigilance among doctors” were compiled by the experts’ recommendation and was given to all subordinate units in order to prevent similar incidents (Figure 1).
5. Discussion
RCA is a structured approach to identify causes and determine the vulnerability of the systems (21). In this study, RCA techniques were used to analyze the adverse events related to blood and blood products and corrective measures taken to reduce similar events.
In a study by Tran et al., the highest errors were in the category of care (66%), communication (22%), administrative (6%), and knowledge (5%), respectively, which is in line with our findings (17). In addition, in a study by Molavi-Taleghani, which was carried out at an emergency department in one of the hospitals in Iran, the results showed that 62.3% of errors were in the category of care services, 13.8% in the category of communication, 15.7% in the category of administrative errors, and 8.1% in the category of knowledge and skill mistakes that is in line with our outcomes (22). On the other hand, in the present study, the greatest number of transfusion errors was related to a domain other than error analysis. This result is supported by the findings of a study in New York as well as a research done by the Commission on Accreditation of National Patient Safety (23).
In this study, the most common causes of error were organizational factors (18.4%), educational factors (13.2%), and duty factors (13.2%). The high rate of organizational factors suggests that in the incidence of adverse events, we cannot blame only the individuals because the weakness in the organization can also disrupt various work systems (24). Meanwhile, task problems are the guidelines, policies, and procedures that are absent, inaccessible, or unrevised (25). In the study by Sorra et al., the commonest reason for mistakes in blood transfusion was associated with the delay in service delivery (51%) and the disproportion between the delivery methods and instructions (49%), and given that the disproportion between delivery methods and instructions has been subordinate to duty factor in the model approved by the national organization of England, the results are consistent with of the present study (26). Considering the educational factors, it is important to note that due to the complex and competitive environment of today’s organizations, the managers of organizations and human resources should have a comprehensive understanding in this regard and try to reduce the errors related to educational factor through the empowerment of human resources. In their study, Butlers and Shi considered the inadequate knowledge of trainees and their insufficient education as potential causes of harm to patients (27).
Organizations often deal with issues by short-term solutions rather than deep-rooted analysis. Dependence on quick-fix solutions makes the organization’s resources repeat a specific mistake over and over again due to improper detection. The focus of the organizations on quick-fix solutions does not create profits but hinders the growth and prosperity of the organization. In the present study, most guidelines in the provision of instructions are related to the proper administration of the blood transfusion process and to the periodic training on blood and blood products. Linden et al. well documented the incidence of adverse events of the blood transfusion in the majority of health centers, and only educational programs as haemovigilance courses for the treatment staff and periodic training courses to promote the knowledge of the personnel about the management of blood products to prevent adverse events were reported necessary (23). Moreover, the accreditation commission has determined the instructions for correct verification of the patient in blood transfusion as their primary goal in the patient safety program (28) that is in line with our findings.
5.1. Conclusions
Generally, the incidence of similar adverse events in the future can be avoided by launching a mandatory error reporting system for the detection of system defects and the development and sharing of measures to improve system safety. Educating as well as investigating are needed to be applied as two critical instruments in optimizing the blood transfusion process. Finally, it should be noted that the systematic and constant application of risk management strategies plus the managers’ commitment and also studying the organizations’ policies are effective to ensure the beneficial effects of these activities.